Archive of Swine Flu Pandemic
Communication Updates
Archived Communication Updates Table of Contents
- June 29, 2010
- The “Fake Pandemic” Charge Goes Mainstream and WHO’s Credibility Nosedives
- January 17, 2010
- Pandemic Interruptus: It Ain’t Over Till It’s Over
- December 15, 2009
- What the CDC Is Saying about Swine Flu Severity
- December 15, 2009
- Update on the December 2 Update
- December 2, 2009
- It’s Official (sort of): The Swine Flu Pandemic Is Mild So Far
- November 18, 2009
- U.S. Pandemic Vaccine Supply and Distribution: Addressing the Outrage
- September 26, 2009
- Overselling Seasonal Flu Vaccination in a Pandemic Season
- August 21, 2009
- Talking about Pandemic H1N1 Vaccination
- July 21, 2009
- The Three-Legged Stool of Pandemic Messaging
En Français: Le tabouret à trois pattes de transmission de messages pour la pandémie
- July 7, 2009
- Why Pandemic Complacency Isn’t OkayEn Français: Pourquoi en cas de pandémie l’insouciance n’est-elle pas acceptable?
- June 17, 2009
- Would you like another wakeup call?En Français: Souhaiteriez-vous un autre appel de réveil?
- June 4, 2009
- Swine Flu Pandemic Prospects: Nobody Knows
- May 23, 2009
- Swine Flu Pandemic Prospects: Nobody Knows
- May 16, 2009
- Swine Flu Pandemic Prospects: Nobody Knows
- May 6, 2009
- Swine Flu Pandemic Prospects: Nobody Knows
- April 29, 2009
- Swine Flu Pandemic Scare Gets Serious
- April 28, 2009
- Swine Flu Pandemic Scare Gets Serious
- April 26, 2009
- Swine Flu Pandemic Scare Gets Serious
- April 24, 2009
- Swine Flu Pandemic Scare Gets Serious
June 29, 2010
The “Fake Pandemic” Charge Goes Mainstream
and WHO’s Credibility Nosedives
by Peter M. Sandman and Jody Lanard
 The last Swine Flu Pandemic Communication Update on this site was January 17 – five months ago. It made four points:
The last Swine Flu Pandemic Communication Update on this site was January 17 – five months ago. It made four points:
- We don’t know what’s coming next.
- It’s a real pandemic.
- It’s a mild pandemic, at least so far.
- It’s probably not over – but we don’t know what’s coming next.
That’s about it, really – still … except for the blame game, which is what we are going to analyze below. The extremely long assessment that follows advances an argument we can summarize in a single sentence:
The absurd charge that the World Health Organization (WHO) hyped a fake pandemic in order to enrich Big Pharma has gained undeserved mainstream credibility mostly because WHO has badly mishandled its risk communication about three issues: (a) the mildness of the pandemic (so far); (b) the debatable meaning of the term “influenza pandemic”; and (c) the inevitable – but not culpable – structural conflicts of interest of WHO advisors.
That’s where we’re going.
Where is the pandemic going? In January, swine flu incidence in the northern hemisphere had peaked and was decreasing in many countries, but was still widespread. Now, as summer approaches, it’s quite low. It’s quite low in the southern hemisphere too, but with somewhat higher levels reported in some tropical countries. Seasonal H3N2, the most severe of the seasonal strains, is still circulating at low levels. At this point, unfortunately, it does not appear to have been replaced by the pandemic virus.
In other words, there is no clear evidence yet that pandemic H1N1 is or is not going to “act” like a seasonal flu strain from now on, which is what former pandemic flu strains have done after 1–3 years. That’s certainly one of the possibilities, but there are two others. It could cause additional pandemic waves more or less like the ones it has already caused. Or it could get a lot more virulent – which most experts don’t expect at this point but don’t rule out either. (Experts do remember that the mild 1968 pandemic returned to cause a more severe European wave in the winter of 1969–1970, a full year after the very mild first European wave. Almost anything is possible with influenza.)
The pandemic is like a hurricane that initially and briefly looked like it might be a Category 4 whopper, turned out to be just barely a Category 1 hurricane – but still a hurricane – and then dissipated. But unlike a dissipated hurricane, the pandemic isn’t completely gone.
In our daily lives, though, the pandemic feels like it’s over, and for some people it feels like it never happened. Other than ongoing vigilance (surveillance and assessment), precautions are in abeyance in most of the world. The most expensive precaution, a new vaccine, wasn’t ready until after the 2009 northern and southern hemisphere waves were over or receding. Still, the vaccine could have prevented a lot of morbidity and some mortality if it had been ready sooner. And if the pandemic comes roaring back, many people will wish they had availed themselves of the vaccine they so disdained as the last wave receded.
Today, the only individuals continuing to take pandemic precautions are obsessed, and the only individuals complaining that we should never have taken precautions in the first place are ignorant.
As we write this in late June 2010, there is now a huge gap between WHO’s pandemic risk communication and the public’s pandemic risk perception. That is, what most people think they just lived through – a mild pandemic that has virtually disappeared – is radically different from what WHO tells them they are living through: a “moderate” pandemic that is still ongoing.
The result: Widespread skepticism about WHO’s credibility, and thus widespread receptiveness to previously fringe allegations.
“Widespread” is a relative term here. Most people pay virtually no attention to the World Health Organization. They didn’t realize it had a lot of credibility, and they didn’t notice when its credibility collapsed. And WHO’s most devoted followers – many of them public health professionals – have tended to rally round the organization in its hour of need. (Some of them have supported WHO publicly while muttering to each other that it really should stand down from some of its earlier pronouncements.)
But there’s a super-important group in the middle: people who don’t follow WHO closely but who do pay enough attention to have learned first that it seemed to be overstating the seriousness of the swine flu pandemic and then that it was accused of doing so on purpose to help Big Pharma make big bucks. That group includes many of the world’s opinion leaders: corporate executives, government officials, medical reporters, foundation heads, etc. Losing ground in their eyes matters for WHO, and may continue to matter for decades to come.
The collapse of WHO’s credibility is important not just in general because the world needs a credible international health agency, but also, in particular, because WHO’s pandemic warnings about the future (though not its status reports about the present) are right on target. H1N1 could mutate into a much deadlier virus. That would be unusual after a year, but not unprecedented. The world could also face another pandemic in the near future, caused by another novel flu virus. There was apparently a flu pandemic in 1830–31 and another in 1833. The 1968 pandemic started less than ten years after the 1957 pandemic ended. And of course all flu-watchers know that the extremely deadly H5N1 bird flu virus is still Out There. If bird flu ever starts transmitting easily from humans to humans, it’s a whole new ball game.
It is very hard for WHO to convince people – governments, journalists, ordinary citizens – to take the near-term pandemic risk seriously as long as WHO keeps describing the past year’s pandemic experience in ways they simply cannot take seriously.
The one-year anniversary of the identification of the new swine-origin H1N1 influenza virus came in late April, 2010. The media ran a lot of anniversary stories. Some health agencies issued anniversary news releases, often featuring “lessons learned” about what had gone well and not so well. The Center for Infectious Disease Research & Policy (CIDRAP) at the University of Minnesota did a whole series of anniversary stories. In preparation for one on communication lessons learned, Lisa Schnirring of CIDRAP sent us a list of questions. We dutifully wrote answers and posted them on this site.
The one-year anniversary of the World Health Organization’s (WHO) declaration of a full-fledged “Phase 6” pandemic was June 11, 2010. There were only a few anniversary stories.
This site’s Swine Flu Pandemic Communication Update about the Phase 6 declaration, posted on June 17, 2009, was entitled “Would you like another wakeup call?” It noted that: “For those who were already awake to pandemic realities and possibilities, [the WHO pandemic declaration] was basically a nonevent – a welcome if belated confirmation of what we knew.”
But in retrospect, the WHO pandemic declaration a year ago looks to many (though not to us) like a big mistake, or even an intentional deception. It was already pretty clear by mid-June 2009 that the pandemic was mild so far, more like the last two pandemics than like the nightmare possibility experts had warned about. But it was early days yet. It was perfectly possible that the pandemic could become much more virulent. (The first wave of 1918’s horrific pandemic was also mild.) Now, a year later, that possibility looks much slimmer. It can’t yet be ruled out; flu is famously unpredictable. But at this point it would be a big surprise. And so, with 20-20 hindsight, a lot of people think the initial pandemic declaration was unjustified.
Four things happened in early June 2010 that make this a compelling risk communication story, a fit but sad ending to the saga of Swine Flu Pandemic Risk Communication (Volume One).

WHO sticks to Phase 6.
On June 3, WHO Director-General Margaret Chan issued a statement summarizing the results of a June 1 teleconference meeting of the Emergency Committee that advises WHO on the H1N1 pandemic.
Dr. Chan said that “while pandemic activity is continuing, the period of most intense pandemic activity appears likely to have passed for many parts of the world.” That wasn’t sufficient, however, to persuade the committee to advise her to downgrade the pandemic to WHO’s “post-peak” phase, when “pandemic activity appears to be decreasing” but “it is uncertain if additional waves will occur.” All of the supporting data in the June 3 statement would seem to match the WHO definition of “post-peak,” but WHO did not stand down from Phase 6.
Nor did WHO seize the opportunity to stand down from its insistence that the H1N1 pandemic has been “moderate” so far, as opposed to “mild.”

The Council of Europe attacks WHO.
Also on June 3, the Parliamentary Assembly of the Council of Europe published an utterly bizarre report  reiterating charges that WHO had foisted on the public a fake pandemic, and had done so partly in order to enrich the pharmaceutical industry. To facilitate this deception, the report claimed, WHO changed its definition of the term “pandemic” and systematically avoided transparency and accountability mechanisms that would have publicly exposed the conflicts of interest that underlay the fraud.
reiterating charges that WHO had foisted on the public a fake pandemic, and had done so partly in order to enrich the pharmaceutical industry. To facilitate this deception, the report claimed, WHO changed its definition of the term “pandemic” and systematically avoided transparency and accountability mechanisms that would have publicly exposed the conflicts of interest that underlay the fraud.
The charges in the report were not unexpected, since they had been ventilated months earlier in public statements, a formal motion, and a hearing – at which WHO Special Advisor on Pandemic Influenza Keiji Fukuda was questioned. Still, publication of the report demonstrated Council support for the charges, even after hearing Dr. Fukuda’s defense. The Council of Europe isn’t part of the European Union; its decisions aren’t binding. But with 47 member states, it does influence public debate and sometimes future government decision-making.

BMJ joins the attack.
On the same day, BMJ (formerly the British Medical Journal) published an article charging that WHO committee members often have conflicts of interest that are not revealed to the public. The article was written jointly by the journal’s features editor and a journalist from the Bureau of Investigative Journalism, a nonprofit group launched on April 26, 2010, “to expose the exploitation of the weak by the strong” and “to reveal the failures of those in power to fulfill the trust placed in them.”
The article focused on three members of an earlier WHO committee that in 2004 had advised WHO to recommend large national pre-pandemic stockpiles of antiviral drugs. It pointed out some connections between those three committee members and the companies that manufacture and sell antivirals.
Publication of the BMJ article and the Council of Europe report was coordinated. On June 4 the principal author of the latter, Paul Flynn, posted on his blog: “One of the joys today was giving evidence with the editor of the splendid British Medical Journal. We have never met before but we cooed in harmony and just avoided saying it was the Pharmas that did it.”

WHO responds to its critics.
WHO responded to the charges in a June 8 open letter to BMJ, and again in a June 10 response to both organizations. It asserted that the pandemic was real, that the definition of a pandemic had not changed, and that WHO’s pandemic decision-making was completely uninfluenced by commercial interests. But it conceded that changes were needed in transparency policies regarding conflict of interest.
That’s the big swine flu risk communication story now, the biggest in months: In June 2010, the credibility of the World Health Organization crashed and burned. Charges that it had manufactured a fake pandemic in deference to the economic interests of Big Pharma gained mainstream attention.
These charges gained traction at this time, in our judgment, not because they are valid (they are not) but because WHO has badly mishandled certain aspects of its pandemic risk communications.
WHO has made three fundamental errors. In diminishing order of importance, they are:
- Failing to acknowledge that the pandemic has been mild overall, and that its incidence is now quite low. By “mild,” we mean similar to certain previous flu pandemics that WHO has long characterized as “mild” or “relatively mild.” By contrast, WHO has insisted on calling this pandemic “moderate” instead. And its tone has often left people feeling as if it were claiming “severe.”
- Failing to acknowledge that WHO changed some flu pandemic definitions and descriptions just as H1N1 was emerging. The technical meaning of the term “influenza pandemic” is debatable, as is the question of whether a mild flu pandemic should be called a pandemic at all. When WHO changed some of its definitions and descriptions of flu pandemic phases in ways that de-emphasized severity, it opened the door to suspicion that it had “changed the definition of a pandemic” in order to make sure H1N1 would qualify.
- Failing to acknowledge – until June 2010 – that WHO transparency about conflicts of interest had become inadequate. WHO’s earlier response to conflict-of-interest charges was to explain its policies and offer reassurance that the policies work. It wasn’t until after the two recent attacks that WHO began to concede that in the face of the public’s profound loss of trust, it may need to be both tougher and more transparent about its expert advisors’ conflicts of interest.
We must immediately concede that “failing to acknowledge” in these three bullet points is an overstatement. In their millions of words about the swine flu pandemic, WHO officials have periodically made statements that can be read as acknowledging all the points we’re accusing them of failing to acknowledge. We would be on safer ground claiming that WHO officials have failed to get these acknowledgments across. But that would imply that they were trying to do so. They weren’t. The main thrust of WHO pandemic communications has been, and continues to be, that H1N1 is a pandemic of moderate intensity that requires a continued “Phase 6” response; that H1N1 unambiguously meets the consensus definition of an influenza pandemic which has not been changed; and that WHO deliberations about how to manage H1N1 have been sufficiently transparent and self-evidently free of dangerous conflicts of interest.
That, we believe, is why WHO’s credibility is seriously threatened, and its ability to warn the world about future pandemic threats seriously compromised.
To understand what is behind the serious recent damage to WHO credibility, we are going examine these three failures in detail.
Such a detailed examination is worthwhile, we think, for two reasons:
- First, we hope to make a contribution to the world’s understanding, and to WHO’s understanding, of what happened – of how the World Health Organization managed to do severe damage to its own credibility – not by the way it handled the technical side of the twenty-first century’s first influenza pandemic (it did a creditable job), but by the way it handled its risk communication during that pandemic. WHO has appointed an external review committee
 chaired by Dr. Harvey Fineberg to assess the “Functioning of the International Health Regulations (2005) in Relation to Pandemic (H1N1) 2009.” We hope this long column will help Dr. Fineberg’s committee see the pivotal role risk communication has played in WHO’s pandemic credibility crisis.
chaired by Dr. Harvey Fineberg to assess the “Functioning of the International Health Regulations (2005) in Relation to Pandemic (H1N1) 2009.” We hope this long column will help Dr. Fineberg’s committee see the pivotal role risk communication has played in WHO’s pandemic credibility crisis.
- Second, we believe we are writing not just about what happened, but also about what happens. The H1N1 pandemic is not the only time WHO’s top scientists’ inattention to risk communication has been its Achilles heel, and WHO is not the only organization that has been damaged by its technical leaders’ inattention to risk communication. Many of the more specific phenomena discussed in this article – for example, WHO’s reluctance to make changes that might be seen as caving in to pressure – are also generic. We hope readers who don’t share our longstanding fascination with the World Health Organization and with influenza pandemics will nevertheless find parts of this analysis illuminating.
For readers who don’t want to delve that deep, we hope the foregoing introduction will have been of interest. For the remainder of this lengthy analysis, use the following links:
Complete Column Table of Contents
January 17, 2010
Pandemic Interruptus: It Ain’t Over Till It’s Over
by Peter M. Sandman
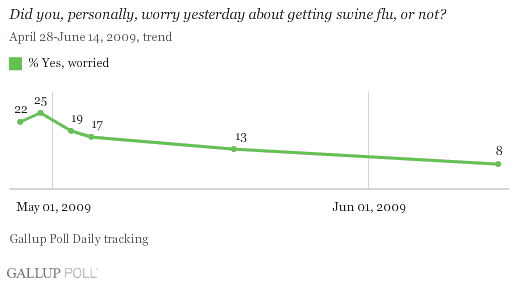
What should pandemic risk communicators be saying in January 2010, when swine flu looks to non-experts like it’s disappearing, when swine flu vaccine is a drug on the market, and when swine flu news has taken on a distinctly skeptical tone?
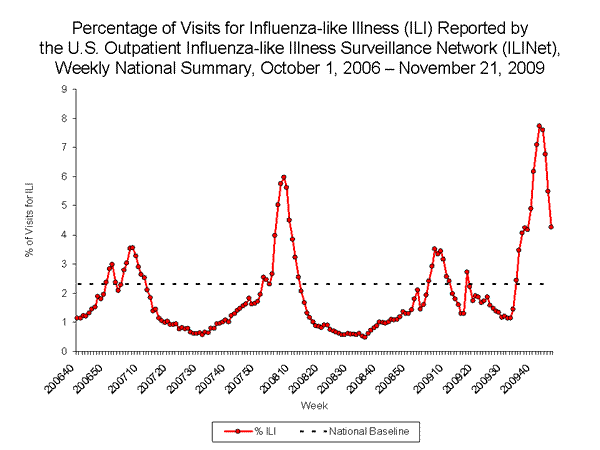
It has been a wild ride so far, from high drama to bored skepticism in a mere nine months. The novel H1N1 influenza virus was first identified in samples from two U.S. children in mid-April 2009, and then a week later in samples from Mexico. April is a month when there’s normally very little flu in the northern hemisphere. From April through December, the U.S. had more flu than in the average flu season. In most of the country, but not all, we saw a first wave in the spring, then a summer decline (but still much more flu than usual in summer), and then a bigger second wave in the fall. Then the fall wave plummeted.
By mid-January in most years, seasonal flu numbers are increasing in the U.S. But in this pandemic year, the pandemic flu numbers are decreasing, and there is virtually no seasonal flu around yet. The same thing is happening in most of Europe. Pandemic H1N1 is way down, and except for a few isolated cases seasonal flu has yet to appear.
Naturally the media have virtually decreed the pandemic over. And some commentators have said, in hindsight, that it wasn’t a pandemic at all.
In the ecosystem of public opinion, all niches are filled. At one extreme are those who confidently predicted a rerun of 1918 or worse, some of whom even now maintain that it happened and health officials somehow managed to cover it up. At the other extreme are those like Marc Siegel and Michael Fumento who were pandemic scoffers from the outset and are now crowing that they were right all along.
Many in the media have happily oscillated from one extreme to the other. Some of the newspapers and broadcast stations that headlined the direst predictions now headline preposterous charges that it was a “false pandemic” manufactured by a conspiracy of public health officials and pharmaceutical companies.
Okay, so what should pandemic risk communicators be saying?
1. We don’t know what’s coming next.
 Although people with normal interests may think of flu as ordinary and boring, public health experts see influenza as endlessly surprising, among the most fascinating of diseases. And influenza is never more surprising than when a new flu virus emerges and launches a pandemic.
Although people with normal interests may think of flu as ordinary and boring, public health experts see influenza as endlessly surprising, among the most fascinating of diseases. And influenza is never more surprising than when a new flu virus emerges and launches a pandemic.
Experts see flu as unusually unpredictable – but considerable unpredictability is a hallmark of nearly all crisis situations. That’s why acknowledging uncertainty  is a core principle of crisis communication.
is a core principle of crisis communication.
The only sensible way to plan pandemic response – and the only sensible way to talk about pandemic planning – is probabilistically. We don’t know what’s next, but we can estimate probabilities and act accordingly.
Probabilistic thinking is the very essence of risk assessment and therefore of risk management. And probabilistic language is an essential part of risk communication.
Thinking and talking probabilistically about risk requires asking six core questions:
- What outcomes are possible?
- What is the estimated probability of each possible outcome? (No one can really know, but experts can make informed guesses.)
- What are the predicted effects of each possible outcome, and how bad is each set of effects? (This can be modeled.)
- What can be done, at what cost, to mitigate each set of effects? (This can be modeled too.)
- How confident are we about the answers to these questions? (Not very.) What are we likeliest to be wrong about? In which direction?
- Based on all of that, what does it make sense to do? (This will be a debatable judgment based partly on values and partly on the guesses and modeling above.)
It doesn’t follow that the wisest course of action is to prepare only for the likeliest set of outcomes. Dire outcomes justify preparedness (if preparedness is possible and cost-effective) even if they’re pretty unlikely. That’s why people buy fire insurance for their homes – not because a big fire is the likeliest outcome, but because it’s a very bad outcome that isn’t vanishingly unlikely.
Inevitably, then, a lot of preparedness will turn out unnecessary or excessive. When your home doesn’t burn down, you don’t cancel your insurance, nor are you angry that you wasted your premium. You’re glad your home didn’t burn down last year, and also glad you’re insured in case it burns down this year.
And fire insurance salespeople don’t claim that their prospective customers’ homes are going to burn down. They ground their sales pitch not in the probability of such a disaster, but in its magnitude. They’re selling a hedge to lessen the impact of a profoundly undesirable scenario – one that is pretty unlikely, but not so unlikely as to constitute a negligible risk. And they’re selling the peace of mind that comes with knowing you have hedged against such a possible disaster.
What’s missing from most people’s pandemic thinking is this probabilistic mindset.
Sports fans think probabilistically. Baseball fans, for example, know that there are times when the smartest thing for a batter to do is try to bunt the runner into scoring position. If the strategy doesn’t pan out, a commentator may remark that the batter probably wishes in hindsight that he’d swung for the fences … but nobody says he should have done so when the odds said bunting was the right bet. There are obvious analogues in virtually every sport: The right play remains the right play even when it didn’t work this time.
Similarly, we all understand that weather forecasters play the odds, and advise us to play the odds. When there’s a 70 percent chance of rain we take an umbrella to work and cancel our picnic plans – and we’re not especially outraged if the sun shines all day. When there’s even a 20 percent chance of a hurricane we buy extra food and check the flashlight batteries – and we feel neither foolish nor victimized if the hurricane weakens or changes course.
But in public health, non-experts often indulge in outcome-biased thinking instead of probabilistic thinking. Thus many people – and many journalists and politicians – seem to believe that officials should have prepared for exactly the pandemic we got (so far), no more, no less … as if they could have known in advance what sort of pandemic would come along.
If the 2009 pandemic had turned out as severe as it looked last April in Mexico, Congress would long since have launched investigations into why the CDC was insufficiently prepared, why we let our public health infrastructure decay, etc. If we end up with a severe third wave, those same questions will be asked. Even the mild pandemic we have had so far was sufficient for “tough questions” about the slow pace of vaccine production. But since the pandemic looks like it’s over (for now) and since it wasn’t very bad (for most people), many are asking instead why public health officials scared us unnecessarily.
I’m not going to burden readers with endless quotations from commentators and critics in the U.S., Europe, India, and elsewhere. They’re all grounded in the same false reasoning:
- Officials warned us that things might get really bad, and urged us to take precautions.
- Things didn’t get that bad (at least not yet). Those who took precautions feel foolish. Those who didn’t take precautions feel vindicated.
- Officials must have known that things wouldn’t get that bad. They misled us on purpose. Here’s why they did it….
Outcome-biased thinking isn’t confined to public health. Consider three other examples.
- After hurricane Katrina, most people came to believe in hindsight that the government should have done more to enable the New Orleans system of levees to withstand heavy floods in a strong hurricane. They didn’t think so beforehand, and they still don’t want to retrofit other cities against other catastrophes. There’s not much demand to prepare New York City for a tsunami or the New Madrid Fault region for an earthquake. Just New Orleans for a hurricane.
- After the financial system imploded in 2008-2009, just about everyone agreed that there should have been tougher regulation of credit default swaps, securitized mortgages, and whatever else needed regulating in order to keep the economy on track. Not that we wanted more government regulation at the time. Nor do we want more government regulation now … except for regulating whatever caused the economy to tank last year.
- After the Christmas Day bomb attempt on Northwest Airlines Flight 253, a near-consensus emerged that the government should have seen it coming and stopped Umar Farouk Abdulmutallab from getting onto the plane. Does that mean we want all people put on the no-fly list if they’re from countries with significant Muslim populations and their fathers think they’re too radical? Nope – just Abdulmutallab and everyone else who’s going to try to blow up a plane.
I’m not asserting that it’s a bad idea to spend more money preparing urban areas for natural disasters, or to regulate financial institutions and especially innovative financial instruments more strictly, or to be more rigorous in the screening of international air travelers. There are pros and cons to each of these measures. And there are counterexamples – horror stories of money spent preparing for natural disasters that never came, of industries that seem unable to compete and innovate effectively because of over-regulation, of innocent people who have struggled unsuccessfully to persuade officials to take them off the no-fly list.
My point is that you can’t prepare only for a hurricane in New Orleans, regulate only the industries that are about to implode, and keep only the actual terrorists from flying. And you can’t get people all worked up about only the pandemics that are going to turn out to have been severe.
You can be as risk-averse or as risk-tolerant as you want in how you play the odds. But you can’t avoid playing the odds.
In all these examples where post-hoc outcome-biased thinking prevailed over real-time probabilistic thinking, the situation was scary enough that many people felt powerless and vulnerable. Sometimes a degree of psychological regression happens when people feel powerless and vulnerable. We get childish and petulant. Like children, we want mommy and daddy to make it right.
So if something bad happens, we complain bitterly that mommy and daddy should have protected us better. And if something bad doesn’t happen, we complain nearly as bitterly that mommy and daddy shouldn’t have disrupted our playtime with unnecessary warnings and precautions.
These examples have something else in common. Discussions of sports and weather refer constantly to playing the odds – but discussions of emergency preparedness, government regulation, counterterrorism, and pandemic response do not.
Early on in the pandemic, public health officials should have been saying – again and again – something like this:
We don’t know how severe this pandemic is going to be. Yet we have to make decisions now – for example, decisions about how much vaccine to order, and decisions about whether to advise closing schools and canceling public events. So some of these decisions may end up wrong. We are trying to err on the alarming side. We’d rather prepare too much than too little. But if things get very bad, critics will say that we should have done more – and in hindsight they will be right. And if the pandemic turns out mild, critics will say that we should have done less – and in hindsight they will be right too.
Officials did say things like this from time to time. At the very start of the CDC’s second pandemic press briefing on April 24, Richard Besser (then acting director) put it superbly:
First I want to recognize that people are concerned about this situation. We hear from the public and from others about their concern, and we are worried, as well. Our concern has grown since yesterday in light of what we’ve learned since then.
I want to acknowledge the importance of uncertainty. At the early stages of an outbreak, there’s much uncertainty, and probably more than everyone would like. Our guidelines and advice our [are] likely to be interim and fluid, subject to change as we learn more….
We do not know whether this swine flu virus or some other influenza virus will lead to the next pandemic; however, scientists around the world continue to monitor the virus and take its threat seriously.
Media coverage of the Besser press briefing was substantial, but very few stories quoted this passage. Reporters went for the hard news: what the CDC thought was happening and what it was going to do about it. “Uncertainty claims” – explicit statements that the situation is uncertain, that officials are playing the odds, and that in hindsight their response may turn out too aggressive or not aggressive enough – are hard to get into the media. Officials almost always end up sounding more certain in news stories than they sounded during the news conference or the interview.
Later on, commentators who missed the qualifiers and uncertainty claims write, “Remember when they said we were all gonna die?”
Even if uncertainty claims make it into the media, they are hard to get into people’s heads – especially the heads of people who feel powerless and vulnerable, who want officials to be confident and definite.
And of course most officials are less committed than Dr. Besser was to communicating their uncertainty. Especially in crisis situations, it’s awfully tempting to project certainty instead (as if that were a stand-in for competence) – to give the anxious public what it seems to want.
But nothing is more important in pandemic risk communication than persuading the public (and the politicians) to think probabilistically. Public health officials need to insist on their uncertainty; they need to make uncertainty the message, not the preamble to the message.
Uncertainty about the future should have been stressed, over and over, early on in the pandemic – far more than it was. But maybe we’re still “early on” in the pandemic. As Yogi Berra (a probabilistic thinker) taught us, it ain’t over till it’s over. So probabilistic thinking should be stressed now as well – both about the decisions that have been made up till now, and about the decisions we face today.
As the 1957 Asian Flu pandemic was looming from a distance, the U.S. Surgeon General at the time, Leroy Burney, said:
I am sure that what any of us do, we will be criticized either for doing too much or for doing too little…. If an epidemic does not occur, we will be glad. If it does, then I hope we can say… that we have done everything and made every preparation possible to do the best job within the limits of available scientific knowledge and administrative procedure.
I doubt that it’s ever advisable to make “every preparation possible.” But Burney’s first sentence is right on target.
Uncertainty is Message #1.
2. It’s a real pandemic.
 After many weeks of information-gathering, discussions with Member States, and expert debate, the World Health Organization (WHO) declared the swine flu outbreak a pandemic on June 11, 2009. In January 2010, some commentators are trying to “undeclare” it.
After many weeks of information-gathering, discussions with Member States, and expert debate, the World Health Organization (WHO) declared the swine flu outbreak a pandemic on June 11, 2009. In January 2010, some commentators are trying to “undeclare” it.
They’re wrong. It’s a real pandemic.
Like a lot of terms in public health, the word “pandemic” isn’t rigorously defined. But there is general agreement that an influenza pandemic has three defining characteristics.

A flu pandemic has to involve a novel influenza virus.
The flu virus that launches a pandemic must be different from other flu viruses that have circulated among humans in recent years. This means that most of the population will have no significant pre-existing immunity from past exposure to the flu, or to the flu vaccine.
Although “novel” is a matter of degree, virtually all flu experts agree that the H1N1 virus that emerged last April is novel enough. It is very different from the H1N1 virus that was responsible for the 1918 pandemic. That earlier H1N1 gradually became the seasonal influenza A virus in the years after 1918 (it may also have been a seasonal strain for about ten years before it became a dreadfully virulent pandemic strain); then H1N1 was supplanted by a different influenza A virus after the pandemic of 1957; then it re-emerged (most experts think because of a laboratory accident) and became seasonal again in 1977; it has been circulating seasonally ever since. The fact that both viruses are classified as A(H1N1) viruses doesn’t make them close relatives.
There was some discussion early on that older people might have some cross-immunity from exposure to the other H1N1 before 1957. This question is still being researched. But U.S. data show that people born before 1957 have a swine flu population mortality rate at least as high as people born after 1957.

A flu pandemic has to be widespread.
The “pan-” in “pandemic” is Greek for “all,” while “-demic” comes from “demos,” Greek for “people.” A disease outbreak doesn’t literally need to threaten “all people” to qualify as a pandemic, but there does need to be a large number of cases in a large number of age groups in a large number of places.
How many cases in how many age groups in how many places is, once again, subjective and debatable. But nobody seriously argues that 2009 H1N1 hasn’t been widespread enough.
What enables a pandemic to become widespread is its ability to transmit efficiently from one person to another. Once health officials determine that an influenza virus has mastered efficient human-to-human transmission, they know the virus will soon be widespread.

-
A flu pandemic has to cause serious illness.
A novel flu virus that infected hundreds of millions of people all over the world still probably wouldn’t end up labeled a pandemic virus if it caused mostly mild illness and no excess mortality in any age group. Flu experts would certainly watch it closely in case that pattern started to change. Officials might even declare a pandemic early on, before the severity level was known. But if it’s not a serious health threat at least to some groups of people, then it’s not a flu pandemic.
This is the criterion that’s most controversial with regard to the 2009 pandemic. Throughout this pandemic, and especially lately in Europe, there has been a lot of scoffing that officials were scare-mongering, expending huge amounts of resources on a “false” pandemic.
On the one hand, millions of people in the U.S. alone have been sick enough to feel truly rotten, and around 11,000 of them have died – far more of them under age 65 than in an average flu season. That’s excess mortality in certain age groups. And more people with swine flu have ended up in hospital intensive care units than during an average flu season. On the other hand, so far the 2009 pandemic has killed fewer people than the three flu pandemics of the twentieth century, which started in 1918, 1957, and 1968. So far, in fact, it has killed fewer people than many ordinary flu seasons, and its overall case fatality rate (the percentage of sick people who die) is much lower than the average seasonal flu case fatality rate.
But as a group of prominent influenza experts put it:
[P]andemics, like interpandemic influenza seasons, vary in severity, by the age groups most affected, the size of the populations affected and in their length. Therefore, it cannot be assumed a priori that pandemics will cause more mortality than interpandemic seasons.
For example, some flu seasons since the 1968 pandemic have been deadlier than that pandemic, partly because of the aging of the population since then, but also because of the increased virulence of the seasonal strain A(H3N2), which was originally the novel virus that caused the 1968 pandemic.
There’s a very practical argument against considering the 2009 pandemic too mild to count: Officials need to announce pandemics early so societies will know to ramp up their preparedness. It makes sense to wait until it’s clear that a novel flu virus is capable of causing serious illness. But waiting until the ultimate case fatality rate is known would mean declaring pandemics only after they’re over … which would defeat the purpose of declaring pandemics in the first place.
Keep in mind that 2009 was the world’s first experience with a pandemic declaration so close to the start of an actual pandemic. It is a sign of stunning progress since 1968.
Experts continue to debate the close cases. The Russian Flu of 1977 is a good example. It was caused by the re-emergence (probably from a lab) of a 1950 strain of human H1N1, and it quickly spread globally. But it mostly affected people younger than age 23 – people who hadn’t been around when that strain was circulating previously. And it did not cause excess mortality in any age group. A few experts consider the Russian Flu to have been a pandemic, but most do not.
In 1995, influenza expert Edwin D. Kilbourne said that “defining a pandemic is a little like defining pornography – we all ‘know it when we see it,’ but the boundaries are a little blurred.” Dr. Kilbourne’s wonderfully readable article discusses several examples of such blurriness, especially regarding the concept of a “novel” virus.
If worldwide disease surveillance had been good enough in 1977 to identify the Russian Flu outbreak at its inception, it might have been declared a pandemic – and then “undeclared” when more was known. But it would take a very fringe expert indeed to recommend “undeclaring” the H1N1 pandemic of 2009.
3. It’s a mild pandemic, at least so far.
 Sometimes it seems like the world (the world of people interested in flu, at least) is divided into two camps: the people who think swine flu is too mild to call it a pandemic versus the people who think it’s a pandemic and how dare anyone call it mild!
Sometimes it seems like the world (the world of people interested in flu, at least) is divided into two camps: the people who think swine flu is too mild to call it a pandemic versus the people who think it’s a pandemic and how dare anyone call it mild!
I’m in the third camp, which feels like the smallest camp: the people who keep insisting that it’s a mild pandemic so far.
It’s certainly not – so far – the pandemic that health officials were expecting and dreading. That expectation was shaped by two anchoring frames.
The first standard of comparison is the pandemic of 1918, the most severe pandemic of modern times. The 1918 pandemic is estimated to have killed about 675,000 Americans – virtually all within a single year, though the pandemic actually lasted 27 months. Its case fatality rate in the U.S. was roughly 2% – compared to roughly 0.02% for the 2009 pandemic so far, about a hundred times lower.
The second standard of comparison is the incredibly deadly novel H5N1 (“bird flu”) virus that emerged in 1997. Bird flu has not gone pandemic (so far); it has infected fewer than a thousand people worldwide. But it killed nearly 60 percent of them – a case fatality rate 30 times worse than the 1918 pandemic, and 3,000 times worse than the 2009 pandemic so far. The nightmare that influenza experts have been living with since 1997, and are still living with today, is that bird flu will mutate in a way that makes it as transmissible as ordinary flu (or as swine flu), only thousands of times deadlier.
Flu experts prepared for the 2009 pandemic in the shadows of 1918 and bird flu. They shied away from the most horrific possibilities, but they never even considered the mildest possibilities.
U.S. experts, for example, developed a Pandemic Severity Index  (PSI) that had five categories. The PSI assumed that a pandemic would infect about 30 percent of the U.S. population. A Category 1 pandemic would have a case fatality rate of less than 0.1%, adding no more than 90,000 U.S. fatalities – still more than twice as bad as the average flu season. A Category 5 pandemic would have a case fatality rate of greater than 2 percent, meaning more than 1,800,000 U.S. fatalities – basically a rerun of 1918 or worse, with a much larger population. A bird flu pandemic would be off the scale in one direction. The swine flu pandemic we got is off the scale in the other direction … which may be why officials haven’t mentioned their PSI in quite some time.
(PSI) that had five categories. The PSI assumed that a pandemic would infect about 30 percent of the U.S. population. A Category 1 pandemic would have a case fatality rate of less than 0.1%, adding no more than 90,000 U.S. fatalities – still more than twice as bad as the average flu season. A Category 5 pandemic would have a case fatality rate of greater than 2 percent, meaning more than 1,800,000 U.S. fatalities – basically a rerun of 1918 or worse, with a much larger population. A bird flu pandemic would be off the scale in one direction. The swine flu pandemic we got is off the scale in the other direction … which may be why officials haven’t mentioned their PSI in quite some time.
I have been describing the swine flu pandemic as “mild” since before it was declared a pandemic – almost always adding the crucial qualifier: “so far.” I based my use of the word “mild” on evolving published data about this pandemic, compared to prior pandemics and average flu seasons, not on my own non-existent influenza expertise.
On May 6, I wrote: “Swine flu looks to be an extremely mild pandemic if it goes pandemic at all, despite WHO warnings that it may ‘come back with a vengeance’ in the fall.” On June 4, I wrote that it was “still mild.” On June 17, I wrote: “The big public health risk isn’t the relatively mild flu that’s circulating now…. Swine flu could come roaring back in a much more virulent second wave.” On July 21, I proposed three core pandemic messages. One was: “Pandemic H1N1 looks very mild so far.” Another was: “We must prepare for the possibility that pandemic H1N1 could become more severe.”
I kept arguing that a communicator who failed to acknowledge the current mildness of the pandemic could not credibly warn about its possible future severity.
Finally, on December 2, I entitled my Swine Flu Pandemic Communication Update: “It’s Official (sort of): The Swine Flu Pandemic Is Mild So Far.” The CDC’s own data showed the mildness of the pandemic, I said, and the CDC was unwisely refusing to say so.
This time I was criticized for insisting so aggressively on the pandemic’s mildness. (See my December 15 acknowledgment of this criticism.) I understand some of the reasons why the term “mild” strikes many as offensive:
- It is insensitive to the impact of the pandemic on those who lost a loved one to H1N1, or were severely ill, or even just worked 90-hour week after 90-hour week in a local health department.
- It ignores the reality that the pandemic has already killed several times as many children as the average flu season. (The average flu season kills mostly the elderly.) That’s a fact that has understandably and justifiably worried many parents, and left them feeling that the pandemic was anything but mild.
- It also ignores the reality that many more people under 65 were hospitalized and in intensive care units during the 2009 pandemic than during the average flu season. Often concentrated over a short period of time in specific “hot spots” around the country, these hospitalizations constituted an unusual burden on the U.S. medical system.
- It focuses on one aspect of pandemic severity, the number of deaths. But pervasiveness matters too. My college professor daughter, for example, says more of her students were out sick with the flu last fall than any semester in her memory. As far as she knows, none of them died. But she certainly experienced the fall as a severe flu season.
Despite all of that, the fact remains that in terms of overall mortality the 2009 pandemic has been very mild so far – so mild that some are denying that it’s a pandemic at all. The time has come for officials to acknowledge and insist on the middle ground. Yes, it’s a pandemic – so far a mild one overall, albeit tragic for tens of thousands of people around the world.
In fact, official acknowledgment of the pandemic’s mildness is long overdue. Both the CDC and the World Health Organization have steadfastly avoided the word “mild” in their pandemic communications. Both have passed up many chances to breathe an audible sigh of relief: when the alarming initial news from Mexico was not borne out, when the pandemic case fatality rate came in lower than the rate of prior pandemics and lower than the rate of the average flu season, etc. Both have seldom said publicly what I think they must be saying privately: “So far, so good. We’re not out of the woods yet, and the pandemic could still take a turn for the worse, but to date it has been much less devastating than we dared hope.”
In part because of their failure to acknowledge the pandemic’s mildness, officials are now reaping the whirlwind. Millions of ordinary citizens have seen for themselves that (with tragic exceptions) this pandemic is not such a big deal. If the CDC and WHO think otherwise, if what we have experienced over the past nine months is really the sort of pandemic health officials consider serious, then it makes sense to shrug off their pandemic warnings altogether.
Officials’ failure to acknowledge that the pandemic has been mild so far thus justifies public skepticism about officials’ warnings that this pandemic or some future pandemic could be far more severe. It even gives a semblance of credence to the absurd allegation that officials have been promoting a fake pandemic for ulterior purposes.
It’s a real pandemic, but so far a mild one. Officials need to say so.
4. It’s probably not over – but we don’t know what’s coming next.
 I’m not a virologist, and I’m not entitled to an opinion about where the 2009 pandemic is headed in 2010. In fact, many virologists think they’re not entitled to an opinion either. They say it’s anybody’s guess.
I’m not a virologist, and I’m not entitled to an opinion about where the 2009 pandemic is headed in 2010. In fact, many virologists think they’re not entitled to an opinion either. They say it’s anybody’s guess.
The least likely possibility, I’m told, is that swine flu will simply disappear. Influenza is such an unpredictable disease that the experts aren’t ruling anything out, not even that. But the H1N1 virus transmits easily from person to person. And it has lots of people left to infect – people who have neither had the disease nor been vaccinated against it. So most experts expect to see more swine flu.
One question is when swine flu will surge again in the U.S. (It hasn’t disappeared. It is still circulating in low levels here, and at higher levels in some countries around the world.) There are three main possibilities:

- There could be a third pandemic wave soon – this winter, in fact. Some experts think that’s very likely, and none would find it surprising. But most countries in the southern hemisphere had a quick, steep, late-fall/early-winter pandemic first wave very much like our second wave … and have seen little or no swine flu since then. So maybe we’re done for this season.

- There could be a delayed pandemic third wave – in the coming spring, summer, or fall; or maybe not till the weather turns cold again next winter. Other pandemics have seen troughs of many months before a new wave, so it wouldn’t be a surprise if that happened again.

- Novel H1N1 could return not as a third pandemic wave but as a no-longer-novel seasonal influenza strain. Once pandemic flu viruses have run their pandemic course, they usually have a second life as seasonal strains. The last three pandemic strains supplanted the seasonal influenza A strain that had been circulating before the pandemic strain emerged. The distinction between a pandemic wave and a flu season with a new strain is a bit arbitrary. But sooner or later the pandemic swine flu virus is expected to turn into a seasonal influenza A strain – maybe even the only seasonal influenza A strain.
A more important question than when swine flu will resurge is how the novel H1N1 virus might change along the way. The scariest possibility is that it could become more virulent, mutating in a way that makes it much less mild. One nightmare scenario: Swine flu and bird flu mix-and-match genetic material, producing a new virus as infectious as swine flu and as deadly as bird flu.
All changes are possible. The swine flu virus could become more or less virulent. It could become more or less infectious. It could attack different age groups or people with different medical conditions. It could become resistant to antiviral drugs. It could (and almost certainly will, over time) drift genetically so the existing vaccine no longer works very well.
Or, of course, it could stay pretty much the way it is – with more and more people becoming immune to it as a result of previous exposure or vaccination. Influenza strains mutate incessantly, so “staying the same” is considered a pretty unlikely scenario. But as the experts all say, the only thing you can be sure of with influenza is that it will surprise you. Staying the same is one possible surprise.
And here’s yet another question: What’s going to happen to the seasonal flu strains? Precedent says one or both of the currently circulating influenza A strains will probably disappear, supplanted by the new flu in town. But that’s not guaranteed either.
If the U.S. is going to have its usual flu season this winter, it’s already a little late … but not yet ridiculously late. So:
- Maybe we’ll see no more pandemic flu this winter, but the seasonal flu will come back as usual.
- Maybe we’ll have to endure both simultaneously – a pandemic third wave plus the usual flu season.
- Maybe the previous seasonal influenza A strains will disappear for good, and swine flu will be our new seasonal influenza A until the next pandemic.
If swine flu does supplant the earlier seasonal A strains (whether it happens this winter or a year or two from now), that could be very good news, especially for seniors. In recent years seasonal influenza has been made up of two influenza A strains: H3N2 (still circulating since it caused the 1968 pandemic) and the 1977 version of H1N1. (There are also two kinds of influenza B in circulation. Influenza B doesn’t seem to compete with influenza A strains, and isn’t known to cause pandemics.) H3N2 is currently the deadlier of the two A strains, especially to the elderly. If H3N2 gets wiped out, and if pandemic H1N1 becomes seasonal and stays as mild as it is so far, we’re unlikely to reach our annual average of 36,000 U.S. flu deaths in the coming years.
In other words, by out-competing and replacing the deadlier seasonal strains (especially H3N2), the 2009 pandemic could end up saving lives!
Like everything else about influenza, this isn’t guaranteed either. Maybe swine flu will end up coexisting with one or both of the two seasonal influenza A strains that have been circulating since 1968 and 1977. Maybe it will supplant those earlier strains but become deadlier itself (just as H3N2 is deadlier today than it was during the pandemic of 1968).
Or maybe swine flu will disappear after all, leaving us back where we started.
Key Messages
So what are the key messages of the moment about the swine flu pandemic? I think there are four.

Like you, we don’t know what’s going to happen next either.
Flu pandemics are unpredictable. From the beginning, we have had to prepare for a wide range of possibilities – and we still do. We will continue to err on the alarming side, convinced that it’s better to over-prepare than to under-prepare, until we are sure the pandemic is over.

We probably haven’t seen the last of swine flu.
It may come back soon, or not for many months. It may come back as a pandemic third wave, or as a new seasonal strain. Either way, getting vaccinated now against swine flu is a sensible precaution.

So far the pandemic has been mild.
It sure didn’t feel that way if you were among its victims, or their families and friends. But the truth is, we were lucky (most of us). This isn’t the pandemic that health officials were worried about, at least not yet. It’s a real pandemic, and it has killed way more children than the average seasonal flu. But overall, it is less deadly so far than the average seasonal flu.

-
We may still face the pandemic officials were worried about.
Swine flu could mutate to become more severe. A new, worse pandemic could emerge – maybe bird flu; maybe something completely new. What has happened already is a tragedy for many people. But it is a practice run for all of us – not a false alarm – and we should see it that way.
December 15, 2009
What the CDC Is Saying about Swine Flu Severity
- How deadly is the pandemic so far?
- What age groups is it hitting hardest?
- What age groups does the government say it is hitting hardest?
by Peter M. Sandman
 This update draws some inescapable tentative conclusions from the most recent (December 10) tentative estimates of U.S. pandemic flu cases, hospitalizations, and deaths provided by the U.S. Centers for Disease Control and Prevention (CDC).
This update draws some inescapable tentative conclusions from the most recent (December 10) tentative estimates of U.S. pandemic flu cases, hospitalizations, and deaths provided by the U.S. Centers for Disease Control and Prevention (CDC).
On January 15, 2010, the CDC updated its estimates of U.S. swine flu cases, hospitalizations, and deaths to cover the period through December 12, 2009 – pretty much finishing out the second wave of the pandemic.
The additional month of data didn’t increase the numbers much, and didn’t change their implications at all. Everything in my December 15 update (which discussed the CDC’s December 10 report on data through November 14) applies equally to the CDC’s January 15 report.
But of course the exact numbers in this update are now out of date. Readers should feel free to do their own arithmetic to calculate updated case attack rates, case fatality rates, population mortality rates, etc., for each of the three age groups. It’s not that hard; just use this December 15 update as a template.
Note that the CDC webpage to which this update periodically links – http://www.cdc.gov/h1n1flu/estimates_2009_h1n1.htm – now provides the CDC data through December 10. This is apparently going to remain the “evergreen” URL for the latest CDC estimate of swine flu cases, hospitalizations, and deaths (assuming there’s enough additional swine flu to justify any further reports). But the CDC has kept its earlier reports posted as well, with links from the evergreen page. The estimates on which this December 15 update was based are now at http://www.cdc.gov/h1n1flu/estimates/April_November_14.htm.
(Added: January 16, 2010)
The update also contrasts the CDC’s estimates with CDC communication about them, and with the Department of Health and Human Services’ new H1N1 vaccination campaign, “Together we can all fight the flu,” launched on December 7.
I don’t have any opinion on whether the estimates the CDC reported on December 10 are reliable, valid, and useful. But I am certain that the arithmetic I have performed on those estimates to show what they mean is solid. And I am certain that what the CDC’s estimates mean diverges significantly from what the U.S. government is telling people about the pandemic.
Bottom line one is what the CDC’s December 10 estimates mean:
- Children (0–17) and adults (18–64) are much more affected, in terms of both deaths and hospitalizations, than they are in an average flu season. Seniors (65+) are much less affected than in an average flu season.
- Nonetheless, the pandemic so far is much less severe than an average flu season in terms of total deaths and hospitalizations per million cases. That is, a much higher percentage of people with swine flu than of people with the seasonal flu recover, and do so without requiring hospital care. This is true mostly because the pandemic is enormously less dangerous than the seasonal flu for people over 65, who account for 90% of all seasonal flu deaths in an average year.
- The pandemic case attack rate is much higher for children than for adults and seniors. So far, kids are likeliest to catch swine flu, by far.
- The pandemic case fatality rate is much higher for adults and seniors than for children. So far, kids are least likely to die if they catch swine flu, again by far.
- The pandemic population mortality rate is also higher for adults and seniors than for children. This is the most useful parameter for comparing the relative risk of different age cohorts. So far, adults and seniors are significantly likelier than kids to first catch swine flu and then die of a flu-related illness.
Bottom line two is what the public is being told:
- The official HHS pandemic vaccination campaign frequently says
children under 18 are most at risk.
- The vaccination campaign appropriately targets high-risk subgroups among young adults, but never mentions that, in general, adults 18 and older are at higher risk than children under 18.
- No vaccination campaign messages have prioritized seniors, even high-risk seniors, despite the fact that seniors’ population mortality rate is only slightly lower than that of adults 18–64, and much higher than that of kids under 18.
- The CDC’s news briefing on its December 10 estimates focused on the risk to children and young adults, implying that the risk was much lower to older adults and seniors. (The CDC may have information suggesting that younger adults in the 18–64 age group are at higher risk than older adults in that age group, but the December 10 CDC estimates do not include this information.)
- To the extent that the public continues to believe, mistakenly, that swine flu is deadliest to children and least deadly to the elderly, it seems likely that many older Americans may underestimate their own risk and therefore decide not to get vaccinated, even when vaccine finally becomes available to them.
This is my second time analyzing the CDC’s pandemic risk estimates compared to the CDC’s pandemic risk communication. On December 2, I posted an update that examined the implications of previous CDC estimates from the first six months of the pandemic. That update also criticized the CDC for failing to acknowledge the implications of its estimates, particularly in its November 12 press briefing.
The CDC’s first estimates included data through October 17, about a week or so before the peak of the second U.S. wave. The CDC’s second estimates, released December 10, include data through November 14, a couple of weeks after that peak. But there is still a lot more influenza (more cases, hospitalizations, and deaths) to come – and to be estimated – during the subsequent downslope weeks of the second wave.
Though the numbers all increased substantially from the first to the second set of CDC estimates, the proportions did not change much. In fact, little has changed in the implications of the CDC’s estimates, in what the public is being told, or in the gap between the two.
I made three main risk communication points in the earlier update:
- The CDC has conveyed a misimpression of how deadly the pandemic is and which age cohorts are most at risk of dying from it.
- If and when people become aware that they have been given a misimpression, the CDC risks sacrificing credibility – credibility it will need if this pandemic turns more severe; if another, more severe, pandemic arises; if controversies arise about vaccine safety; etc.
- The goal of motivating people (especially young people) to get vaccinated may make it tempting not to correct these misimpressions. But the price of reduced transparency and reduced credibility is too high. Sustainable public health leadership requires a very high level of candor, even if that candor may diminish achievement of a specific public health objective.
These points remain on target.
Analysis of the Three Age Groups
Children
0–17 | The CDC estimates 16 million cases, 71,000 hospitalizations, and 1,090 deaths.
U.S. Census data show that 24.3% of the U.S. population of 308 million is under 18; that comes out to 75 million children.
16 million cases out of 75 million children = 21.3% case attack rate
(21 sick children out of every hundred children)
1,090 deaths out of 16 million cases = 0.007% case fatality rate
(70 dead children out of every million sick children)
21.3% (CAR) × 0.007% (CFR) = 0.00149% population mortality rate
(14.9 dead children out of every million children in the population)
71,000 hospitalizations out of 16 million cases = 0.44% case hospitalization rate
(4.4 hospitalizations out of every thousand sick children)
1,090 deaths out of 71,000 hospitalizations = 1.5% inpatient mortality rate
(15 dead children out of every thousand children hospitalized)
|
Adults
18–64 | The CDC estimates 27 million cases, 121,000 hospitalizations, and 7,450 deaths.
U.S. Census data show that 62.9% of the U.S. population of 308 million is 18–64; that comes out to 194 million adults.
27 million cases out of 194 million adults = 13.9% case attack rate
(14 sick adults out of every hundred adults)
7,450 deaths out of 27 million cases = 0.028% case fatality rate
(280 dead adults out of every million sick adults)
13.9% (CAR) × 0.028% (CFR) = 0.00389% population mortality rate
(38.9 dead adults out of every million adults in the population)
121,000 hospitalizations out of 27 million cases = 0.45% case hospitalization rate
(4.5 hospitalizations out of every thousand sick adults)
7,450 deaths out of 121,000 hospitalizations = 6.2% inpatient mortality rate
(62 dead adults out of every thousand adults hospitalized)
|
Seniors
65+ |
The CDC estimates 4 million cases, 21,000 hospitalizations, and 1,280 deaths.
U.S. Census data show that 12.8% of the U.S. population of 308 million is 65 and over; that comes out to 39 million seniors.
4 million cases out of 39 million seniors = 10.3% case attack rate
(10 sick seniors out of every hundred seniors)
1,280 deaths out of 4 million cases = 0.032% case fatality rate
(320 dead seniors out of every million sick seniors)
10.3% (CAR) × 0.032% (CFR) = 0.00330% population mortality rate
(33.0 dead seniors out of every million seniors in the population)
21,000 hospitalizations out of 4 million cases = 0.52% case hospitalization rate
(5.2 hospitalizations out of every thousand sick seniors)
1,280 deaths out of 21,000 hospitalizations = 6.1% inpatient mortality rate
(61 dead seniors out of every thousand seniors hospitalized)
|
Comparisons by parameter
- Case attack rates:
- Children 21.3%
Adults 13.9%
Seniors 10.3%
The pandemic is likeliest to sicken children, and least likely to sicken seniors.
- Case fatality rates:
- Children 0.007%
Adults 0.028%
Seniors 0.032%
The pandemic is likeliest to kill sick seniors, and least likely to kill sick children.
- Population mortality rates:
- Children 0.00149%
Adults 0.00389%
Seniors 0.00330%
The pandemic is likeliest to first sicken and then kill adults; it’s nearly as dangerous to seniors, but much less dangerous to children.
- Case hospitalization rates:
- Children 0.44%
Adults 0.45%
Seniors 0.52%
The differences are small, but sick seniors are likelier to be hospitalized than sick adults or children.
- Inpatient mortality rates:
- Children 1.5%
Adults 6.2%
Seniors 6.1%
Hospitalized adults and seniors are much likelier to die than hospitalized children. (Note that some people die of influenza without having been hospitalized first; these deaths are part of the CDC’s estimated total number of deaths. Thus the number of deaths divided by the number of hospitalizations, reported here, is a rough and somewhat inflated measure of inpatient mortality rates.)
Some conclusions based on the December 10 CDC estimates
For the H1N1 pandemic:
- The age-specific case attack rates tell us that so far children 0–17 are most likely to catch swine flu.
- The age-specific case fatality rates tell us that so far seniors 65+ are most likely to die if they do catch swine flu.
- The population mortality rates tell us that so far adults 18–64 are most likely to do both: to catch swine flu and then die as a result.
The data do not permit assessment of younger versus older children (0–4 versus 5–17) or of younger versus older adults (18–49 versus 50–64) or of younger versus older seniors (65–74 versus 75+), though these finer distinctions may make a difference.
The pandemic is attacking a higher percentage of children than of adults and seniors. But among the three groups, the children are least likely to die.
It is nonetheless true that the pandemic is more deadly than the seasonal flu to children 0–17 and adults 18–64:
- Approximately 90% of the 36,000 seasonal flu deaths in an average year are 65 and over, leaving only 3,600 deaths among children and adults under 65.
- By comparison, 11% of pandemic deaths so far are children, 76% of the deaths are adults, and 13% are seniors. The U.S. population is made up of 24% children, 62% adults, and 13% seniors.
In other words:
- The seasonal flu discriminates overwhelmingly against seniors (65+) – seniors are 13% of the U.S. population and 90% of U.S. seasonal flu deaths.
- By contrast, the pandemic so far is discriminating against adults (18–64), though less overwhelmingly; adults are 62% of the population and 76% of the swine flu deaths.
- For both the seasonal flu and the pandemic so far, children (0–17) make up a much smaller percentage of the death toll than of the population.
It is tragic that the pandemic is killing more children – a lot more children – than usually die from the flu. It is nonetheless deducible from the CDC estimates that the pandemic is less dangerous to children than it is to adults and seniors.
Analysis of the Pandemic versus the Seasonal Flu
While the preceding analysis of the pandemic itself is based entirely on the CDC December 10 estimates plus census data, the comparisons with seasonal flu estimates are not nearly as crisp. The CDC’s methodologies for estimating the seasonal flu burden and its distribution among age cohorts are necessarily quite different from its methodologies for estimating the burden to date of the pandemic. So we are not comparing apples with apples.
But if it is approximately correct that about 90 percent of seasonal influenza-related deaths are in people 65 and older – as the CDC frequently reports – then the comparisons above between how the seasonal flu affects different age groups and how the pandemic so far affects different age groups should be approximately (but only approximately) on target.
The same is true for the comparisons below about overall seasonal flu severity versus pandemic severity so far. If it is approximately correct that about 5–20% of the U.S. population catches the flu in an average year, about 200,000 of them are hospitalized, and about 36,000 of them die, then the severity comparisons below should be approximately (but only approximately) correct as well.
| Cases: | There have been an estimated 47 million pandemic cases so far, 15.3% of the U.S. population of 308 million. The seasonal flu averages roughly 31 million cases per year, 10% of the 308 million total U.S. population. The CDC says the seasonal flu case attack rate ranges from 5% to 20%. At 15.3% and climbing, the pandemic is already near the upper end of the seasonal flu range. |
| Hospitalizations: | There have been an estimated 213,000 pandemic hospitalizations so far – versus roughly 200,000 hospitalizations in the average seasonal flu year. |
| Deaths: | There have been an estimated 9,820 pandemic deaths so far – versus roughly 36,000 deaths in the average seasonal flu year. |
Thus the number of pandemic H1N1 cases (15% of the population) from the start of the pandemic through November 14 was already getting close to the upper end of the CDC’s estimated range of seasonal flu cases (5% to 20% of the population). And that was at a point when the second wave was far from over. Through November 14, those cases had led to 106% as many hospitalizations as the average seasonal flu (213,000 pandemic H1N1 hospitalizations so far versus a seasonal average of 200,000 hospitalizations), which had led to only 27.3% as many deaths as the average seasonal flu (9,820 pandemic H1N1 deaths so far versus a seasonal average of 36,000 deaths). Remember: These comparisons are all methodological “apples and oranges.” But they are all we’ve got so far.
Here they are without any numbers: The pandemic has already sickened a lot more people than the seasonal flu average. Despite a lot more people getting sick, only slightly more people than the seasonal flu average have needed hospitalization. And with slightly more people hospitalized, far fewer people – less than one-third as many – have died.
If “mild” refers to the number of people who get sick, the pandemic is not milder than the seasonal flu average. In those terms it is already more severe than the seasonal flu average, and climbing. If “mild” means the percentage of the population or the percentage of sick people who end up dying, then the pandemic – so far – is significantly milder than the seasonal flu average.
But what’s happening in this pandemic to children under 18, and to adults 18-64, is certainly not mild, compared to the much smaller impact of the seasonal flu on those age groups.
What the Government Is Saying
The following three quotations are all from CDC Director Thomas Frieden’s December 10 press briefing, at which the CDC released the latest estimates. They are Dr. Frieden’s only remarks at the briefing bearing on the significance of the estimates.
The bottom line is that by November 14th, the day up to which those estimates include, many times more children and younger adults, unfortunately, have been hospitalized or killed by H1N1 influenza than occurs during a regular flu season….
What we have seen so far reiterates that people under the age of 65 are most heavily impacted by influenza. By November 14th, many times more children and younger adults, unfortunately, have been hospitalized or killed by H1N1 influenza than happens in a usual flu season. Specifically, there have been, we estimate there have been nearly 50 million cases, mostly in younger adults and children. More than 200,000 hospitalizations which is about the same number that there is in a usual flu season for the entire year. And, sadly, nearly 10,000 deaths, including 1,100 among children and 7,500 among younger adults. That’s much higher than in a usual flu season. So as we’ve seen for months this is a flu that is much harder on younger people and fortunately has largely spared the elderly until now….
In terms of comparison of this year’s flu with H1N1 influenza with seasonal flu, we know that it’s much milder for older people. It’s much less likely to result in death because older people are much less likely to get infected. But it has been a much worse flu season for people under the age of 65, particularly younger adults and children. The estimate we have – the estimate that we’re releasing here is not done in the same way that gives us the 36,000 estimate. That estimate is a different methodology. And will give a slightly larger number than this number would give. But if you were to compare, even though it’s not a directly applicable comparison, under 50 in that estimate, there are less than 1,000 deaths a year in age under 50. We didn’t break out in this – we’re not able to at this time, the 50 to 64 versus [under] 50. But a large portion of those adults are under 50. So it is really many times more severe in terms of severe illness and hospitalizations are several times higher for children and young adults as well in H1N1 than in a usual flu season….
Dr. Frieden’s comments convey the strong impression that pandemic risk is highest for children 0–17 and adults 18–50. As we have seen, the CDC’s December 10 data say that the pandemic is deadliest so far to the 18–64 age group, slightly less deadly to the 65+ age group, and least deadly to the 0–17 age group.
The vaccination public service announcements released by the Department of Health and Human Services on December 7 emphasize three groups: children, pregnant women, and young adults.
Here’s the text of one 10-second television PSA: “Children are especially at risk for the H1N1 flu virus. So get yours vaccinated. Learn more at flu.gov. Together, we can all fight the flu.”
Are children really “especially at risk” for the pandemic virus?
- If you think “especially at risk” means “more at risk than from the average seasonal flu,” then the statement is true.
- If you think “especially at risk” means “more at risk than their parents and grandparents,” then the statement is false according to the CDC’s estimates.
I don’t want to speculate on which message, the true one or the false one, the writers of this PSA meant their audience to hear. Either message would presumably help motivate parents to get their children vaccinated. But which message, the true one or the false one, will adults and seniors hear when they listen to the PSA, and how will that message affect their intention to get vaccinated?
And here is a line from a 30-second PSA distributed by HHS: “Kids run a higher risk of getting the H1N1 flu and developing serious complications.” What message are people in all age groups likely to get from the second half of that sentence – that children are likelier to have serious swine flu complications than older people (false) or that children are likelier to have serious swine flu complications than during an average flu season (true)?
The CDC website currently describes the U.S. government’s pandemic vaccine priority groups as follows:
These target groups include pregnant women, people who live with or care for infants younger than 6 months of age, healthcare and emergency medical services personnel with direct patient contact, infants 6 months through young adults 24 years of age (especially children younger than 5 years of age), and adults 25 through 64 years of age who are at higher risk for 2009 H1N1 complications because of chronic health disorders or compromised immune systems.
I am not making any policy recommendation about vaccine prioritization. It’s not my field. And there are several coherent reasons for prioritizing children (and the youngest adults) even if they are less at risk than their parents and grandparents:
- Young people have more years of life expectancy left.
- Young people are our future.
- Young people may be more likely to transmit infections than the elderly.
- Young people usually have a better antigenic response to influenza vaccines than the elderly.
- Surveys show most Americans would rather protect the young than the elderly.
The question of whether children should be prioritized for vaccination is separable from the question of whether the public should be given misleading information about the relative risk to different age groups.
Good risk communication requires that messaging about vaccine prioritization should always be compatible with the latest available information about the relative risk to the various age groups. Then, if there are reasons for choosing not to align vaccine prioritization with age-related risk, those reasons should be explained. And to the extent that those reasons may be controversial, they should be debated. For people to participate usefully in that debate, they need sound information about both the scientific data (e.g. children are least at risk) and the related values concerns (e.g. children have their whole lives ahead of them).
As the vaccine supply increases to the point where prioritization will no longer be necessary, the question of what to tell people about the relative risk to different age groups will be more important than the question of which age groups to vaccinate first – not just from the perspectives of integrity and credibility, but also from the perspective of public health: motivating precautionary behavior in people not previously prioritized. Many of my friends – mostly in their sixties – have decided they don’t need to be vaccinated against the pandemic virus because they have received the clear impression that their risk from that virus is very low. This misimpression made them comfortable going to the back of the line when the vaccine supply was inadequate. Now it makes them unmotivated to get in line at all.
I want to end this update with a story about U.S. public health resource prioritization in the early history of a different pandemic, one that continues to afflict the world. The punch lines are quotes from a medical ethicist and a former New York City health commissioner arguing for candor.
In the early years of the AIDS pandemic, cases of HIV in the United States were highly concentrated in certain identifiable groups. Efforts to prevent the disease from spreading more broadly – which has since happened – should logically have focused in those early years on the most at-risk groups.
But according to a 1997 Pulitzer Prize-winning Wall Street Journal article by Amanda Bennett and Anita Sharpe, the U.S. government made a political decision to conduct a broad-based anti-HIV campaign instead. It did so despite “unpublished research by the CDC itself [which concluded] that ‘the most effective efforts to reduce HIV infection will target injecting drug users on the Eastern seaboard, young and minority homosexual and bisexual men, and young and minority heterosexual women and men who smoke crack cocaine and have many sexual partners.’”
Bennett and Sharpe asked: “Shouldn’t the public hear the truth, even if there might be adverse consequences?” Their story quotes statements from Boston University medical ethicist George Annas and former New York City Health Commissioner Stephen Joseph that answer their question:
Annas: “When the public starts mistrusting its public health officials, it takes a long time before they believe them again.”
Joseph: “Political correctness has prevented us from looking at the issue squarely in the eye and dealing with it. It is the responsibility of the public-health department to tell the truth.”
Like Joseph, CDC Director Thomas Frieden is also a former New York City Commissioner of Health. During his tenure in New York, he worked courageously to fight HIV, sometimes speaking out in ways that were politically hazardous. In 2005, for example, he quickly announced the discovery of a new, multi-drug-resistant strain of HIV, braving criticism from some scientists for going public too soon, and from some gay activists for promoting sexual stereotypes and trying to frighten gay men into practicing safe sex. Jody Lanard and I wrote a column praising Dr. Frieden for exemplary, candid risk communication.
I hope he will do it again.
My wife and colleague Jody Lanard assisted on this update.
Note: Before the December 10 CDC estimates and press briefing, I had largely completed a different “ Update on the Update” about my original December 2 update on the CDC’s original November 12 estimates and press briefing. It covered four topics:
- The uncomfortable response of many public health professionals to the update
- Flaws they pointed out in the update
- Increased media attention to the pandemic’s mildness
- Continuing CDC interpretations – misinterpretations, in my view – of the November 12 data
Interested readers are welcome to read what I wrote here.
(Added: December 15, 2009)
Related developments since this Swine Flu Pandemic Communication Update was posted on December 15, 2009:
- On January 15, 2010, the CDC updated its estimates of swine flu cases, hospitalizations, and deaths for three age groups: 0–17, 18–64, and 65+. Once again it did not do the arithmetic to show that swine flu was deadliest to adults and least deadly to children. The CDC report included this double–comparison sentence: “The data confirms that people younger than 65 years of age are more severely affected by this disease relative to people 65 and older compared with seasonal flu.”
- On January 22, 2010, the CDC published age–specific population mortality rates for the H1N1 pandemic … for the first time as far as I can determine. That week’s Morbidity and Mortality Weekly Report (MMWR) included this sentence: “Since August 30, cumulative deaths associated with laboratory–confirmed 2009 H1N1 infection per 100,000 population were 0.31 for persons aged 0–4 years, 0.26 for 5–18 years, 0.38 for 19–24 years, 0.60 for 25–49 years, 1.03 for 50–64 years, and 0.65 for 65+ years.”
- On February 2, 2010, I posted a Guestbook entry entitled “Why did the CDC misrepresent its swine flu mortality data – innumeracy, dishonesty, or what?” I argued that although the CDC had published data showing that the swine flu risk was lowest for children and highest for adults aged 50 and over, it had continued to pursue a vaccination messaging strategy inconsistent with its own data.
- On February 12, 2010, the CDC posted another update of estimated cases, hospitalizations, and deaths for the three age groups. Like the others, this update did not do the arithmetic to show that swine flu was deadliest to adults and least deadly to children. It included this sentence: “The data by age provided in the updated estimates continues to confirm that people younger than 65 years of age are more severely affected by this disease relative to people 65 and older compared with seasonal flu.”
- On February 17, 2010, the CDC posted a webpage entitled “Flu–Related Hospitalizations and Deaths in the United States from April 2009 – January 30, 2010.” The new page included three additional weeks of data beyond what was reported in the January 22 MMWR. More importantly, it showed the swine flu death rates for different age groups in a clear bar graph, instead of buried in the middle of a paragraph. Hospitalization data were also graphed.
(Added: February 18, 2010)
December 2, 2009
It’s Official (sort of):
The Swine Flu Pandemic Is Mild So Far
by Peter M. Sandman
 People who get swine flu are one-sixth as likely to die as people who get the ordinary seasonal flu. That’s according to estimates released by the U.S. Centers for Disease Control and Prevention (CDC) on November 12, 2009.
People who get swine flu are one-sixth as likely to die as people who get the ordinary seasonal flu. That’s according to estimates released by the U.S. Centers for Disease Control and Prevention (CDC) on November 12, 2009.
But the CDC didn’t say so. And journalists didn’t do the math. So nothing like the previous paragraph appeared anywhere in the mainstream media on the day of the CDC announcement or the days that followed.
Here I am, three weeks later, a risk communication expert not a flu expert, telling you that the CDC “secretly” (well, quietly) thinks the swine flu pandemic is mild.
So far, anyway. Influenza is famously unpredictable, and influenza pandemics are even more so. Don’t bet the farm (or your life) that swine flu will stay mild, because it could turn more virulent at any time. Still, the big news virtually everybody has missed is that U.S. public health officials think it’s mild so far.
On November 30, while I was putting the finishing touches on this update, Dr. Martin Cetron of the CDC participated in a webinar on the lessons of the 1918 pandemic. I didn’t listen to the webinar, but a reporter for the University of Minnesota’s Center for Infectious Disease Research & Policy (CIDRAP) did. That day’s CIDRAP News Headlines carried this news brief:
CDC estimates case-fatality rate at .018%
The estimated case-fatality rate (CFR) for pandemic H1N1 flu so far is .018% – about 100-fold lower than the 2% CRF in the pandemic of 1918–19, Dr. Martin Cetron of the Centers for Disease Control and Prevention (CDC) said today. Cetron, director of the CDC Division of Global Migration and Quarantine, gave the estimate in a webcast, presented by Public Health Reports, on lessons of the 1918 pandemic.
Though CIDRAP didn’t say so, presumably Dr. Cetron cited the November 12 CDC estimates. (There’s no other way he could have come up with 0.018%.) As far as I know, he is the first person at CDC or elsewhere to use those estimates publicly to calculate a CFR. I don’t know if he made the comparison to seasonal flu.
And the next morning, while my webmaster was preparing to post the update, the New York Times published an editorial that finally used the CDC’s November 12 estimates to demonstrate that the pandemic is milder than the seasonal flu. Entitled “The Swine Flu, as of Now,” the editorial included this key passage:
So far, the news about swine flu is better than expected. The pandemic may have reached its peak and is heading downward in all regions of the country; weekly deaths from swine flu have started to decline; the virus remains relatively mild; there seem to be few claims of serious side effects from the vaccine; and despite widespread complaints about shortages, vaccine supplies are steadily building up.
By mid-October, the latest estimates available, the swine flu had infected some 22 million Americans, sent roughly 98,000 to the hospital and killed roughly 3,900. Those numbers may sound high, but they are not apt to reach the levels of harm caused by a normal flu season.
There it is: the key November 12 numbers keeping company with the phrases “relatively mild” and “not apt to reach the levels of harm caused by a normal flu season” in a major national newspaper.
Most of what's in this update still stands; one webinar and one editorial aren’t nearly enough to teach the American people that the pandemic is mild. But they’re a start.
This update is partly the evidence that that’s really what the CDC is saying-but-not-saying, and partly an assessment of why the CDC isn’t saying it more candidly and why reporters aren’t hearing it at all.
The Basic Swine Flu Numbers
The obvious question to ask about any risk is: How serious is it? Risk assessors long ago partitioned seriousness into two components:
- Probability (or frequency) – how often does it happen; how many people does it happen to?
- Magnitude (or consequence) – when it happens, how bad is it?
For an infectious disease, the probability measure is the case attack rate (CAR) – what percentage of the population gets the disease in some unit time? The most important magnitude measure is the case fatality rate (CFR) – what percentage of those who get the disease die from it? – though hospitalization rates and absenteeism rates are also pretty important.
On November 12, for the first time, the CDC provided its best estimate of these two numbers for the first six months of the swine flu pandemic.
Well, not really. It didn’t actually provide a CAR or a CFR. It could have, but chose not to. But it did provide the data needed to calculate these two crucial statistics.
The CDC estimated that about 22 million Americans (with a range of 14–34 million) were sick with swine flu between late April when it first appeared and October 17. The U.S. population is currently 308 million. So a little over seven percent of Americans have had swine flu so far (22 million is 7.1% of 308 million). That’s the swine flu case attack rate for the first six months of the pandemic. It can only go up, as more people in the same population get sick.
By contrast, the average flu season sickens 5–20% of Americans. But of course the next six months could tell a very different story. It’s too soon to tell.
Out of the 22 million swine flu cases so far, the CDC estimated, about 3,900 (with a range of 2,500–6,100) died. That’s a case fatality rate of 0.018% – 180 swine flu deaths for every million swine flu illnesses.
The pandemic case fatality rate could also get higher in the months ahead, especially if the swine flu virus mutates to become more virulent. But unlike a case attack rate, which automatically keeps climbing as the unit time grows longer (as long as the disease remains in circulation), there’s no particular reason to expect a case fatality rate to increase, decrease, or remain the same. So far, at least, the pandemic CFR in the United States is approximately 0.018%.
For an influenza pandemic, a case fatality rate of 0.018% is an astonishingly low number. It’s a lot lower than the CFR of previous pandemics, and a lot lower than the CFR of the average flu season.
These numbers are the biggest pandemic news in some time. They prove that so far the pandemic is mild.
The CDC didn’t interpret the numbers that way, and the media didn’t cover them that way. That’s the main thing I want to talk about.
But I want to talk about four other things first:
- The CDC provided not just overall estimates of the number of U.S. cases and deaths, but also separate estimates for three age groups. I want to get those estimates (and CARs and CFRs based on them) onto the table too, so we can see whether the pandemic is severe for some even though it’s mild overall.
- Risk estimates take on meaning mostly in comparison to other risks that are larger or smaller. I want to put the pandemic’s CAR and CFR figures into context by comparing them in detail to comparable figures for the seasonal flu, the 1918 pandemic, and bird flu. (You can skip this part if you don’t like numbers and you’re willing to take my word for it.)
- The meaning of the word “mild” is central to this update. I want to detail what I mean by the word. In particular, I want to talk about the ways in which this pandemic looks less dangerous than it did at first, the ways in which it could get worse, and the ways in which it could get still less serious … and could even end up saving lives.
- Nearly everything in this update is based on CDC estimates. I want to explain why we need to rely on estimates, why we don’t have solid counts of flu cases and flu deaths.
Then, finally, I can turn to the risk communication issues:
- Why does the CDC virtually never use the word “mild” to describe the pandemic virus?
- Why do local health officials and journalists settle for the meme that pandemic H1N1 is “about like the seasonal flu”?
- Why did the CDC decide to interpret its November 12 estimates as more alarming than reassuring?
- Why did the media go along with the CDC’s misinterpretation?
- And why do I think it’s important for health officials to be more candid about the fact that the pandemic is mild so far, as well as the possibility that it could turn more virulent.
Ages of Swine Flu Victims
The CDC divided the U.S. population into three age groups: 0–17, 18–64, and 65+. For convenience, I’ll call them children, adults, and seniors. Here are the relevant estimates. For each age group, the first line comes directly from the CDC. The other three lines are my arithmetic to calculate a case attack rate (for the first six months of the pandemic) and a case fatality rate. The only additional information used is the U.S. census data.
| Children: | CDC estimates 8 million cases and 540 deaths
24.3% of the U.S. population of 308 million = 75 million children
8 million cases out of 75 million children = 10.7% CAR
(11 sick children out of every hundred children)
540 deaths out of 8 million cases = 0.007% CFR
(70 dead children out of every million sick children) |
|---|
| Adults: | CDC estimates 12 million cases and 2,920 deaths
62.9% of the U.S. population of 308 million = 194 million adults
12 million cases out of 194 million adults = 6.2% CAR
(6 sick adults out of every hundred adults)
2,920 deaths out of 12 million cases = 0.024% CFR
(240 dead adults out of every million sick adults) |
|---|
| Seniors: | CDC estimates 2 million cases and 440 deaths
12.8% of the U.S. population of 308 million = 39 million seniors
2 million cases out of 39 million seniors = 5.2% CAR
(5 sick seniors out of every hundred seniors)
440 deaths out of 2 million cases = 0.022% CFR
(220 dead seniors out of every million sick seniors) |
|---|
Okay, so what stands out?
These conclusions are in conflict with two things you may have heard.

You may have heard that the pandemic is especially high-risk for children.
The CDC does keep saying that. But based on the CDC’s own estimates, it’s simply not true. Children are likelier than adults or seniors to get swine flu, but less likely to die from it. (This may or may not be true for certain narrower age groups of children, but the CDC’s November 12 estimates say it is true for the entire population of Americans under 18.)
It is true – and the CDC keeps stressing – that swine flu has already killed more children in six months than an average flu season kills in a year. The pandemic is deadlier for kids than the seasonal flu. But that’s because the seasonal flu is especially unlikely to kill children, not because the pandemic is especially likely to do so. The pandemic really is deadlier to kids than the seasonal flu … but it’s less deadly to kids than it is to adults and seniors.
There are still two defensible reasons to make children a high-priority target for swine flu vaccination: the fact that children catch and spread infections more effectively than older people, so vaccinating kids protects their parents and grandparents; and the value judgment (which I share) that children’s lives are more worth protecting than the lives of older people. But according to the CDC’s numbers, children are least threatened, not most threatened, by the pandemic virus.

You may have heard that the pandemic is especially low-risk for seniors.
That’s not true either, if the CDC’s numbers are right. Seniors are a little less likely than adults to get swine flu – and a lot less likely than children. They’re a little less likely than adults to die if they get it – but a lot more likely than children.
When the two factors are considered together (which is what the population mortality calculation does, separately for each age group), the pandemic’s risk is highest for adults and lowest for children. Seniors are right smack in the middle.
It has been widely reported that seniors are partly protected from the pandemic by their exposure to a similar H1N1 virus back in the 1950s. (I have written this myself, several times.) Maybe it’s true. But the CDC’s November 12 numbers say that compared to people 18–64, people 65 and over are:
- only a little less likely to get swine flu (5.2% versus 6.2% CAR); and
- only slightly less likely to die if they get it (0.022% versus 0.024% CFR).
These differences are pretty minor, hardly a valid basis for concluding that adults should worry and seniors shouldn’t.
Overall Comparison to Seasonal Flu
The seasonal flu isn’t a single phenomenon; there are severe flu seasons and mild flu seasons. So the seasonal flu numbers below aren’t just estimates (like the pandemic numbers above); they are estimates of averages.
According to the CDC, about 10% of the U.S. population gets the seasonal flu in an average year. The number ranges between 5% and 20%, but we’re going to stick with the 10% average. So the seasonal flu case attack rate is about 10%. That means there are 31 million flu cases a year, on average, in the current U.S. population of 308 million.
The estimated average number of annual U.S. deaths from the seasonal flu, again according to the CDC, is 36,000. If 31 million people get sick and 36,000 die, that’s a case fatality rate of 0.12%.
Of course the actual CFR varies with the severity of each year’s flu strains, the effectiveness of each year’s vaccine, the number of people who get vaccinated, and other factors. It ranges from 0.05% to 0.2%, but is usually shorthanded to an average for a typical year of about 0.1%. We’ll stick with 0.12%, 36,000 deaths divided by 31 million cases. That’s 1,200 deaths for every million cases of flu.
If we multiply the average CAR of 10% by the average CFR of 0.12%, we get an average seasonal flu PMR (population mortality rate) of 0.012%. For every million people in the United States, roughly 120 of them die every year of a flu-related illness.
So here’s the overall comparison for all three parameters, case attack rates, case fatality rates, and population mortality rates:
| 2009 Pandemic (estimated) | Seasonal Flu (estimated average) |
|---|
| CAR | 7.1% (6 months) | 10% (annual) |
|---|
| CFR | 0.018% (180 in a million) | 0.12% (1,200 in a million) |
|---|
| PMR | 13 in a million (6 months) | 120 in a million (annual) |
|---|
The comparison of case attack rates (and therefore population mortality rates) isn’t terribly useful yet. The seasonal flu numbers are annual averages, while the pandemic has lasted only six months so far. There’s no way to predict what will happen over the next six months. If the pandemic virus continues infecting people at the same rate as the first six months, that would yield a first-year CAR for the pandemic of 14.2%, significantly more than the average seasonal flu. But there’s no reason to expect the next six months to be identical to the first six months. The pandemic could accelerate; we’re approaching winter, and influenza tends to transmit better in winter. Or the pandemic could ebb; as I write this, it seems to be ebbing. Or it could accelerate and then ebb. Or it could ebb briefly and then come roaring back in a third wave in late winter or spring.
For what it’s worth, previous flu pandemics have ended up sickening one-quarter to one-half of the population over roughly two years. And the first year has usually been bigger than the second year. So this pandemic’s 7.1% case attack rate for its first six months is a little on the low side for a pandemic … but it’s early days yet.
Still, unless it fades soon, the pandemic is on course to sicken more than 10% of the population by the end of its first year, beating out the average flu season.
Note that the typical U.S. flu season runs from November through April, usually peaking in January and February. Pandemics, by contrast, have no season (though they tend to be worse in cold weather than hot weather). In the U.S., the swine flu pandemic started in late April, had a spring spike, then receded but didn’t disappear over the summer, then spiked again in the fall, and now seems to be receding again (though there’s no way to know if it will keep receding).
Statements pointing out that the amount of pandemic illness is very high “so early in the flu season” are accurate if they mean to suggest that only during pandemics do we see a lot of flu in spring and fall. And it’s reasonable to worry that the pandemic might get worse as the weather gets colder. But it is misleading to compare the pandemic’s first six months with the seasonal flu’s off-season in order to imply that the pandemic is making more people sick than the seasonal flu. To compare the pandemic’s CAR with the seasonal flu’s CAR, the most valid comparison is a year versus a year, and this pandemic’s first year started in late April 2009.
The more enlightening comparison for now is the pandemic’s CFR with the seasonal flu’s CFR. Those numbers don’t include any time unit. The average seasonal flu kills 1,200 Americans for every million it makes sick. So far, the swine flu pandemic has killed only 180 Americans for every million it has made sick. In other words, the average seasonal flu is more than six times as deadly as swine flu if you get it.
There’s a word for a pandemic virus that is less than one-sixth as virulent as the average seasonal flu virus. The word is mild.
Comparison to Seasonal Flu by Age Groups
What about the three age groups? Does the picture change when we look separately at children, adults, and seniors?
We can’t do a rigorous comparison. I can’t find published seasonal flu attack rates separately for children, adults, and seniors. And the CDC only started collecting data on pediatric seasonal flu deaths a few years ago.
Here are the two key published CDC estimates for seasonal flu: It kills an average of 36,000 people a year in the U.S., and 90% of them are 65 and over. Let’s work with just those two numbers to get two population mortality rate estimates for the seasonal flu, one for Americans 65 and over and one for Americans under 65:
- 90% of 36,000 U.S. flu-related deaths are in people 65 and over. 90% of 36,000 = 32,400. So an estimated 32,400 Americans 65-and-over die of a flu-related illness in the average flu season.
- 12.8% of the U.S. population of 308 million is 65 and over. 12.8% of 308 million is 39 million. So about 39 million Americans are 65 and over.
- Dividing #1 (32,400 flu-related deaths in people 65 and over) by #2 (39 million people 65 and over) yields an estimated average seasonal flu-related annual mortality rate for U.S. seniors of 0.083%. (Reminder: This isn’t the case fatality rate. It’s the 65-and-over population mortality rate, the percentage of the population 65 and over who die of a flu-related illness in an average year, not the percentage of that year’s 65-and-over flu cases who die.)
- 10% of 36,000 U.S. flu-related deaths are in people under 65. 10% of 36,000 = 3,600. So an estimated 3,600 Americans under 65 die of a flu-related illness in the average flu season.
- 87.2% of the U.S. population of 308 million is under 65. 87.2% of 308 million is 269 million. So about 269 million Americans are under 65.
- Dividing #4 (3,600 flu-related deaths in people under 65) by #5 (269 million Americans under 65) yields an estimated average seasonal flu-related annual mortality rate for U.S. non-seniors of 0.0013%. (Again, this is an population mortality rate, not a case fatality rate.)
The estimated average seasonal flu population mortality rate for Americans 65 and over is 0.083% – 830 in a million. The estimated average seasonal flu population mortality rate for Americans under 65 is 0.0013% – 13 in a million. If you divide 0.083 by 0.0013, you get 64. An American in the 65-and-over age group is roughly 64 times (0.083 divided by 0.0013) as likely as an American under 65 to die from a flu-related illness.
These population mortality rate calculations are as firm (or as flimsy) as the CDC’s “36,000” and “90%” estimates are. If the CDC is right that about 36,000 Americans die in an average flu season and about 90% of them are 65 and over, then I must be right also that the seasonal flu is 64 times as likely to kill a U.S. senior as a younger U.S. resident.
But I don’t have any age-related case attack rate data for the seasonal flu. To calculate a very approximate CFR, therefore, I’m going to assume a 10% CAR for both age groups. I have already defined a disease’s population mortality rate as its case fatality rate times its case attack rate. It follows that the CFR is the PMR divided by the CAR.
So our estimate of the average seasonal flu CFR for Americans 65 and over is 0.083% divided by 0.1 = 0.83%. And our estimate of the average seasonal flu CFR for Americans under 65 is 0.0013% divided by 0.1 = 0.013%.
Now we can compare the average seasonal flu to the first six months of the swine flu pandemic. Since our seasonal calculations distinguish only two groups, under 65 and 65+, we need to combine the pandemic data for children and adults. Here’s what we get:
| | Pandemic | Seasonal |
|---|
| CAR – under 65 | 7.4% (6 months) | 10%* (annual) |
| CAR – 65+ | 5.2% (6 months) | 10%* (annual) |
| CAR overall | 7.1% (6 months) | 10% (annual) |
CFR – under 65 |
0.017% |
0.013%* |
| CFR – 65+ | 0.022% | 0.83%* |
| CFR overall | 0.018% | 0.12% |
PMR – under 65 |
13 in a million (6 months) |
13 in a million (annual) |
| PMR – 65+ | 11 in a million (6 months) | 830 in a million (annual) |
| PMR overall | 13 in a million (6 months) | 120 in a million (annual) |
(The four asterisks denote estimates that are grounded in the probably false assumption that the seasonal flu attacks under-65s and 65-and-overs with the same frequency.)
The most stunning comparison here is the four CFR estimates. Look at them:
- 0.017% (pandemic CFR for Americans under 65)
- 0.013% (seasonal flu CFR for Americans under 65)
- 0.022% (pandemic CFR for Americans 65+)
- 0.83% (seasonal flu CFR for Americans 65+)
As they say on Sesame Street: One of these is not like the others.
What jumps out from the chart is that the seasonal flu is a pretty scary disease for people 65 and over. If you catch it, the odds of it killing you are 0.83% – 83 in a thousand, nearly one in a hundred. (And lots of seniors catch it.) Of course 83 in a thousand is the average. The seasonal flu kills more seniors in years dominated by seasonal H3N2 flu than in years dominated by seasonal H1N1 flu.
The other three CFRs are all so much lower that they look almost indistinguishable by contrast: 0.013%, 0.017%, and 0.022% – from just over one in a thousand to just over two in a thousand, compared to 83 in a thousand.
But these three CFRs are worth distinguishing:
- Americans 65+ who get swine flu are a little likelier to die than Americans under 65 who get swine flu (0.022% versus 0.017%).
- Americans under 65 who get swine flu are a little likelier to die than Americans under 65 who get the seasonal flu (0.017% versus 0.013%).
- But they are all enormously less likely to die than Americans 65+ who get the seasonal flu (0.013%-0.022% versus 0.83%).
The PMR (population mortality rate) estimates are the most reliable numbers; they’re not based on the assumption of equal seasonal flu attack rates. In a mere six months, the CDC’s data say, swine flu has already killed as many Americans under 65 as the seasonal flu kills in an average year: 13 per million population. And it has killed almost the same percentage of Americans 65 and over: 11 in a million. So, yes, swine flu really is deadlier to Americans of all ages than the seasonal flu is to Americans under 65.
That’s because the seasonal flu isn’t very deadly to Americans under 65. It’s the fourth PMR that really stands out: In an average year, the seasonal flu kills not 11 seniors in a million, not 13 in a million, but 830 seniors in a million! (Remember: The average seasonal flu kills 36,000 people in the U.S.: 32,400 people 65+, and 3,600 people under 65.)
The communication problem these numbers present is a very standard problem in epidemiology: how to talk about relative risk so people don’t get a misperception of absolute risk.
Suppose there are two cancers. One is pretty rare, killing only a dozen or so people for every million in the population; the other is much more common, killing nearly a thousand people for every million. Now suppose some lifestyle choice (grilling steak over charcoal, say) increases the incidence of the first cancer, the rare one, by about a third. How worried should barbecue lovers be? On the one hand, you’re increasing the cancer rate by about a third! On the other hand, if you increase the incidence of a pretty rare cancer by about a third you still have a pretty rare cancer. A much tinier percentage increase in the incidence of the common cancer would be a much bigger absolute health threat.
In this analogy, seasonal flu for people 65 and over is the common cancer. The difference between pandemic H1N1 and the seasonal flu for people under 65 is the effect of frequent barbecuing on the incidence of the rare cancer. An ethical epidemiologist helps people interpret relative risk data based on the size of the absolute risk: “The number goes up by about a third” is ultimately less informative than “the number goes up by a few extra cases in a million.”
In a nutshell: So far, the swine flu pandemic is a little more serious than the average seasonal flu for Americans under 65. But the average seasonal flu is a life threat almost exclusively to people over 65. No age group is hit anywhere near as hard by the pandemic (so far) as seniors are hit by the seasonal flu.
Or look at it this way. People over 65 are 12.8% of the U.S. population. According to the CDC’s November 12 estimates, they make up 11.3% of U.S. pandemic deaths so far (440 out of 3,900 estimated deaths). The two percentages – 12.8% and 11.3% – are pretty close. But the CDC says people over 65 – 12.8% of the population, remember – make up 90% of U.S. seasonal flu deaths.
The main thing going on isn’t that the pandemic discriminates on the basis of age, attacking mostly the young and sparing the elderly. The difference in case attack rates is fairly small. The main thing going on is that the seasonal flu discriminates on the basis of age, killing mostly the elderly while it mostly gives their children and grandchildren a miserable week in bed.
Some seasonal flu vaccination campaigns are candid about the age differences in vulnerability, but most are not. When officials simply say that we should all get vaccinated every year because flu kills 36,000 Americans a year, they are grossly understating the risk to grandma and grossly overstating the risk to her kids and grandkids. (Children under four are also at increased risk of seasonal flu complications, compared with the rest of the under-65 group.) One reason officials perpetuate this misleading impression is that children are thought to be the main transmitters of seasonal flu. And flu vaccines are more effective in young people than in seniors. One way to protect grandma is to get her kids and grandkids vaccinated.
Individual doctors take their cue from public health professionals. The New England Journal of Medicine recently published an article by internist Danielle Ofri that offers a pristine example of a doctor who regularly oversells the risk of seasonal influenza to her patients under 65.
Dr. Ofri writes that her patients who “routinely refused the seasonal flu vaccine” were initially desperate for pandemic H1N1 vaccine last spring, when the virus first emerged. But six months later her patients were more worried about vaccine safety than about pandemic flu.
“How to explain this dramatic shift in 6 short months?” she wonders. “It certainly isn’t related to logic or facts, since few new medical data became available during this period. It seems to reflect a sort of psychological contagion of myth and suspicion.”
Leave aside that “new medical data” have in fact become available since early in the pandemic, data suggesting that the pandemic is milder than it originally looked in Mexico City. I want to focus on Dr. Ofri’s unsuccessful efforts to persuade her patients to get the seasonal flu vaccine every year.
Presumably, those patients are mostly under 65, since most Americans 65 and over do get the seasonal vaccine. How does Dr. Ofri try to persuade them to get vaccinated? Frustrated by her lack of success, she earnestly tells us her approach: “No matter how often I trotted out the statistics of 30,000 to 40,000 annual deaths from influenza, the patients would not be moved.”
It’s a safe bet that when Dr. Ofri tells her under-65 patients about the 30,000–40,000 annual deaths from influenza, she deemphasizes the fact that 90% of those deaths are in people 65 and over. Dr. Ofri probably doesn’t perceive herself as exaggerating the seasonal flu risk to her under-65 patients, but that is exactly what she is doing. It’s worth wondering whether her apparent willingness to mislead her patients in this way might have something to do with their resistance to her advice about vaccination.
I think the decision of public health authorities and individual doctors to underplay the age differences in seasonal flu vulnerability is a culpable decision. Lots of Americans under 65 get the flu every year, and 99.987% of them recover. Lots of Americans 65 and over get the flu every year, and nearly one percent of them die. Rather like breaking your hip, influenza is a big deal for the elderly and an inconvenience for the young. There are exceptions, of course; 3,600 annual flu-related deaths in the under-65 population aren’t nothing. But they pale to insignificance beside the 32,400 annual flu-related deaths in the much smaller 65-and-over population.
It’s very difficult for officials to talk coherently about the seriousness of the pandemic without first coming clean about the seasonal flu. Seasonal flu is basically two diseases: a severe one for huge numbers of seniors and a mild one for nearly all of their children and grandchildren. The swine flu pandemic so far is – for both age groups – a little more severe than the seasonal flu is for people under 65, and a lot milder than the seasonal flu is for seniors.
For the record: Despite the critique above, I think that 3,600 seasonal deaths a year in people under 65 are well worth preventing. Most of those deaths are likely to be preventable with the seasonal flu vaccine – which I believe is very safe, and which is thought to be 70% to 90% effective in young healthy people when the vaccine match is good. It is the misleading, mistrust-inducing communication that needs changing, not the important effort to increase vaccination rates.
I also need to acknowledge that there are at least two ways in which the swine flu pandemic is (or may be) worse than the average seasonal flu.
- Swine flu is especially likely to be serious for people with specific underlying medical conditions: pregnant women, asthmatics, diabetics, etc. Statistics aren’t available to permit a direct comparison, but for some of these conditions it is possible that swine flu is worse than the seasonal flu.
- The percentage of doctor visits that were for influenza-like illnesses has already reached higher peaks during the first six months of the swine flu pandemic than it usually reaches during non-pandemic flu seasons. In other words, the pandemic (and news about the pandemic, and concern about the pandemic) is sending a lot of people to the doctor with respiratory complaints who would have toughed it out at home during an ordinary flu season.
Neither of these facts is anywhere near as important as the fact that so far swine flu is much less deadly than the seasonal flu. No other fact about the swine flu pandemic is as important as that fact.
Two More Comparisons
The seasonal flu is the most useful yardstick for assessing the seriousness of the swine flu pandemic. But let me add, quickly, two other yardsticks: the pandemic of 1918 (also an H1N1 strain) and the bird flu (H5N1) threat that has hung over the world since 1997.
The 1918 pandemic is estimated to have sickened about 30%  of the U.S. population, and killed about 675,000 of them – virtually all within the space of a single year, though the pandemic actually lasted 27 months in all. The U.S. population at the time was 103 million. (1918, by the way, was the only year since 1900 in which the U.S. population actually declined, thanks to the 1918 pandemic.)
of the U.S. population, and killed about 675,000 of them – virtually all within the space of a single year, though the pandemic actually lasted 27 months in all. The U.S. population at the time was 103 million. (1918, by the way, was the only year since 1900 in which the U.S. population actually declined, thanks to the 1918 pandemic.)
So the 1918 pandemic sickened 31 million Americans (30% of 103 million). The 675,000 who died are 2.2% of the 31 million sickened, and 0.66% of the 103 million U.S. population.
Now compare the two pandemics:
| Pandemic of 2009 | Pandemic of 1918 |
|---|
| CAR | 7.1% (first 6 months) | 30% (worst 12 months) |
| CFR | 0.018% | 2.2% |
| PMR | 13 in a million (first 6 months) | 6,600 in a million (worst 12 months) |
The pandemic of 1918 was the worst pandemic in modern times, maybe the worst in history. It infected 30% of Americans, an attack rate the current pandemic may or may not eventually equal. But here’s a number the current pandemic is vanishingly unlikely to equal, unless the swine flu virus mutates and becomes far more virulent: The 1918 pandemic had a case fatality rate of 2.2%, 122 times worse than the swine flu CFR to date.
As for bird flu, there are no U.S. data, of course, since there haven’t been any U.S. cases (at least not yet). Since its emergence in 1997, the H5N1 bird flu virus has infected a grand total of 442 people worldwide, according to the World Health Organization. 262 of them died.
With a world population of 6.8 billion, bird flu’s CAR is absurdly low: 442 out of 6.8 billion is 0.0000071%. But bird flu’s CFR is terrifyingly high: 262 out of 442 is 59%. So far, in other words, H5N1 is almost impossibly difficult to catch – but if you catch it you’re likelier than not to die.
Since 1997, the pandemic worst case scenario in the back of every influenza expert’s mind has been this: What if bird flu mutates in a way that enables it to transmit efficiently from human to human, while staying just as deadly as it is already?
Meanwhile, instead of a bird flu pandemic that kills 59% of its victims, we have been dealt a swine flu pandemic that kills 0.018% of its victims – 3,278 times as mild.
So, just to rub it in:
- Worldwide bird flu CFR 59.%
- U.S. 1918 pandemic CFR 2.2%
- Average U.S. seasonal flu CFR 0.12%
- 2009 pandemic CFR in the U.S. 0.018%
Like I said: mild.
What Does “Mild” Mean Here?
Nearly all of the above numbers are based on CDC estimates. (One exception worth noting: I’m using the conventional estimate of 10% for the seasonal flu case attack rate; the CDC usually uses a range of 5% to 20% instead.)
The CDC estimates are debatable. And in fact they are hotly debated – most notably by vaccination opponents, who argue that the CDC has an incentive to overestimate both seasonal flu deaths and swine flu deaths in order to build the case for vaccination.
I’m neither a virologist nor a biostatistician, and I don’t feel qualified to have an opinion about the validity of the CDC’s estimates. But if the estimates are reasonably accurate – or even if they’re equally inflated – then it is clear that so far the swine flu pandemic is basically a practice run. It is more severe than the seasonal flu for the people least endangered by the seasonal flu (under-65s), but it’s a lot less severe than the seasonal flu for the people most endangered by the seasonal flu (65-and-overs). And it’s a lot less severe than the pandemic we were expecting.
It’s also less severe than the pandemic we thought we were getting at first. A May 2009 article in Science, based on early data from Mexico, estimated the pandemic’s case fatality rate at 0.4% – three to four times as bad as the seasonal flu’s average CFR in the U.S. In the weeks that followed, that number began to seem high, though not as high as it seems now. Here’s what I wrote about what I called “the ‘mildness’ meme” in a late June 2009 email responding to a query from Canadian Press reporter Helen Branswell:
Compared to the seasonal flu, which kills on average about one person in a thousand, swine flu isn’t especially mild. Health officials can’t calculate a precise case fatality rate because they’re not trying to count all the cases – so they don’t have any denominator for the fraction. But it’s looking like swine flu is roughly as deadly as the seasonal flu – about one death in a thousand cases. And while seasonal flu deaths are overwhelmingly the elderly, swine flu deaths tend to be younger.
By July 21, only a month later, I was writing that pandemic H1N1 “looks very mild so far” – with a case fatality rate “apparently lower than the rate for the seasonal flu.”
From the perspective of late November, May’s 0.4% and June’s 0.1% look way too high. Based on the November 12 CDC data, the best U.S. pandemic CFR estimate is 0.018%.
That could change. Flu viruses mutate, and swine flu could mutate in a way that makes it more virulent, increasing its CFR. (A mutation could also make it more transmissible, increasing its CAR. Or it could make it no longer susceptible to antiviral drugs, or to the vaccine we have worked so hard to produce.) Of course a mutation that makes swine flu even milder is also possible, but it’s the possible change for the worse that merits attention. One worst case scenario for swine flu: The swine flu and bird flu viruses mix-and-match genetic material, a process called reassortment, to produce a new flu strain with the transmissibility of swine flu and the virulence of bird flu – which would make it by far the worst flu virus in history. Even without such a catastrophic reassortment, the swine flu pandemic could come roaring back in a third wave that would make the first two waves feel like practice runs.
And that is why it’s so important for the CDC to acknowledge that this pandemic – so far – is mild. The first two waves really are practice runs, a chance to prepare for The Big One. This is not being candidly communicated to the public, so the public is not even thinking about The Big One, let alone preparing for it. Nobody knows whether The Big One is coming next month or next century. But we do know that it’s not here yet.
This is a crucial point. There are many reasons to tell people that swine flu is currently mild:
- Because it’s the truth.
- Because people who are very anxious deserve to be told they can calm down.
- Because people who already think it’s mild deserve to be told they’re right.
- Because the credibility of the CDC and of the public health profession is at stake.
But the biggest reason to tell people that swine flu is currently mild is to help people realize that what we’re experiencing so far isn’t what we have been worrying about, that we’re not out of the woods yet, that the next pandemic or the next wave of this pandemic could turn out to be The Big One.
Nonetheless, “mild” doesn’t mean “trivial.” Swine flu has, after all, killed about 3,900 Americans in six months, more than the September 11 attacks of 2001. It will surely kill more in the months ahead.
And though some think otherwise, to me the swine flu virus is surely more dangerous than the swine flu vaccine. Let the policy experts debate whether the swine flu vaccine manufacturing effort was worth the cost. That’s a puzzle that looks different today than it did last spring when decisions had to be made without knowing the virus would turn out so mild (so far) – and it’s a puzzle that may look different yet again next spring when we have twelve months of pandemic experience to look back on. The fact is, we now have a pandemic vaccine (though not yet enough of it). Despite the mildness of the virus so far, getting vaccinated ought to be a no-brainer.
This is a major conundrum for public health professionals. Surveys show that lots of Americans are already deciding against swine flu vaccination because they suspect the virus is mild. Lots more would presumably make the same decision if the CDC flat-out told them the virus is mild. But the virus is mild. So telling the truth about the mildness of the pandemic virus could undermine swine flu vaccination – and thus kill people in the coming months whose deaths could have been prevented by the vaccine.
On the other hand, continuing to exaggerate the seriousness of the pandemic by failing to be explicit about its mildness could undermine long-term public health credibility – and thus kill people in the coming decades whose deaths could have been prevented if they trusted the advice of public health officials.
Whenever health officials warn the public that something may turn out awful and it turns out pretty minor instead, credibility suffers to some extent. A number of risk communication strategies can minimize the damage: emphasizing the magnitude of the risk rather than overstating its probability; acknowledging that it may turn out minor (and voicing hope that it does); explaining that false alarms are part-and-parcel of preparedness; etc. Still, warnings that in hindsight turn out to have been unnecessary or exaggerated inevitably damage the credibility of the source. (Of course over-warning the public damages credibility a lot less than understating the risk and having the situation turn out dire. That’s why crisis communication experts always advise officials to err on the alarming side.  )
)
So yes, it’s embarrassing and a little damaging to tell people that the situation looks better (so far) than you feared. But if the situation actually looks better (so far) than you feared, telling people so does less damage to credibility than not telling them and waiting till they figure it out for themselves.
If it keeps ignoring its own data and pretending that the pandemic is less mild than it actually is (so far), the CDC will be digging itself a deeper and deeper credibility gap. It really shouldn’t let the situation deteriorate to the point where the only thing that can save the agency’s credibility is if the pandemic virus mutates into something much more severe.
For me, there’s no conundrum here. The CDC was right to warn people that the pandemic might get bad. In fact, I criticized the CDC early on for not warning people aggressively enough, and for not urging the public to do what the government was doing: prepare for the worst while hoping for the best. Now the CDC needs to keep warning people that the pandemic still might get bad – while telling people that so far it is remarkably mild.
Uncertainty is a central characteristic of an influenza pandemic. So candor about uncertainty is a central characteristic of pandemic communication.
The pandemic isn’t guaranteed to continue on its current course.
On one extreme, as we have discussed already, the pandemic virus could turn more virulent – even much more virulent.
On the other extreme, the pandemic could actually end up saving lives.
How is that possible? As has been true in most previous pandemics, the H1N1 pandemic virus seems to be crowding out the seasonal flu viruses. That too isn’t guaranteed. (Very little about influenza is guaranteed, except its unpredictability.) But in the northern hemisphere this past spring and summer, the seasonal strains pretty much disappeared (as they usually do in the summer), while the pandemic strain continued to circulate. Meanwhile, the southern hemisphere was having its June-August winter. Instead of a typical flu season, those countries in the southern hemisphere that do systematic influenza surveillance reported that nearly all of their flu cases and flu deaths were from the pandemic strain, not from any of the seasonal strains. And since the pandemic strain is less deadly so far than the worst of the seasonal strains (H3N2), most countries in the southern hemisphere (among the countries that do surveillance) reported fewer flu deaths than usual.
The CDC says there is very little seasonal flu in the U.S. so far; it’s nearly all pandemic H1N1. But there’s not usually much seasonal flu in late November. If this were a normal year, the flu season would be just barely beginning.
This isn’t a normal year. And no one knows yet if we’ll have a normal flu season or not. Here are some of the possibilities, in addition to the possibility that the pandemic virus could become more virulent:
- The pandemic virus recedes and eventually disappears, at least temporarily, while some or all of the seasonal strains end up circulating as usual. We face a pretty typical winter flu season with mostly just the seasonal strains.
- The pandemic virus remains pervasive enough to out-compete the seasonal strains. It doesn’t become more virulent, though maybe it becomes more pervasive as the weather gets colder. We face a milder-than-usual winter flu season with mostly just the pandemic strain.
- The pandemic virus remains pervasive but the seasonal strains pick up steam anyway. We face a bad winter flu season with both seasonal and pandemic flu strains co-circulating.
- The pandemic virus recedes and disappears, at least temporarily, but the seasonal strains have been knocked out, at least temporarily. We face virtually no winter flu season at all.
From what I’ve read, the experts seem to think the first three possibilities are all entirely possible, and they’re not ruling out the fourth. In other words, they haven’t a clue.
In the second and fourth of the four possibilities – the two with little or no seasonal flu this year – the pandemic will have saved lives in the U.S. (assuming the pandemic virus itself doesn’t get more virulent). Saving lives is about as mild as “mild” can get.
The possibility of little or no seasonal flu this year isn’t a secret – but it certainly isn’t something public health officials like to talk about, for fear of undermining seasonal flu vaccination. Public health officials have been avoiding talking about this possibility for months.
Starting in early November, the CDC began to acknowledge this possibility, at least in its weekly flu report: “It is too early in the influenza season to determine if seasonal influenza viruses will circulate widely or how well the seasonal vaccine and circulating strains will match.”
Jody Lanard and I discussed the “what if there’s no seasonal flu this year” question at some length in our September 26 update, “Overselling Seasonal Flu Vaccination in a Pandemic Season.” So I won’t belabor the point here.
But I do want to quote two key paragraphs from that update:
If the seasonal flu strains disappear, or mostly disappear, there will be lots of media stories about that fact in the months to come. People in the northern hemisphere will learn that flu experts knew it was a real possibility as early as April 2009, as soon as the new soon-to-be pandemic virus emerged. They will learn that the amount of seasonal flu in the southern hemisphere dramatically decreased in that hemisphere’s 2009 flu season – decreased in some countries to minuscule levels, as pandemic flu H1N1 dominated in country after country.
Then people (reporters, bloggers, politicians, citizens) are very likely to ask officials:
- Why did you push the seasonal flu vaccine so hard last fall?
- Why didn’t you at least tell us you didn’t know yet whether it would be necessary?
- Why didn’t you give us enough information to make our own informed decision whether to get the seasonal vaccine early or wait until more was known about the need for it?
- If swine flu suddenly disappeared, or looked like it was disappearing, you wouldn’t be urging so many people to get that vaccine, would you? Or would you?
The last bullet point is worth pondering. It would be an exaggeration to claim that swine flu looks like it’s disappearing, but it has been declining in the U.S. for several weeks now. Despite the downward trend, public health officials doubt that the pandemic virus will disappear when barely seven percent of the U.S. population have caught it so far. They expect to see more waxing and waning before a definitive wane. And they are certainly still urging people to get the pandemic vaccine as soon as it becomes available.
They’re almost certainly right to do so; it’s not over till it’s over, and the new flu virus will probably circulate at some level of virulence for years. But I hope officials will be aggressively candid about the evidence that the pandemic’s second wave may be ebbing. I hope they will base their case for pandemic vaccination on the uncertainty of the future, not on exaggerated claims about the seriousness of the present.
Here is the CDC’s weekly graph tracking the percentage of doctor visits that were for an influenza-like illness (ILI):
The graph demonstrates four points: (1) ILI doctor visits peaked higher during the second wave of the pandemic than during the last couple of flu seasons; (2) they’re much, much higher than usual so early in the season; (3) they took ten weeks to climb from trough to peak; and (4) for the last four weeks they have started precipitously downward, but it’s too soon so say whether they’ll continue down or turn around. (As I’ve already noted, the second point isn’t much of a point, since pandemics aren’t seasonal – though it’s true that cold weather tends to increase flu transmission.)
Based on earlier data pointing in this downward direction, CDC Director Thomas Frieden said in Congressional testimony on November 4: “It’s likely that the current wave of infection will peak, crest, and begin to decline before there are ample supplies” of vaccine. He added: “Whether there’ll be another wave of H1N1 between now and May and whether we’ll get a different strain, only time will tell.”
Frieden was testifying on the vaccine shortage. His prediction that the pandemic wave would soon “begin to decline” (before the vaccine supply was adequate) was interpreted as an admission of defeat vis-à-vis pandemic vaccination. This is pretty stunning when you think about it. The head of the CDC tells Congress that the second pandemic wave may be ending, and Congress is so preoccupied with vaccination program deficiencies that it sees this as bad news, not good news.
Maybe it is bad news after all. Maybe the pandemic’s ebb will make room for the more deadly seasonal flu to make a comeback. Nobody knows.
But for those who are focused on the pandemic itself, it’s got to be good news. Not only have the pandemic’s first and second waves both been mild. The second wave may already be ebbing. And there may be time to get vaccinated before another wave.
If the second wave does in fact continue to decline, there may, of course, be a third wave coming after it. The third wave may or may not be short. It may or may not be mild. But any way you look at it, the big pandemic news is this: So far, we have been very, very lucky. That’s the news – but it has not been the official message, and the mainstream media have missed it entirely.
Why Do We Have Only Estimates?
You may wonder why we have to rely on CDC estimates, instead of actual numbers.
The statistics I have been playing with in this update – case attack rates (CARs), case fatality rates (CFRs), and population mortality rates (PMRs) – require knowing two things about the disease in question:
- how many people in a particular population of known size catch it in some period of time; and
- how many of those people die from it.
The first number divided by the population size gives you the CAR (case attack rate); the second number divided by the first number gives you the CFR (case fatality rate); the CAR times the CFR gives you the PMR (population mortality rate). All you need to know is how many people get sick with the disease and how many die from it.
For influenza, pandemic or seasonal, there is simply no way to count the people who get sick from the disease. Here’s why:
- Lots of people have mild symptoms and don’t go to the doctor. They’re missed unless authorities do various types of surveys to pick them up.
- Others go to the doctor and are diagnosed with an “influenza-like illness” but don’t get a flu test. (Flu experts shorten “influenza-like illness” to “ILI”; the fact that they have extensive use for this abbreviation tells you how seldom they actually know whether a case is actually flu or some other ILI.)
- Still others get a screening test for flu, but not a more expensive and sensitive test to identify which kind of flu they have (or had). So once a pandemic has started you can’t be sure which cases are pandemic flu and which are seasonal flu unless you test for that – though nearly all such specific tests in the U.S. since the summer have either been positive for pandemic flu or negative for flu; there’s very little seasonal flu out there so far this year.
- Many of the tests, even some of the more expensive ones, have high rates of false positives and false negatives.
If you count only people who have a laboratory-certified case of influenza, you’re grossly underestimating the number of flu cases. And if you count everybody who recalls having an ILI, you’re grossly overestimating the number of flu cases. There are known to be people who had flu-like symptoms, got treated for flu, and when they were eventually tested turned out to have a bad rhinovirus (a cold). There are known to be people who had flu-like symptoms, figured it was a cold and just stayed home, and when they were eventually tested turned out to have flu. Obviously lots of people who are never tested may be getting misclassified.
So a few months ago, the CDC stopped counting flu cases (swine flu or seasonal flu), and reverted to flu surveillance and monitoring systems that are closer to its methods during non-pandemic years. It does careful laboratory analyses of small samples from around the country and then extrapolates. That in one oversimplified sentence is how it comes up with its estimates of the number of flu cases. On its website, the CDC offers a more thorough explanation of its multiple surveillance mechanisms.
Figuring out the number of flu deaths (again, pandemic or seasonal) raises some of the same problems: people who die without being tested or whose tests may not be accurate. But it also raises a different sort of problem. The number of flu deaths is an informed guess, mostly because flu victims don’t necessarily die of “pure flu.” They often die of a preexisting disease that the flu made worse, or they die of a new disease they got because the flu made them weak, or they die of the flu because other diseases made them unable to fight it off, or they die of several things at once including the flu. Even when it is established that someone got the flu and later died, whether to attribute that death to the flu is a judgment call.
The CDC has been estimating seasonal flu cases and deaths for years. But until the November 12 estimates were released, the CDC had only its tally of laboratory-confirmed swine flu cases and laboratory-confirmed swine flu deaths to go on.
Journalists loved these swine flu tallies, and used them endlessly, even though the CDC kept warning that the former number, especially, was way low because it omitted cases that had never been tested. (The World Health Organization still maintains worldwide tallies of laboratory-confirmed cases and deaths, and the media still dote on them, especially in developing countries.) A very low estimate of the number of swine flu cases so far made the pandemic look less pervasive than it actually was. It also made the pandemic look more deadly than it actually was, since the smaller number of recorded cases made for a higher apparent case fatality rate (not that journalists ever bothered to do the math).
From time to time various CDC officials tried to correct the record with seat-of-the-pants guesstimates of the “real” number of U.S. cases so far:
Although the CDC didn’t stress the point nearly as much, its tally of pandemic deaths was also lower than the real number, mostly because it relied on a strict definition of what constituted a death from pandemic flu – a definition that ruled out many deaths from pneumonia, organ failure, etc., brought on or exacerbated by influenza. By contrast, the CDC’s estimate of 36,000 average seasonal flu deaths includes these “flu-related” deaths. It seemed sensible to use the same criteria for both definitions.
Not that the CDC wanted to facilitate comparisons between pandemic deaths and seasonal flu deaths. It didn’t. It really didn’t. The November 12 press briefing that unveiled the new swine flu statistics never mentioned the 36,000 figure for seasonal flu – a notable omission, considering how often officials flog that figure when trying to persuade people to get the seasonal flu vaccine.
Although the 36,000 figure never came up at the November 12 briefing, the CDC’s Anne Schuchat did mention a much less commonly used number: the 3,600 people under 65 who die in an average flu season. Her point was that swine flu is tougher on the young than the seasonal flu:
If you think about, that only about 10% of the seasonal flu deaths occur in people under 65, that would be about 3600 deaths, we do think we are having a pretty severe amount of deaths so far from the h1n1 virus.
The fact that swine flu is somewhat more deadly to the young than the seasonal flu was featured often in the news briefing. The fact that it is much less deadly overall than the seasonal flu wasn’t mentioned.
But the November 10 New York Times “scoop” by Donald G. McNeil did use the 36,000 figure. Entitled “Recalculating the Tally in Swine Flu Deaths,” the article included this paragraph:
The new estimate will be a more accurate comparison to the 36,000 deaths from seasonal flu each year, [CDC spokesman Glen Nowak] said. That estimate is also based on confirmed cases as well as hospital reports of people who appear to have died after a bout of flu. Over 90 percent of seasonal flu victims are over 65, and many are bedridden or in nursing homes or have serious medical problems like cancer or heart disease that the flu worsens.
McNeil’s story stops short of directly comparing 36,000 annual deaths from the seasonal flu with 3,900 swine flu deaths in six months. The story does include both numbers (though it uses “about 4,000” instead of 3,900). It tells readers that the new CDC swine flu numbers are a lot higher than the old ones. It tells readers that the change isn’t a change in the pandemic, but in how pandemic cases and deaths are counted. It tells readers that the change will facilitate comparison to the seasonal flu. It tells readers the most important seasonal flu number for comparison. And then it doesn’t make the comparison.
Still, McNeil’s story comes closer than most. Like the CDC, most reporters didn’t focus on the new evidence that so far the pandemic was milder than the seasonal flu. They found other, more alarming aspects of the November 12 numbers to emphasize instead.
The Forbidden Word: “Mild”
Never once to my knowledge has anyone at the CDC pointed out publicly that so far this pandemic looks less deadly than the seasonal flu. Never once.
Of course CDC officials couldn’t have pointed that out back in May, when the limited early evidence from Mexico suggested that the pandemic was way more deadly than the seasonal flu. But by late July the tally of confirmed deaths already looked awfully low relative to the guesstimated number of cases – certainly lower than the analogous comparison for the seasonal flu – and still the CDC avoided saying so. It still isn’t saying so.
I understand at least some of officials’ reasons for hesitating to say so:
- The numbers are so squishy. Prior to the November 12 estimates, they were really squishy. Officials didn’t want to do math with seat-of-the-pants guesstimates – a textbook case of “garbage in, garbage out.” The numbers are presumably less squishy now, but still pretty squishy.
- The pandemic is a moving target. Even an accurate measure of the pandemic CFR so far wouldn’t constitute a firm prediction of the pandemic CFR in the months to come – but most reporters would undoubtedly interpret it as one. And many politicians would perceive it, or pretend to perceive it, as a promise – especially later if things get worse. Why give out a number if the number’s going to keep changing, and if people are going to misperceive and reify it?
- As we have seen, the pandemic isn’t actually milder than the seasonal flu for people under 65. The only reason it turns out milder than the seasonal flu overall is because it is enormously milder than the seasonal flu for the elderly, who are the principal seasonal flu victims. Children and young adults, by contrast, rarely die from the seasonal flu and somewhat less rarely die from the pandemic flu. Wouldn’t trumpeting the overall comparison, accurate though it is, mislead the majority under 65 into thinking they, too, were less at risk from the pandemic virus than from the seasonal flu?
- The CDC’s own vulnerability is high. If officials say anything now about how mild the pandemic is so far, they’re likely to be accused of trying to over-reassure the public … or of trying to wriggle out from accountability for having hyped the pandemic ever since last spring … or of trying to reduce people’s outrage at the inadequacy of the vaccine supply. They’re also likely to undermine preparedness efforts, including the vaccination program itself (when more vaccine becomes available).
- The worst-case scenario is still on the table. Although there are few if any signs of it yet, the pandemic H1N1 virus could still mutate or reassort into a more severe strain. If health officials state outright that the pandemic is “mild so far,” how many of us would lose track of the “so far”? And then if things turned horrific in the months ahead, how many of us would come to feel that we had been over-reassured and badly misled? Isn’t it better to let people overreact to the mild pandemic we have so far than to leave them even less prepared for the severe pandemic we might still end up with?
And as I have noted already, it’s almost impossible to explain the pandemic-versus-seasonal differences without first coming clean about the fact that the seasonal flu is a threat mostly to the elderly. That might undermine future seasonal vaccination campaigns. And consider how much damage such an admission could do to the credibility of public health agencies, which would be accountable for all those past seasonal vaccination campaigns that conveniently neglected to mention how seldom the flu kills people under 65.
If the CDC is going to explain that the pandemic is less dangerous so far than the seasonal flu, it will also have to explain that that’s not the case for people under 65. That will raise an obvious paradox: How can the pandemic be less dangerous than the seasonal flu overall when it is more dangerous than the seasonal flu for the bulk of the population, everybody under 65? To unravel the paradox, it will have to come out of the closet about the seasonal flu, admitting that in terms of deaths the seasonal flu is almost entirely a disease of the elderly.
Explaining all that wouldn’t just be embarrassing about past seasonal flu vaccine communications. It would also undermine the annual push for seasonal flu vaccination. The only way to avoid this chain of inferences is to shut up about the fact that the pandemic is turning out milder than the seasonal flu, and hope the media don’t out you.
I still think public health officials should come clean. Whether the media out them or not, if the pandemic stays mild the public will eventually realize it (many realize it already, even without the November 12 data), and will hold officials accountable for not having said so sooner. Not coming clean will damage official credibility far more than coming clean. But I do understand why coming clean will be very, very difficult.
Some officials will undoubtedly claim that they’ve been coming clean all along. After all, the CDC certainly acknowledges that 90% of seasonal flu cases are 65 and over. It’s right there on the CDC website for all to see … all who look. But when officials talk to the public, and especially when officials talk to the public about the importance of vaccination, “36,000 deaths a year” is a much more widely used statistic than “90% of them elderly.”
Even the CDC website reflects the bias. The remaining 10% of those 36,000 seasonal flu deaths, the ones who are under 65, add up to an average of 3,600 deaths a year. That’s the most relevant statistic for the 87.2% of the U.S. population that’s under 65. So search the CDC website for “36,000” and “influenza,” and then do it again for “3,600” and “influenza.” Most of the 36,000s refer to the annual average number of flu-related deaths; most of the 3600s do not refer to the annual average number of flu-related deaths in people under 65. They’re about something else entirely.
Is it possible that the CDC collected the new data about the severity of the pandemic, posted the data on its website, planned to discuss the data at that day’s press briefing … and never thought to use the data to calculate the pandemic’s case attack rate, case fatality rate, and population mortality rate so far, so it could compare those estimates to the analogous numbers for the seasonal flu?
I guess it’s possible. But it seems a lot likelier that the CDC did at least some of the calculations, realized that its data were telling it the pandemic is significantly milder than the seasonal flu so far … and decided not to say so – presumably for the reasons I have listed above, plus some others I haven’t thought of.
The November 12 CDC news briefing “explained” the new data in ways that look designed to emphasize the severity of the pandemic, not its surprising mildness.
For one thing, the CDC’s generally excellent briefer, Dr. Anne Schuchat, refreshingly used the word “pandemic” 22 times. In previous CDC briefings, the word has been used very sparingly; I have always assumed the reason was a fear at some level of government that “pandemic” might be an excessively scary word. On November 12, just when the data were showing that so far swine flu is much milder than the seasonal flu, Dr. Schuchat unleashed the P word.
A reporter responded to the new numbers by saying: “With these numbers seeming to triple literally overnight … it’s fair to say when they hear this, they [the public] will be quite alarmed. What is your message to the public, parents and adults, when they hear these new numbers?” This was a chance for Dr. Schuchat to say, no, actually these are very reassuring numbers. Here’s what she said instead, her whole answer to that question:
Influenza is serious. Vaccination is the best effort to protect one’s self or family. These efforts give a bigger picture of what’s going on and reaffirm the priority recommendations we’ve given. We focus vaccination on younger people because they are disproportionately affected with the virus. Things haven’t really changed from last week to this week; […] we’re finally able to update the public on how big a toll this virus is having so far. Of course, this is just the first six months and I am expecting all these numbers unfortunately to continue to [rise].
Another reporter actually asked about the comparison to seasonal flu, specifically regarding children: “I’m wondering at this point are you able to say definitively that this [pandemic] is producing more serious illness in more children than seasonal strains….” I have quoted Dr. Schuchat’s answer already, but here it is again: “If you think about, that only about 10% of the seasonal flu deaths occur in people under 65, that would be about 3600 deaths, we do think we are having a pretty severe amount of deaths so far from the h1n1 virus.”
In response to another question asking for historical perspective – another chance to say the pandemic is milder than the seasonal flu so far – Dr. Schuchat answered as follows:
We’ve been tracking influenza for decades. We have some systems that go back to 1958. Others of our systems are newer. What we are seeing in 2009 is unprecedented. People know we haven’t had a pandemic since 1957. So it’s not surprising that what we’re seeing is unprecedented. To have very high rates of influenza-like illness in September and October is extremely unusual. So I think the report in the MMWR focuses in on that. When we look back year after year, we don’t see a fall [like] this.
It’s certainly true that it would be unprecedented to have as much seasonal flu in the fall as we have pandemic flu this fall. But why would Dr. Schuchat consider this fact more noteworthy (and newsworthy) than the fact that we’re experiencing a pandemic that is killing far fewer people so far than the seasonal flu usually kills?
While Dr. Schuchat chose not to compare the overall swine flu death toll so far to the average seasonal flu death toll, she concluded the November 12 briefing by comparing it to the 1918 pandemic death toll:
What does this look like compared to previous pandemics. The estimates I’m giving you are the first six months. This is April through the middle of October. We have a long flu season ahead of us. In typical seasonal flu we see disease from December to May, it’s only November. So exactly what we will see as a full toll of illness from this pandemic is very difficult to say. I can say, though, that what we’re seeing with this h1n1 virus is nowhere near the severity of the 1918 pandemic. That caused much larger numbers six months in. I think projecting out forward is difficult. And we’re really keen to get vaccine given as rapidly as possible to those in greatest need so we can limit the full toll this pandemic takes. So thank you, everybody.
All things considered, it was courageous of the CDC to produce the November 12 numbers at all, and to feature them in its November 12 press briefing. Yes, the agency interpreted the new numbers chiefly as evidence that the pandemic is more pervasive and more deadly than previously reported, not as evidence that it is milder than the seasonal flu. But at least it produced the new numbers.
Perhaps in the weeks to come the CDC will find additional courage to interpret the numbers more candidly. Or perhaps state and local health officials will take up the task, even if the CDC does not. Or perhaps the media will give the numbers a second look. So far, I see no signs of any of these developments.
Notwithstanding all the reasons to avoid the word “mild,” something is stunningly wrong when the evidence says we’re facing a pandemic that is six times milder so far than the ordinary seasonal flu, and the government officials in charge of pandemic preparedness decline to tell us so.
“About Like the Seasonal Flu”
So have the media told us so? Very, very seldom – even after the CDC handed reporters the data on November 12.
I am not accusing the media of hyping the pandemic. The dominant media meme about pandemic severity has been that it’s “about like the seasonal flu.” Reporters keep hearing those words from local health officials, and keep repeating them. They seemed approximately true back in June, when there were no real data to go on. And they’re still approximately true – experientially – for the typical victim. Both kinds of flu usually lead to a miserable week in bed and then you’re better. But “about like the seasonal flu” misses three key facts about this pandemic:

- So far, overall, the pandemic is mild – killing fewer people than the seasonal flu usually kills, mostly because it kills far fewer people 65 and over, who are the main victims of the seasonal flu.

- But for children and adults under 65, the pandemic is actually deadlier than the seasonal flu (which isn’t very deadly for children and adults under 65). And the difference in deadliness may be greater for people with certain medical conditions, or for certain age groups within the under-65 cohort.

- All that could change. Nobody can estimate the odds that the pandemic will become more severe, perhaps catastrophically severe – but experts know that such a sudden change is far more likely with a new pandemic flu strain than with the constantly but gradually mutating seasonal strains.
“About like the seasonal flu” doesn’t just miss the first of these three key facts. It misses them all.
Both public health officials and journalists seem terrified of saying anything that suggests that so far the pandemic is a pussy cat, and equally terrified of warning people that it could become a raging tiger at any moment. They’re overstating how bad it is and understating how bad it could get.
When health officials and reporters say that the pandemic is turning out a lot like the seasonal flu, then, what do they think they mean?
- That it’ll probably kill around 36,000 people in a single year? That’s an awfully high guess, given the pandemic’s current behavior. Having killed 3,900 people in the first six months, it would have to kill another 32,100 (more than eight times as many) in the next six months to get to 36,000.
- That it’ll probably kill mostly the elderly? That would be a huge surprise.
- That it’s nearly guaranteed not to mutate suddenly into an enormously more dangerous form? That would be nice, if only it were so.
- That it’ll give most of its victims a really rotten feverish week and then they’ll be fine? That’s solid, at least so far.
More importantly, when officials and reporters say the pandemic is turning out a lot like the seasonal flu, what does their audience think they mean? I don’t know what percentage of the U.S. population actually realizes that the seasonal flu currently kills about 36,000 Americans a year, 90% of them elderly. I suspect most Americans would guess a far lower mortality figure and a far more balanced age distribution.
Maybe all the audience is getting out of the comparison is the part that’s actually so: Most pandemic patients, like most seasonal flu patients, feel awful for a week and then recover.
The more you know about the seasonal flu, the more misled you would be if you imagined that the swine flu pandemic resembles it.
Partly because most seasonal flu deaths are elderly, most seasonal flu deaths are virtually invisible. Of course every death is a tragedy for the loved ones left behind, but seasonal flu is the Rodney Dangerfield of diseases, unable to command the public respect that 36,000 annual deaths ought to command. So when a local official says the swine flu pandemic is similar to the seasonal flu, the official may mean “Wow, expect it to kill around 36,000 people!” But the public may hear: “No biggie. It’s just like a normal year.”
Perhaps that’s why so many comparisons to the seasonal flu say that the pandemic will probably be roughly as severe as a typical flu year, and then go on to explain why it should be considered worse than a typical flu year.
On August 7, 2009, for example, the President’s Council of Advisors on Science and Technology  (PCAST) stated: “The case-fatality ratio (i.e., proportion of infected individuals who die as a result of the infection) appears to be similar to seasonal influenza … perhaps 0.05 to 0.2 percent of all symptomatic cases.” PCAST went on to say that the pandemic would probably kill more people than the seasonal flu (because it would probably infect more people), and offered a “plausible scenario” for “planning purposes” of 30,000-90,000 deaths.
(PCAST) stated: “The case-fatality ratio (i.e., proportion of infected individuals who die as a result of the infection) appears to be similar to seasonal influenza … perhaps 0.05 to 0.2 percent of all symptomatic cases.” PCAST went on to say that the pandemic would probably kill more people than the seasonal flu (because it would probably infect more people), and offered a “plausible scenario” for “planning purposes” of 30,000-90,000 deaths.
It’s the 90,000 number that got most of the media coverage – not PCAST’s mistaken guess that the pandemic would have about the same CFR as the seasonal flu. Neither the reporters who were alarmed by the 90,000-deaths scenario nor the commentators who berated that scenario as alarmist noted that it was far from a worst case scenario.
Though the 90,000-deaths figure is way lower than any real worst case scenario, it is also way higher than the pandemic death toll will be if things stay the way they are. In fact, so is the low-end number in PCAST’s planning scenario. If things stay the way they are, the swine flu pandemic won’t kill 30,000 Americans during its first year either.
As far as I can find, the CDC itself has never come right out and said that the swine flu pandemic has or will have a case attack rate, case fatality rate, or population mortality rate similar to those parameters for the seasonal flu. But CDC officials have seemed comfortable with hundreds of other statements by health agencies, experts, and journalists equating pandemic H1N1 with the seasonal flu.
This comparison grossly overstates the current seriousness of the pandemic overall. It slightly understates the pandemic’s current seriousness for people under 65. And it irresponsibly ignores the possibility of a major change: a major change for the worse if the pandemic virus becomes more virulent, or a major change for the better if the pandemic remains mild and supplants the seasonal strains.
The comparison is thoroughly misleading to people who have a decent sense of what the seasonal flu is like. It’s very difficult to guess what it might mean to people whose impression of the seasonal flu is wrong to start with.
From time to time, even before November 12, some flu expert has expressed the view that that the swine flu pandemic might actually be milder than the seasonal flu – and managed to get a little media coverage for that view. On September 16, 2009, for example, Reuters ran a story about Marc Lipsitch of Harvard University, citing Dr. Lipsitch’s estimate that swine flu’s case fatality rate so far was somewhere between 0.007% and 0.045% – which nicely matches the 0.018% figure based on CDC estimates two months later. Even though the Reuters story explicitly compared Lipsitch’s much lower estimate to the conventional seasonal flu case fatality rate average of 0.1%, ABC News ran the story under the headline “Swine Flu Death Rate Similar to Seasonal Flu: Expert.”
It didn’t make much of an impression, and certainly didn’t alter the media meme that swine flu is about like the seasonal flu.
Off-Base Coverage of the November 12 Data
It is hard to blame the media for mishandling the pandemic-versus-seasonal story prior to November 12. Without the CDC to lead the way (and do the arithmetic), journalists weren’t about to calculate their own tentative CARs, CFRs, and PMRs based on the CDC’s case number guesstimates and its laboratory-confirmed death counts. Instead, they endlessly reported that the pandemic was about as severe as a typical flu season.
Then came November 12. At last the CDC had provided surveillance and monitoring data as a basis for estimating the severity of the pandemic, and for comparing it to the severity of the seasonal flu. But the CDC didn’t actually do the CAR, CFR, and PMR calculations, nor did it make the comparisons. Did the media?
No.
I have looked at virtually all the coverage in major national media of the CDC’s November 12 recalculation of the first six months of swine flu cases and deaths. Here are my overall conclusions:
- Nobody missed that this was just a recalculation, not a change. The CDC emphasized that point in its November 12 press briefing, and reporters got it right. Every story was at pains to explain that the pandemic hadn’t suddenly gotten worse.
- Nobody said the pandemic could in fact get worse. The possibility of an increase in virulence wasn’t mentioned at the November 12 briefing, so it wasn’t mentioned in the news coming out of that briefing. Reporters who cover the pandemic story routinely presumably know about that possibility, but they’re busy covering what has happened, not what could happen.
- Nobody used the CDC’s new numbers to calculate a case attack rate, a case fatality rate, or a population mortality rate. In fact, nobody calculated anything. Reporters cited the numbers (some of the numbers) they were given, period. Nobody did any arithmetic.
- Nobody said the new numbers were reassuring. The new numbers were higher than the previous tallies of laboratory-confirmed cases and deaths – so they had to be seen as alarming. The main thrust of virtually every story was: “This doesn’t mean things are worse than they were. But it does mean things are worse than the previous numbers suggested.” I counted alarming, neutral, and reassuring paragraphs in some stories to make sure my impression was accurate. Most paragraphs were neutral. But there were a lot more alarming than reassuring paragraphs.
- Direct comparisons to the seasonal flu were rare. Some stories did include the 36,000 figure for annual seasonal flu deaths, and some mentioned that seasonal flu kills mostly the elderly while the pandemic is killing mostly younger people. But very few stories tried to assess which was more serious – overall or for specific age groups. No story said the seasonal flu is much more deadly to the elderly than the pandemic is so far to any age group.
- One story (a blog, actually, by Jacob Goldstein on the Wall Street Journal website) explicitly said the new numbers might be seen as suggesting that the pandemic is milder than the seasonal flu. The story went on to detail the reasons why the author thought that conclusion would not be justified.
- Most stories implied that the pandemic is worse than the seasonal flu. The facts and statistics most frequently included in the coverage made this inference inevitable. Story after story, for example, stressed that the number of pandemic cases and deaths is “unprecedented so early in the season” – implying that the pandemic would probably get worse as the “season” progressed. Also much-reported was the estimate of pandemic pediatric deaths, and the fact that this number greatly exceeds both the previous count of laboratory-confirmed pandemic pediatric deaths and the count of laboratory-confirmed seasonal flu pediatric deaths.
- Many stories pointed out that the regular flu season hasn’t gotten started yet. Nobody wondered whether there would be a seasonal flu this year. And nobody noted that if the pandemic virus supplanted the seasonal flu strains and stayed mild, the pandemic would actually save lives – albeit the lives of the elderly. (Nobody raised the question of how many elderly deaths equals one pediatric death, though a few stories came close to implying that the seasonal flu mostly kills people who are on their deathbeds anyway.)
- Most stories dwelled on the new numbers fairly briefly, and then segued to the vaccine shortage and other pandemic issues that had been raised at the CDC’s press briefing.
Why have reporters failed to use the CDC’s November 12 numbers to show that the pandemic – based on the CDC’s estimates – is indisputably milder so far than the average seasonal flu? I don’t know. But three hypotheses seem likely to me:

Reporters (especially medical reporters) may be reluctant to stray off the reservation.
Interpreting a CDC story differently than the CDC interprets it – and differently than your peers are interpreting it – carries all kinds of risks: offending your sources at the CDC and elsewhere; complicating your relationships with other reporters; raising questions about your competence or your objectivity in the minds of your editors and your public.

Reporters (especially medical reporters) may be reluctant to undermine their own story.
Say you’ve been covering swine flu for weeks, or even for months. You’ve been selling your editors on its importance, pitching for more space or airtime to tell the story. Do you really want to be the one to say, oops, it’s not such a big deal after all, at least not yet?

Reporters (especially general assignment reporters) may simply not realize what the numbers mean.
Much has been written about the "two cultures" of words and numbers; journalists are word people, and mostly pretty innumerate. It’s easy to imagine a reporter, perhaps even a medical reporter, looking at the numbers, listening to Anne Schuchat’s November 12 briefing, and never realizing what the numbers are saying that Dr. Schuchat isn’t saying.
Reuters ran four stories on the new CDC numbers. They pick up nearly all the themes in my summary above, so I want to analyze all four. Then I’ll look at a couple of other typical stories. I will conclude with Jacob Goldstein’s Wall Street Journal blog, the only example I have found in the mainstream media that used the November 12 data to explore the possibility that the H1N1 pandemic might actually be milder than the seasonal flu.
The first Reuters story moved at 3:33 Eastern Time on November 12. Here’s its lede:
WASHINGTON (Reuters) — Swine flu is causing the worst flu season in the United States since 1997, when current measurements started, and has killed an estimated 3,900 people from April to October, U.S. health officials reported on Thursday.
The “worst flu season” theme was justified several paragraphs later:
“Nationwide, the percentage of visits to health-care providers for influenza-like illness was higher than that observed at the peak of any seasonal influenza season since ILINet (the CDC’s reporting system) was implemented in its current form in 1997,” the report reads.
In September and October the number of people hospitalized for flu was as high as usually seen by the end of an entire average flu season – which runs from October through April in the United States.
The second of these two claims is false. The CDC estimates U.S. seasonal flu hospitalizations at 200,000 a year – the vast majority of them in the winter flu season. The CDC’s November 12 estimate of the first six months of swine flu hospitalizations was just 98,000 (63,000–153,000). Nor is it true that a higher percentage of swine flu cases have been hospitalized so far than the percentage of seasonal flu cases usually hospitalized. For swine flu, 98,000 hospitalizations out of 22 million cases is a hospitalization rate of 0.44%. For the seasonal flu, 200,000 hospitalizations out of 31 million cases is 0.65%.
The first claim is true. Pandemic ILI doctor visits peaked higher than flu season peaks. Not mentioned, however, is another, far more important truth: The 3,900 deaths in the story’s lede are a long, long way short of the death toll in an average flu season, far less the worst flu season.
At 5:24 p.m. Reuters moved a “factbox” with all the new numbers. Two initial paragraphs put the numbers in this context: The pandemic is worse than the seasonal flu. But the numbers don’t mean it’s getting worse than it was, only worse than we thought:
(Reuters) — New estimates suggest the pandemic of H1N flu is far worse than an average influenza season, with at least 22 million infections and 3,900 deaths, according to the U.S. Centers for Disease Control and Prevention.
The new estimates are extrapolations based on detailed data for April-October from 10 states and do not reflect a worsening of the pandemic, the CDC stressed. Following are the figures released by the agency, with the median number of cases followed by the full potential range….
At 5:51 p.m., Reuters moved an update by reporter Maggie Fox. The new story stresses that the pandemic has already killed more children than the seasonal flu usually kills.
WASHINGTON, Nov 12 (Reuters) — H1N1 swine flu killed an estimated 3,900 Americans from April to October, including more than 500 children, U.S. health officials said on Thursday….
“I have already seen a larger number of [pediatric] deaths than we have had for several years,” the CDC’s Dr. Anne Schuchat told reporters. “I do believe the pediatric death toll from this pandemic will be extensive and much greater than what we see with seasonal flu.” …
The CDC said swine flu is causing the worst flu season in the United States since 1997, when current measurements started.
“What we are seeing in 2009 is unprecedented,” Schuchat said. “Influenza is really serious. The vaccines we have are the best way to protect patients.” …
Much later in the story, Fox does point out that the average flu season kills about 36,000 Americans. How does she interpret the difference between 36,000 and 3,900? These three short paragraphs are fascinating, and worthy of annotation:
In an average flu season, about 36,000 Americans die and 200,000 are hospitalized. But 90 percent of these are people over 65. [“But”? So the deaths of 32,400 seniors don’t count for much?]
With H1N1, the opposite is true – 90 percent of those infected and seriously ill are younger adults and children. [This sounds like the pandemic goes after younger people, doesn’t it? But 87.2% of the U.S. population is under 65 – so it’s hardly surprising that about 90% of pandemic cases and deaths are too. The pandemic isn’t singling out the young. The seasonal flu singles out the old.]
And Schuchat pointed out that it is only November. “We have a long flu season ahead of us,” she said. The U.S. flu season usually runs from October to May. [But the pandemic hasn’t been seasonal so far; it started in April – and may or may not get worse with the cold weather. Even as Schuchat was speaking and Fox was writing, the second pandemic wave appeared to have already peaked, whether that ultimately turns out true or not.]
At 5:53 p.m., Fox posted a blog entry under the title “Is swine flu getting worse?” Her answer:
No, says the U.S. federal government, but officials finally have enough data to give a good picture of the pandemic and it isn’t pretty. The CDC estimates that 22 million Americans caught swine flu in the first six months of the pandemic and 3,900 people died.
This includes 540 children.
So why the big jump in numbers? In a country of 300 million people, it takes some time to do a count. The US doesn’t have an organized public health system and states and cities lack enough staff to crunch the numbers in real-time. So the CDC takes a representative, detailed sampling from 10 states and then extrapolates this to the total US population. The latest figures are the first to give a good estimate of how extensive the pandemic is so far.
At least Fox’s blog doesn’t say the pandemic is more severe than the seasonal flu (though it surely doesn’t say it’s milder). This time Fox’s point is that the pandemic is more severe than we thought.
Steve Sternberg’s story in USA Today sounded many of the same themes. I’ll annotate this one too:
Swine flu has swept through about 22 million Americans from April to October, killing an estimated 3,900 people, including 540 children, health officials said Thursday.
The analysis represents the government’s latest effort to assess a viral outbreak that in just six months has flooded emergency rooms and intensive-care beds in at least 48 states that have reported widespread flu cases. With flu season just beginning, an estimated 98,000 people have been hospitalized, according to the Centers for Disease Control and Prevention (CDC). [Again, the fact that the normal flu season is just beginning is only marginally relevant to predicting the course of the pandemic.]
“We’ve been tracking influenza for decades,” says Anne Schuchat, director of the CDC’s National Center for Immunization and Respiratory Diseases. “What we are seeing in 2009 is unprecedented.” [Well, yes, there hasn’t been a pandemic since 1968. In that sense 2009 is unprecedented. Is the number of deaths so far unprecedented? It would be unprecedented this early in a normal flu season – which is what the Schuchat quote seems to be implying. But if you consider the pandemic an out-of-season flu season, it’s killing fewer people and a smaller percentage of cases than the flu usually kills. That’s unprecedented. Where is it in the story?]
What the numbers don’t reveal is what will happen next, because no one knows yet when the flu season will hit its peak or how many waves of cases to expect, says Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases. [Better. Of course the pandemic second wave (which isn’t a season) may have hit its peak about when this story was written. But the main thing the numbers don’t reveal is whether the virus will become more virulent during the course of the pandemic. No November 12 story even mentions that question – the main question in the minds of experts all over the world.]
The new national estimates are extrapolations of data drawn from a CDC emerging-diseases network of hospitals, laboratories and health departments in 10 states and from reports of hospitalizations and deaths, Schuchat says. They illustrate the extent to which swine flu, also known as H1N1, is hitting children, who account for 8 million infections, 36,000 hospitalizations and 540 deaths. In a typical flu season, about 80 children die. [Yes, the pandemic is killing more children than a typical flu season kills – though this apples-and-oranges comparison of 540 estimated pandemic pediatric deaths with 80 laboratory-confirmed seasonal flu pediatric deaths exaggerates the difference. The right comparison is estimated to estimated or confirmed to confirmed. What’s really missing here, though, is the fact that swine flu isn’t actually deadlier to children than to, say, seniors. Seasonal flu is enormously deadlier to seniors than to children.] …
In a typical flu season, which ends in May, 90% of deaths and hospitalizations involve people 65 and older. The H1N1 outbreak began in April; 90% of those who become infected and need medical care are younger than 65. [Of course, just under 90% of the U.S. population is younger than 65 too.]
Schuchat urges people who appear to be getting severely ill and those with chronic conditions and asthma to quickly see a doctor. Antiviral drugs, such as Tamiflu and Relenza, are most effective when given soon after symptoms set in, she says. What worries her most is that flu season has barely begun: “We have a long flu season ahead of us.” [Does Schuchat think the pandemic “season” has just begun? As Fauci pointed out earlier in the story, there’s no basis to think this is so … or not so. Or is Schuchat worried that we’ll get a normal flu season (of seasonal flu strains) on top of the pandemic? That’s hardly an argument that the pandemic is severe.]
The following Associated Press story by Lauran Neergaard is better than most. It doesn’t say the pandemic is worse than the seasonal flu.
WASHINGTON — Estimates of deaths caused by the swine flu have grown to nearly 4,000 since April, roughly quadrupling previous estimates. But that doesn’t mean swine flu suddenly has worsened.
Instead, the federal numbers made public Thursday reflect a long-awaited better attempt to quantify the new flu’s true toll. Most cases still don’t require a doctor’s care.
Swine flu has sickened about 22 million Americans since April and killed about 540 children.
And it’s still early in the season. [What season? Again the assumption seems to be that the pandemic will keep getting worse as the weather gets colder. That’s certainly possible, perhaps even likely, but it’s not a foregone conclusion.]
“I am expecting all of these numbers, unfortunately, to continue to rise,” said Dr. Anne Schuchat of the Centers for Disease Control and Prevention. “We have a long flu season ahead of us.” [Well, yes, cumulative totals do tend to rise. But they have been rising more slowly over the past few weeks. Basically, nobody has a clue how much they’ll rise. And nobody has a clue how long the second pandemic wave will last, whether and when there will be a third wave, or whether the seasonal flu will arrive on schedule or be preempted by the pandemic strain.] …
In a typical winter, seasonal flu strains cause 200,000 U.S. hospitalizations and 36,000 deaths, the vast majority in people over 65. Seasonal influenza doesn’t usually start circulating until November. Swine flu began a big climb in September, leading to what CDC called unprecedented high levels of illness so early in a season – and no way to know when the flu will peak. [If you read carefully, this puts Schuchat’s “unprecedented” quote in the proper context: unprecedentedly early for a flu season, not unprecedentedly deadly. But Neergaard still doesn’t make the point that the pandemic is less deadly than the average seasonal flu.]
Finally, let’s look at Jacob Goldstein’s Wall Street Journal blog. Its headline is promising: “Putting 22 Million Cases of Swine Flu in Context.”
Goldstein starts with “a few quick numbers: 22 million cases, 98,000 hospitalizations, 3,900 deaths,” then explains that the numbers are approximate, based on uncertain estimates. Then comes the key paragraph:
Uncertainty aside, how do the estimates for H1N1 compare to seasonal flu? At first blush, it looks relatively minor. While 22 million sounds like a very large number (7% of the entire population), the CDC also says that in a typical year anywhere between 5% and 20% of the population gets the seasonal flu. In that context, 7% doesn’t sound so big. Similarly, 3,900 deaths pales next to the 36,000 deaths a year attributed to seasonal flu.
Reading this graf, I was ready to applaud – though “at first blush” made me nervous. Goldstein actually did some arithmetic to arrive at the 7% figure, and then he compared it to the seasonal flu’s 5-20%. And he stuck 3,900 and 36,000 in the same paragraph – the only reporter to do so.
Then Goldstein takes it all back:
But there are a few really big caveats to those comparisons. For one thing, the six months the CDC is looking at are usually flu’s off-season, when there’s very little of the virus going around. “What we are seeing in 2009 is unprecedented,” Anne Schuchat, a senior doc at the CDC, said on a conference call today. “If we look back year after year, we don’t see a fall like this.” So we’ll have to wait until the traditional big flu months this winter to see what happens with H1N1, and how it compares with seasonal flu.
Another key caveat is the different population getting hit hard by H1N1. While the very old are typically among those hit hardest by seasonal flu, H1N1 is taking a bigger toll on children and adults between the ages of 18 and 64. “The pediatric death toll from this pandemic will be extensive and much greater than what we see with seasonal flu,” Schuchat said.
Both caveats are true. We don’t know what the winter will bring, and the pandemic isn’t killing almost exclusively the elderly the way the seasonal flu does. But neither caveat, in my view, undermines the truth Goldstein started with. It is a truth the CDC, local health officials, and the vast majority of journalists have either missed or ignored: Compared to the average flu season, the swine flu pandemic isn’t especially widespread so far, and it is amazingly mild.
If the pandemic virus remains at its current level of virulence, what would it take for this pandemic to be as deadly as the average flu season (albeit deadly to a different cohort of victims) by the end of its first twelve months?
As we have seen, the pandemic’s current case fatality rate is about 0.018% – 3,900 estimated deaths out of 22 million estimated cases so far.
So if the pandemic does not become more or less virulent – that is, if its case fatality rate remains at about 0.018% – how many people would it have to infect in order to kill 36,000 of them? In other words, 36,000 is 0.018% of what number? The answer is 200 million.
The pandemic has already infected an estimated 22 million people in the U.S. 178 million to go.
The current U.S. population is 308 million. For the pandemic to infect 200 million of them by the end of its first year, it would have to achieve an annual case attack rate of 65%. That would be truly unprecedented.
My wife and colleague Jody Lanard assisted on this update.
On December 15, I posted an “Update on the December 2 Update” commenting on four topics related to this December 2 update:
- The uncomfortable reaction of many public health professionals to the update
- Flaws they pointed out in the update
- Increased media attention to the pandemic’s mildness
- Continuing CDC interpretations – misinterpretations, in my view – of its own pandemic severity data.
Also on December 15, I posted a new update, commenting on new estimates of pandemic cases, hospitalizations, and deaths released by the CDC on December 10.
November 18, 2009
U.S. Pandemic Vaccine Supply and Distribution:
Addressing the Outrage
by Peter M. Sandman and Jody Lanard
 We set out to write a “Swine Flu Pandemic Communication Update” on the pandemic vaccine shortage, the resulting outrage, and how best to manage it. But it turned out too long for an update, so we upgraded it to a column. Here’s a very brief summary for the “Update” archive.
We set out to write a “Swine Flu Pandemic Communication Update” on the pandemic vaccine shortage, the resulting outrage, and how best to manage it. But it turned out too long for an update, so we upgraded it to a column. Here’s a very brief summary for the “Update” archive.
As in most other developed countries, the fall rollout of the U.S. pandemic vaccination program has been hampered by a shortage of vaccine. The result is outrage.
Some of the outrage is about the shortage itself. That’s nobody’s fault; the vaccine virus turned out to be difficult to grow.
Some of the outrage is about betrayed expectations. Officials are very much at fault for overpromising, having frequently predicted that there would be ample vaccine by mid-October, and only occasionally warned that the prediction might not pan out if everything didn’t fall into place perfectly. Even before the pandemic began, in fact, the meme was established that it would require only three to six months after the emergence of a pandemic influenza strain to manufacture sufficient vaccine.
And some of the outrage is about how the limited vaccine supply is being distributed. The two key distribution issues so far:
- Unfairness and line-jumping – with complaints focusing on why some doses ended up going to Wall Street bankers, Guantanamo detainees, and similarly undeserving recipients.
- Chaos and confusion – with complaints focusing on how difficult it is to figure out who has vaccine, how frustrating it is to try to get any, and how disruptive the whole thing has been to health care providers.
Managing public (and health care provider) outrage about vaccine supply and vaccine distribution has thus become an important pandemic risk communication task, a necessary distraction from the paramount task of convincing people to get vaccinated.
Officials have done a good job managing some aspects of the outrage. The CDC, for example, was far more candid about predicting that vaccine distribution would be “a bumpy road” than it had been about predicting that there might not be enough vaccine as early as the schedule called for. Other aspects of the outrage have been badly managed so far. Government “apologies” for overpromising about vaccine supply, for example, came out sounding more like scapegoating Big Pharma than actually owning up to official over-optimism.
A number of outrage management strategies could help officials cope better in this situation. Among them: dilemma sharing, empathic identification, and the risk communication seesaw.
For the longer – much longer – version, read the column.
September 26, 2009
Overselling Seasonal Flu Vaccination in a Pandemic Season
by Peter M. Sandman and Jody Lanard
 Seasonal influenza vaccination campaigns have started in the U.S., at least a month earlier than in most years. Some doctors, including our own internist, had seasonal vaccine on hand by late August.
Seasonal influenza vaccination campaigns have started in the U.S., at least a month earlier than in most years. Some doctors, including our own internist, had seasonal vaccine on hand by late August.
The main reason for starting seasonal flu vaccination early this year is the ongoing swine flu pandemic. The pandemic vaccine won’t start becoming available in the U.S. until some time in October. National and state public health officials understandably want to get as much of the labor-intensive seasonal vaccination effort as possible out of the way before the even more labor-intensive pandemic vaccination effort starts. Individual practitioners are similarly motivated to avoid having to manage both potential rushes at once.
And it makes sense for patients too. If you know you plan to get the seasonal vaccine, you might well want to get your shot out of the way before your doctor or clinic is inundated with pandemic vaccinees – or, worse yet, pandemic flu patients. And if you know you’re planning to get both vaccines, you might well want to space out the two vaccinations, just in case there might be some good reason for spacing them out.
So if we assume that people should get vaccinated against the seasonal flu, doing so early is perfectly sensible.
But there are three reasons why it might be smarter to wait – reasons that the U.S. Centers for Disease Control and Prevention (CDC) and most other public health agencies in the U.S. and elsewhere are not yet acknowledging publicly.
They’re not keeping these three reasons secret. After all, we learned about them exclusively from public sources, including lots of CDC sources. But they’re not shouting them from the rooftops – and they are shouting from the rooftops that people should get their seasonal flu shots now.
When people belatedly find out about these three reasons, the result may well be mistrust and outrage. How much mistrust and outrage will depend on how significant the three reasons turn out to be over the next several months.
We are not asserting that the three reasons we’re about to discuss mean people should forgo the seasonal vaccine this year, nor that they mean the CDC should stop urging people to go get vaccinated. Those are medical and public health policy questions beyond our expertise as risk communication consultants.
We are asserting something more moderate, and more in our field: that it is a huge mistake for the CDC or any public health agency to urge people to go get vaccinated against the seasonal flu ASAP without first making sure they are aware of the three new arguments against early vaccination.
1. Displacing the seasonal flu
The biggest of the three reasons for hesitating to get vaccinated against the seasonal flu: There may not be much seasonal flu this year.
Or there may be. No one knows. Here’s what we do know:
- In previous pandemics, the pandemic strain has typically supplanted the seasonal strain, becoming the new seasonal strain – or at least the new dominant seasonal strain; some existing seasonal strains may stay in circulation as well. It’s not clear how often the process has happened quickly (early in the pandemic) versus gradually (by the end of the pandemic). What’s clear is that a new pandemic flu strain usually out-competes preexisting strains (at least influenza A strains), sooner or later. Thus the 1918–1920 pandemic strain, an H1N1, became seasonal after 1920, replacing an earlier influenza A strain. The 1957–1958 pandemic strain, an H2N2, became seasonal after the 1957–1958 pandemic, replacing the H1N1 strain that had circulated since 1918. The 1968–1969 pandemic strain, an H3N2, became seasonal after that pandemic, replacing H2N2. On the other hand, in 1977 an “almost pandemic” 1950-type H1N1 strain (thought to have escaped from a laboratory) did not replace H3N2, but has coexisted with it … at least until the 2009 pandemic.
- CDC surveillance is currently showing 99%+ novel H1N1. That is, there is virtually no seasonal flu in circulation in the U.S. right now.
- The CDC changed its pandemic flu case definition, for hospital reporting purposes, on August 30. It now wants hospitals to assume that any flu case is a pandemic H1N1 case. It no longer asks them to send in samples for typing, and it no longer recommends typing in order to choose the right antiviral medications for patients. In evolving epidemics and outbreaks, case definitions sometimes change repeatedly, as happened during SARS. Still, the change in the pandemic flu case definition implies, to us at least, that the CDC thinks it’s likely that there won’t be much seasonal flu for a while.
- In most other countries (especially in the southern hemisphere) that have seen competition between seasonal flu strains and the new pandemic strain, the pandemic strain is winning. In some, including Australia and New Zealand, it has almost entirely won already. In others, there is still some significant circulation of seasonal H3N2, coexisting with pandemic H1N1. The World Health Organization recently reported
 that between June and August there were “regional outbreaks of influenza A(H3N2) in China” and numerous other countries. Nonetheless, the WHO report makes clear that overall the pandemic strain is supplanting either all or very high percentages of the seasonal strains.
that between June and August there were “regional outbreaks of influenza A(H3N2) in China” and numerous other countries. Nonetheless, the WHO report makes clear that overall the pandemic strain is supplanting either all or very high percentages of the seasonal strains.
- On August 21, WHO issued a pandemic update
that stated:
It has been noted throughout the temperate zones of the southern hemisphere, which are now passing out of their winter season, that when pandemic H1N1 began to circulate, the relative importance of seasonal strains, represented by H3N2 in nearly all countries, rapidly diminished and pandemic H1N1 became the dominant strain. Some seasonal H1N1 strains were reported but were even less common than seasonal H3N2. It is too early to tell if this co-circulation of multiple strains will continue into the coming season of the Northern Hemisphere but it appears very likely that pandemic H1N1 will be the dominant influenza virus in the early part of the winter months.
- WHO recently proposed the strains to be used in the 2010 southern hemisphere vaccine. WHO recommending replacing the seasonal H1N1 strain with pandemic H1N1, though it continued to specify an H3N2 and an influenza B.
Of course flu is unpredictable. It wouldn’t be a shock if the seasonal flu reappeared in strength this year, despite the facts summarized in these bullet points. On the other hand, it wouldn’t be a surprise at all to have little or no seasonal flu this year.
(Little or no seasonal influenza A, at least. We haven’t been able to figure out the extent to which pandemic influenza, which is always influenza A, tends to supplant seasonal influenza B.)
Instead of candidly acknowledging that the pandemic might reduce or eliminate the 2009–2010 flu season, most health officials – especially local health officials – are over-confidently promoting the urgent need for the seasonal flu vaccine. Here are four examples:

- “[J]ust because a novel virus has arrived doesn't mean the seasonal ones have gone away,” a Salt Lake Valley (Utah) health official said. “They’re always circulating and mutating and always with us.” The reporter paraphrased the official as adding that “there really is no excuse for not getting a [seasonal] flu shot.” But in fact the seasonal strains in the U.S. have virtually gone away at this point. And if previous pandemics are any guide, they may well stay away (at least the influenza A strains).

- Even more creatively, a county health official in Illinois said the seasonal flu vaccine is “especially important this year because there’s a concern that H1N1 will mutate and combine with the seasonal flu viruses and will make the H1N1 more transmissible. We don’t know that for sure, but that’s certainly a concern.”

- New York City’s health department just released a health bulletin entitled, “Prevent Influenza: Get vaccinated!”
 It says: “Anyone who wants to avoid seasonal flu should be vaccinated. The yearly seasonal flu vaccine is especially important for people in these groups….”
It says: “Anyone who wants to avoid seasonal flu should be vaccinated. The yearly seasonal flu vaccine is especially important for people in these groups….”

- Finally, on September 24, CDC spokesman Tom Skinner said, “We believe it is advantageous for seasonal and 2009 H1N1 vaccines to be taken as soon as available.”
None of these seasonal flu vaccine promotional statements, nor any other U.S. seasonal flu promos we have collected, mentions the possibility that there may be very little seasonal influenza around this season. Officials are pushing the seasonal flu vaccine as if the seasonal flu strains were definitely going to be a major player in the 2009–2010 flu season.
If they turn out wrong, they are setting themselves up for further public outrage and mistrust, when the public belatedly discovers that the seasonal flu has mostly disappeared – and that officials knew that might very well happen but chose not to say so for fear of undermining their seasonal vaccination campaign. This can only do further damage to official credibility about vaccines – all vaccines.
It’s not like the public won’t notice if the seasonal flu goes away.
If the seasonal flu strains disappear, or mostly disappear, there will be lots of media stories about that fact in the months to come. People in the northern hemisphere will learn that flu experts knew it was a real possibility as early as April 2009, as soon as the new soon-to-be pandemic virus emerged. They will learn that the amount of seasonal flu in the southern hemisphere dramatically decreased in that hemisphere’s 2009 flu season – decreased in some countries to minuscule levels, as pandemic flu H1N1 dominated in country after country.
Then people (reporters, bloggers, politicians, citizens) are very likely to ask officials:
- Why did you push the seasonal flu vaccine so hard last fall?
- Why didn’t you at least tell us you didn’t know yet whether it would be necessary?
- Why didn’t you give us enough information to make our own informed decision whether to get the seasonal vaccine early or wait until more was known about the need for it?
- If swine flu suddenly disappeared, or looked like it was disappearing, you wouldn’t be urging so many people to get that vaccine, would you? Or would you?
2. A possible bad match
Official credibility about vaccines is a precious and endangered resource. Preserving credibility requires absolute candor, not overselling. Most officials know that in principle. But their sense of urgency about getting people vaccinated routinely overcomes their commitment to providing balanced information and letting people make up their own minds. Vaccination ardor too often overcomes vaccination candor.
Even in normal years, many officials oversell the seasonal flu vaccine, making over-promising statements about its benefits. We have written about this extensively before.
One of the most common ways of over-promising is to imply (usually without actually lying) that flu vaccines always or nearly always work. From time to time a patient complains: “I got the flu vaccine but then I got the flu anyway. So I’m not going to get vaccinated next year.” Officials usually try to rebut that impression this way: “You may have gotten the flu shortly after getting the vaccine, before your body had a chance to build up antibodies in response to the shot. Or you may have had a flu-like illness that wasn’t actually the flu.”
What usually doesn’t get said? “Well, the flu vaccine is only 70 to 90 percent effective in healthy young adults – much less effective than most other familiar vaccines. And it’s worse than that in the elderly and people with compromised immune systems. And some years one or more of the circulating flu strains mutates a bit between the time when we start manufacturing vaccine and the time when you actually get your shot. If a strain has drifted and the vaccine is no longer a good match, getting vaccinated will provide less protection against that strain – sometimes no protection at all.”
When you read most flu vaccine promotional materials (and we read reams of them), you get a clear impression that the vaccine will prevent you from catching the flu. Even if the language is technically correct, an ordinary intelligent interested person gets an unduly optimistic impression of the vaccine’s potential benefits. Neither beforehand (when you’re deciding whether to get vaccinated) nor afterwards (when you catch the flu after having been vaccinated) do the experts routinely clue you in that the flu vaccine is less reliable than most other vaccines people get in the U.S. On a societal level, it saves thousands of lives. But on an individual level, at its best – when there’s a good match between circulating strains and the strains in the vaccine – it protects only 7 to 9 out of every 10 healthy young people who roll up their sleeves for it.
This year’s seasonal flu vaccine has three different components in it – one aimed at seasonal H1N1 (different from pandemic H1N1), one for seasonal H3N2, and one for influenza B. Of the three seasonal flu strains that the vaccine is designed to help you fight off, the most dangerous is H3N2. It is usually H3N2 that causes a “bad” flu season. And it is H3N2 that is responsible for most flu-related deaths in people 65 and over – which is about 90% of total flu-related mortality in most non-pandemic years.
There are signs that the currently circulating strain of H3N2 may be drifting away from the “vaccine strain.”
As of September 5, the CDC reported that only 5% of all H3N2 samples tested in the U.S. during the 2008–2009 flu season (which ends officially on October 4) had shown reduced responsiveness to the current vaccine strain. As of September 12, just one week later, the CDC said the cumulative percentage had risen to 13%.
Other countries are also reporting increasing evidence of H3N2 drift away from the vaccine strain.
On September 10, between those two CDC weekly reports, Wall Street Journal medical reporter Betsy McKay wrote:
[CDC and WHO officials] are also monitoring the emergence of a new variant of a long-circulating seasonal flu strain, called H3N2, which is associated with more hospitalizations and deaths among the elderly than other strains. The variant has been identified on several continents and now makes up about 20% to 30% of H3N2 viruses analyzed in WHO labs, Dr. Zhang [WHO flu expert Wenqing Zhang] said.
That percentage is much smaller in the U.S.: The new variant currently makes up only about 5% of tested H3N2 viruses, said Nancy Cox, the CDC’s influenza chief. “It’s a very small proportion,” she said.
In these two paragraphs, the WHO flu expert was talking about recent H3N2 viruses from all around the world – 20% to 30% had drifted, to some extent, from the vaccine strain. The CDC flu expert was talking about U.S.-only H3N2 viruses from the entire 2008–2009 flu season (October 2008 to September 2009) – only 5% had drifted. Because the CDC’s Dr. Cox used a cumulative statistic, the reporter got the impression that the U.S. might be an exception to the worldwide trend of a higher and higher proportion of variant H3N2, not well matched to the vaccine strain. In reality, the trend is occurring in the U.S. as well.
A couple of weeks later, WHO upped the proportion of “recent” variant H3N2 samples even more, reporting on September 23  : “The majority of recent [H3N2] viruses were antigenically and genetically distinguishable from the [H3N2] vaccine viruses.” As of August 2009, the September 23 report said, at least two countries (China and New Caledonia) still had widespread outbreaks of H3N2 influenza, and several countries had regional H3N2 outbreaks. So H3N2 hasn’t disappeared, though it is waning in many countries where the pandemic strain dominates … and the H3N2 that is left is an increasingly bad match for the H3N2 component of the seasonal vaccine.
: “The majority of recent [H3N2] viruses were antigenically and genetically distinguishable from the [H3N2] vaccine viruses.” As of August 2009, the September 23 report said, at least two countries (China and New Caledonia) still had widespread outbreaks of H3N2 influenza, and several countries had regional H3N2 outbreaks. So H3N2 hasn’t disappeared, though it is waning in many countries where the pandemic strain dominates … and the H3N2 that is left is an increasingly bad match for the H3N2 component of the seasonal vaccine.
In the same September 23 report  , WHO announced the recommended flu strains for the southern hemisphere’s 2010 influenza season. It recommended dropping the current seasonal H1N1 strain completely, and replacing it with the pandemic H1N1 strain. It also recommended replacing the seasonal H3N2 strain that is in this year’s vaccine with the drifted H3N2 strain that seems to be becoming more prevalent. WHO, in short, is betting that within six months the drifted H3N2 will be a bigger threat than the dominant circulating H3N2 strain from 2008–2009, against which the current 2009–2010 vaccine is meant to protect.
, WHO announced the recommended flu strains for the southern hemisphere’s 2010 influenza season. It recommended dropping the current seasonal H1N1 strain completely, and replacing it with the pandemic H1N1 strain. It also recommended replacing the seasonal H3N2 strain that is in this year’s vaccine with the drifted H3N2 strain that seems to be becoming more prevalent. WHO, in short, is betting that within six months the drifted H3N2 will be a bigger threat than the dominant circulating H3N2 strain from 2008–2009, against which the current 2009–2010 vaccine is meant to protect.
Remember, 99%+ of recent CDC flu samples are pandemic H1N1, not any seasonal strain, drifted or otherwise. But an increasing percentage of the few seasonal H3N2 samples collected are turning out to be a less-than-ideal match with the 2009–2010 seasonal vaccine.
It’s too soon to predict with any confidence that the 2009–2010 seasonal vaccine will turn out to be a bad match for H3N2. As we have seen, it’s too soon to predict with any confidence whether there will even be much H3N2 circulating. But the gradually accumulating evidence suggests that if the northern hemisphere does see a significant return of seasonal strains in 2009–2010, the seasonal vaccine may provide less protection than usual against the most dangerous of those strains. In other words, if there is a lot of seasonal H3N2 this year, the current flu vaccine may be a poor match for some or much of it as the season progresses.
A significantly drifted seasonal flu strain can emerge before or during any flu season, after it is too late to alter that season’s vaccine. But we don’t always have such early hints that it may be happening.
By mid-October, officials should have a better sense of how much H3N2 is circulating, and how much of that H3N2 has drifted to the point where the seasonal vaccine is a relatively bad match (and maybe even how bad a match). Mid-October is when U.S. flu vaccination campaigns have traditionally been launched.
In a normal year, then, officials wouldn’t have launched an early seasonal vaccination campaign in anticipation of the pandemic vaccination campaign to come. They would have more time to figure out how serious the H3N2 mismatch issue was likely to become. Then, in principle, they could use this information to help them decide how aggressively to promote the vaccine. And if they were candid about the extent of the drift, prospective vaccinees (particularly those in low-risk groups) could use the information to help them decide whether to bother to get vaccinated that year.
We realize this is an idealistic formulation. Officials never want to give people reasons why they might not want to get a seasonal flu shot in any particular year. In a normal year, flu vaccine campaigners rarely even mention signs of potential vaccine mismatches. We saw this last season, when the circulating influenza B strains in Canada and the U.S. looked like (and turned out to be) a bad match with the influenza B vaccine component. Long after it was clear that the circulating lineage of influenza B was unrelated to the vaccine component, we kept collecting official statements that the vaccine was a “good match.” No nuance; not even “2 out of 3 ain’t bad, especially since the match with H3N2 is good.”
So pandemic year or not, you probably wouldn’t be hearing much about H3N2 drift from public health officials, especially in their vaccination promotional efforts. Again, we need to stress that the information we’re reporting in this update isn’t secret; we got most of it from weekly flu reports issued by the CDC and health agencies in other countries. A few reporters have written stories about H3N2 drift. But most people who are hearing (and perhaps heeding) the message to get their seasonal shots early are not hearing that there are signs suggesting the vaccine may provide little protection against the most dangerous of the circulating seasonal strains.
If the potential mismatch comes to pass (and if there is much H3N2 circulating this coming season), people will learn later that officials knew about it when they were busily promoting early vaccination, but downplayed it in order not to risk undermining the seasonal vaccination campaign with an inconvenient truth. This will predictably and justifiably further undermine the credibility of official vaccination campaigns. The underlying message will be: “We’ll tell you all the good reasons to get vaccinated, overemphasize the vaccine’s efficacy, and downplay uncertainties and hints of potential bad matches. Why? Because we really want you to get vaccinated more than we want you to make your own well-informed decision about vaccination.”
This is disrespectful to the public. Yes, trying to convey the uncertainties is difficult. And some people just want to be told what to do. Others want to preserve their unduly confident sense that “science” is more definite than it is. But officials should not cave in because of this. There is already an abundance of evidence that publics end up distrusting officials who oversell vaccines.
3. Could the seasonal flu shot be dangerous?
So far we have discussed two reasons why people might want to wait awhile to decide about getting a seasonal flu shot this year:
- There might be little or no seasonal flu this year.
- If there is some seasonal flu, it might become obvious in another month that the vaccine is likely to be a bad match for the most virulent seasonal strain, H3N2.
Both of these reasons have to do with the efficacy of the seasonal vaccine. The question they raise is whether you might be wasting your time, money, and effort getting a shot that might not be needed this year, or might not work very well this year.
Opponents of vaccination typically focus not on vaccine efficacy but on vaccine safety. They insist that vaccines are dangerous, and to them the seasonal flu vaccine is no exception. We think most of their arguments about the risk of vaccination are wildly overblown and some are outright dishonest, though others do have a germ of truth. We think the seasonal flu vaccine is pretty safe – far safer than the flu – and we get our flu shots religiously every year (though we have decided to wait awhile this year). Of course even a tiny risk of a serious adverse reaction becomes more worthy of consideration when the compensating benefit starts to look smaller than usual.
But that’s not the point of this section.
There is apparently some evidence that the seasonal vaccine might increase people’s vulnerability to the pandemic H1N1 strain. A Canadian study currently undergoing peer review is said to show this effect. The data were shared with several high-level officials (at least in Canada). News of the study was also leaked to the media, presumably by someone who thought its worldwide public health implications were too serious to await the slow process of professional journal publication.
The Canadian study isn’t a prospective study – the gold standard for medical research. But its authors are very reputable flu experts, not vaccination opponents.
After the leak, numerous national and international experts and officials – some on the record, some off – commented on the study’s reported findings.
A CDC spokesperson told the Canadian Press that “the scientists at the Centers for Disease Control and Prevention have not seen this effect in [surveillance and monitoring] systems we have reviewed in the United States.”
On September 24, Canadian Press medical reporter Helen Branswell wrote:
Complicating the issue is the fact that scientists elsewhere have looked for a similar effect but have failed to see it. The U.S. Centers for Disease Control has said it finds no evidence of this and Kieny [WHO vaccine expert Marie-Paule Kieny] said British and Australian researchers have also drawn a blank when they searched their data.
Kieny said it is important to study the data with an open mind. “If there is something, it’s better that it comes out. I think one needs to keep open eyes and a fresh mind and look in all fairness to the results.”
Like WHO’s Dr. Kieny, most officials speaking publicly about the rumored results of the Canadian study sounded dubious but refreshingly respectful about it. They thought the results were unlikely to prove right. But many noted that influenza constantly surprises us. And most emphasized that the results deserved rapid and thorough examination, because of their possible implications for the massive seasonal flu vaccination campaigns that have already begun in many places.
That’s not to say that experts were happy to see any public discussion of the possibility that seasonal flu vaccination might increase a vaccinee’s pandemic risk. The overall tone of official comments, not surprisingly, suggested that the Canadian study deserved immediate expert attention just in case it might turn out to have merit. But in the meantime members of the public should go ahead and get their seasonal flu shots – preferably without having heard about what came to be called in official (and journalistic) circles “the Canadian problem.”
There is one small published study from Australia that looked for a relationship between seasonal vaccination status and subsequent infection with pandemic H1N1. It is just about the only actual data we have found on the matter – as opposed to quotations from various countries’ officials saying they haven’t seen any evidence that seasonal vaccination makes people likelier to catch the pandemic flu.
In the Australian study, the authors reported that they looked for but found no statistically significant evidence that people vaccinated against the seasonal flu had a reduced risk of catching pandemic H1N1. The Australian study report does not mention the question raised by the Canadian study: Were vaccinated persons more likely to get pandemic H1N1? But the study results appear to show a statistically insignificant “benefit” (our word) from seasonal vaccination in most age groups, and a statistically insignificant “harm” (our word) from seasonal vaccination in one age group. Bottom line: no evidence of benefit or harm.
As all researchers know, it is hard to prove a negative. The Australian study didn’t find that seasonal vaccination decreases or increases vulnerability to pandemic H1N1. That’s a long way from putting the issue to rest. But the Australian study is compatible with prior influenza research, whereas the Canadian study, if it turns out valid, would be a new and surprising wrinkle.
We don’t know what data the CDC and other health agencies around the world may have accumulated bearing on the startling possibility that seasonal flu vaccination might make vaccinees likelier to catch pandemic flu. As far as we know, no study other than the Canadian study was designed specifically to investigate this possibility. But there may be data sets more robust than the Australian data set that go a long way toward settling the question. And there may be studies – peer-reviewed or not; published or not – that contain additional information of relevance.
It would be helpful in light of the Canadian study if governments with relevant data would make their data public, rather than asking the world to take their word for it.
Worst case: The seasonal vaccine turns out not only unnecessary this year, or not only ineffective against the most virulent seasonal flu strain – but actually dangerous, by increasing vaccinees’ susceptibility to pandemic H1N1. This could cause a fiasco (like the 1976 swine flu vaccination campaign) that shadows all influenza vaccination for a generation or more. And, most important, it could kill people.
That’s the worst case. How likely or unlikely is it? To answer that question now, you have to weigh the reassurances of public health officials based on evidence that you haven’t seen against the results of a study that you also haven’t seen (and most of them haven’t either). Or you could wait to get your seasonal flu shot until more evidence is available.
The bottom line
We are not influenza experts. We will defer to the experts on whether it is good public health policy for the CDC to keep promoting seasonal flu vaccination this year, despite all of the above.
And we’ll defer also on whether it’s good public health policy to keep promoting early seasonal flu vaccination. That decision puts a very high priority on getting one vaccination program at least partially out of the way before the other one gets started. It puts a lower priority on waiting a month or so while we see whether a flu season starts to materialize, whether the H3N2 turns out to be a decent match if it does, and whether there is further evidence bearing on the Canadian researchers’ finding.
As ordinary people in a high-risk group for seasonal flu who have always gotten our flu shots every year, we are both waiting this year. But we are not qualified to offer an opinion on the public health implications of the CDC’s decision to move full-speed-ahead now.
We do want to comment, however, on the risk communication implications of the CDC’s moving full-speed-ahead now – especially moving full-speed-ahead without aggressive public acknowledgment of the three factors that prospective vaccinees might want to consider before deciding whether to roll up their sleeves or wait.
If there is a strong public health case for getting vaccinated now instead of waiting to see how things develop, the CDC and other public health officials should make the case, explaining why that case trumps the three arguments we have discussed. But it is a serious risk communication error for public health officials to make a case for seasonal flu vaccination – and early seasonal flu vaccination – without acknowledging the ways in which the contrary case is uniquely strong in this pandemic year.
Updated: August 21, 2009
Talking about Pandemic H1N1 Vaccination
by Peter M. Sandman
 This month, August 2009, the U. S. CDC is sponsoring a series of eleven swine flu vaccination “public engagement” meetings, facilitated by the Keystone Center. As Keystone explains:
This month, August 2009, the U. S. CDC is sponsoring a series of eleven swine flu vaccination “public engagement” meetings, facilitated by the Keystone Center. As Keystone explains:
The CDC is asking for public discussion, deliberation and input as the agency considers whether to simply make vaccines available to those seeking immunization, to promote vaccination to those most at risk or to implement a widespread immunization program.
The main purpose of the meetings, I assume, is to hear the questions and comments of stakeholders – stakeholders, not the general public: the sorts of people who choose to spend a summer Saturday at a swine flu vaccination meeting (not to mention the sorts of people who find out about such meetings in the first place).
A secondary purpose may be to prepare to respond to the concerns stakeholders, critics, and the general public are bound to have as the U.S. gets closer to a swine flu vaccination rollout. The meetings may well end up having a bigger impact on pandemic H1N1 vaccination messaging than on pandemic H1N1 vaccination policy, though of course the two are connected.
The most important vaccination policy question the CDC faces is the same one every government with some pandemic vaccine to distribute faces: deciding which priority groups should get first shot. Although all governments have access to pretty much the same data, they aren’t all making the same decisions.
- Everybody is prioritizing people whose health conditions make them likelier than others to have severe, life-threatening cases: people with asthma, immunocompromised people, pregnant women, etc.
- Although there was talk early on about prioritizing people most needed to sustain societal infrastructure (cops, firefighters, water treatment technicians, and the like), most of that has died down, because the pandemic virus is mild so far and serious absenteeism problems have yet to surface anywhere in the world. Unless there’s an increase in virulence, the prioritization will be about preventing flu deaths, not keeping society going.
- There is disagreement over how high a priority to put on three groups: the elderly, who are far less likely to catch this particular flu strain but are more likely to have serious cases if they do; children, who are major sources of transmission and whose deaths are more disturbing than the deaths of adults; and healthcare workers, who are likely to have close contact both with patients who are already infected and with patients who have other health conditions that make them especially vulnerable.
Telling the public who’s at the front of the vaccination line – and why – is certainly a messaging task. But that’s not the big messaging question. The big messaging question is how aggressively to urge people to roll up their sleeves. Should the CDC and officials in other countries with vaccine supplies be offering pandemic vaccination or pushing pandemic vaccination? (There is little if any support for requiring pandemic vaccination, except for healthcare workers in some jurisdictions.)
I vote for offering.
Vaccination Promotion, Resentment, and Psychogenic Illness
To understand why, first consider the likely effects of a pandemic vaccination program on people who don’t get what they want out of the program:
Some people who want to get vaccinated but can’t are likely to:
- overvalue the vaccine;
- resent not getting vaccinated;
- assume that any respiratory illness they get is swine flu;
- experience that illness as more severe than it would otherwise seem;
- demand more in the way of treatment; and
- blame the authorities for failing to acquire enough vaccine and choosing to vaccinate others instead of them.
Some people who don’t want to get vaccinated but feel pressured into doing so are likely to:
- undervalue the vaccine;
- resent the pressure to get vaccinated;
- assume that any illness they get is a side-effect of the vaccine;
- experience that illness as more severe than it would otherwise seem;
- demand more in the way of treatment; and
- blame the authorities for pushing them to get vaccinated.
The more aggressively health officials urge people in the prioritized categories to get vaccinated, the larger both of these two unhappy groups will be, and the stronger both groups’ reactions will be.
That is, when officials strongly push asthmatics, pregnant women, and so forth to get vaccinated, they will increase the number of such people who do get vaccinated – including the number who get vaccinated despite feelings of reluctance (alongside those who are successfully persuaded that getting vaccinated is a really good idea). That’s the purpose of pushing, after all. For those who get vaccinated despite continuing reluctance or ambivalence, moreover, the aggressiveness of the campaign will tend to increase the strength of their resentment at having been pushed, and will thus tend to increase the number who later become convinced that they’re suffering from vaccination side-effects.
It’s important to understand this second effect. People who are gently advised to get vaccinated and decide to go along will end up convincing themselves it was worth doing; that’s how cognitive dissonance works. But people who are pushed hard don’t need to tell themselves that vaccination is a good idea; they can simply tell themselves they did it because they were pushed hard. The most effective persuasion therefore applies enough psychological pressure to get people to do what you’re asking, but not so much that they experience themselves as complying rather than deciding.
Meanwhile, each dose administered to a reluctant vaccinee from a prioritized group will mean one less dose available for a more enthusiastic would-be vaccinee from a non-prioritized group. And each aggressive reiteration of the case for vaccination will strengthen the fervor and frustration of those for whom no dose is available. Thus an aggressive and appropriately targeted campaign will simultaneously increase the desire of some non-prioritized people to get in and decrease the number of such people who can get in. The predictable result is more people who will end up convinced that not getting vaccinated did them irreparable harm – many more than the actual number who will actually be harmed.
Note that the first group – people who want to get vaccinated but can’t – will include most of the population of the developing world, where there will be very little available vaccine for the foreseeable future. If developing countries somehow acquired a plentiful supply of pandemic vaccine, it’s hard to know how much public enthusiasm there would be for actually getting vaccinated. Mass vaccination programs in the developing world are often only modestly successful despite some pretty high-pressure communication campaigns. Skepticism is often widespread about the efficacy and safety of the vaccine – and even about the good intentions of the Western donors who finance such mass vaccination programs.
That’s when vaccine is available. The West has pledged to donate only small amounts of pandemic vaccine to the have-not countries, whose governments have (wisely) decided they have higher priorities for their own meager public health budgets. So the people of those countries won’t face the question of whether to say yes or no to pandemic vaccine. No pandemic vaccine will be on offer, leaving them free to assume – often with their governments’ encouragement – that the pandemic vaccine is a major lifesaver the selfish West is refusing to share.
An aggressive vaccination advocacy campaign in the West obviously won’t help ameliorate the developing world’s chronic case of pandemic vaccine envy – but it probably won’t hurt much either. Even if the vaccine-flush countries downplay their vaccination programs, and even if pandemic vaccination turns out pretty unpopular in the developed world, the developing world will still seethe with resentment that rich countries are protecting themselves while leaving their poor neighbors to suffer and die from the dreaded swine flu. Some officials in developing countries have privately said that they would rather have no vaccine at all (and thus keep citizen resentment directed outward at the West) than just a little vaccine (focusing citizen resentment on local elites who will be perceived as getting what little vaccine there is, whether that is true or not).
As for the second group – people who don’t really want to get vaccinated but feel pressured into doing so – the resentment will probably be particularly virulent for two subgroups:

- healthcare workers, because the pressure on them to get vaccinated is less for their own benefit than for the benefit of their patients; and

- parents of prioritized children, because so many of them are already anxious about the ever-growing number of pediatric vaccinations, and because much of the available vaccine supply will contain thimerosal, which some parents worry (I believe wrongly) might be linked to autism. (In the U.S., the CDC says, “enough thimerosal-free vaccine in pre-loaded syringes will be available for young children and pregnant women.”)
In short, aggressive pro-vaccination messaging is likely to yield more resentful vaccinees overly preoccupied with vaccine side-effects, and more resentful non-vaccinees overly preoccupied with pandemic H1N1 itself. The vaccine will of course cause some actual adverse reactions as well, and the pandemic will continue to cause some actual severe illnesses. Both numbers are still unknown, though the second will surely be much larger than the first. Both numbers will end up inflated by resentment.
Among the predictable results of aggressive pro-vaccination messaging, then, are these: more psychogenic illness, more mistrust, more litigation, and more hostility toward government vaccination programs and public health in general.
The Case for a Softer Sell
Well, okay, that’s unfortunate. But won’t aggressive pro-vaccination messaging also save lives by persuading more of the most vulnerable people to get vaccinated? Yes, it will. There are exceptions, of course – people for whom pressure leads more to obstinacy than to compliance. But the pressure is bound to succeed more often than it backfires. (That’s certainly the general belief about vaccination persuasion campaigns.) Assuming the pandemic vaccination communication effort is effective, it will get more people to say yes to vaccination. And assuming the pandemic vaccine is effective, that will reduce mortality and morbidity.
The question is whether the public health gain from persuading reluctant vaccinees is sufficient in this instance to justify the public health loss from pressuring one group while excluding another. If pandemic H1N1 were very virulent – more virulent than it currently is, even for people in the high-risk groups – the answer would clearly be yes. On the other hand, if pandemic H1N1 were very virulent, the number of reluctant vaccinees would also be tiny. The benefits of pressure would obviously be worth the cost (assuming the vaccine is effective) … and pressure would be largely unnecessary anyway.
But if nothing changes significantly, what we will have in a few months is a vaccine that many will see as hurriedly manufactured and hurriedly tested, deployed against a disease that is very contagious but very mild – milder than the average seasonal flu. To sell a mass vaccination program under those circumstances, considerable pressure may be necessary … and the benefits of that pressure may not justify the damage it will do.
Please remember that I am not talking about physical damage caused by the vaccine, which is likely – though not guaranteed – to be about as safe as the regular flu vaccine. A high-pressure pandemic vaccination promotion campaign may save some lives from pandemic H1N1. It may also drive a potentially larger number of people away from life-saving flu vaccine and other vaccines over the longer term – and diminish trust and confidence in public health officials across the board.
The fact that controversy over one vaccination campaign can taint public acceptance of other vaccines is well-known to professionals in vaccine communication. Kristine Sheedy of the CDC’s National Center for Immunization and Respiratory Diseases, Office of Health Communication, put it this way in a May 2007 PowerPoint slide on “Truths that can Make Marketing Influenza Vaccine Difficult”  :
:
Truth: Issues with flu vaccine impact parental acceptance of other childhood vaccines and vice versa….
Negative coverage of flu vaccine effectiveness came up frequently in discussions with parents about the necessity and effectiveness of infant immunizations….
I’m not advising officials to sound like they have no opinion on whether or not people should get vaccinated against pandemic H1N1. People rightly expect public health officials to have an opinion on public health decisions. As far as I can tell, most experts genuinely believe that most people (and especially people in the prioritized groups) are better off vaccinated than not. So they should say so – clearly but not very urgently. This situation calls for a health education approach (experts provide objective information so people can make an informed decision) rather than a more aggressive style of precaution advocacy (officials strongly promote what they believe is best, though people are free to do as they wish).
Moreover, I would advise officials to explain why they aren’t pushing pandemic vaccination as aggressively as they sometimes push other health measures. The best risk communication approach is for officials to say that they believe pandemic vaccination is a good idea, especially for people in the prioritized groups, but that they do not consider it so compellingly important, so urgent, that people with doubts or concerns need to overrule themselves and get vaccinated anyhow.
Recommend vaccination – but don’t push it hard. And say the reason you’re not pushing it hard is because so far it’s just not important enough to justify trying to talk people out of their reservations and anxieties.
I think most doctors and public health officials will dislike this advice. Doctors and especially public health doctors prefer to decide what’s best, and then urge the patient (or the public) to do it.
Doctors understand that some medical decisions are tough calls. They understand that in such situations they have an obligation to be candid about their uncertainty and to leave the final decision in the patient’s hands. Still, most doctors prefer to make a strong recommendation, even when the medical evidence is mixed.
And in this case the medical evidence won’t be mixed. Assuming the vaccine passes its safety and efficacy trials, it will be clear that pandemic vaccination is medically preferable to going without, especially for people in the high-risk groups. The case for not making a really strong recommendation on behalf of pandemic vaccination won’t be that the medical evidence is mixed. The case will be that the medical preference for vaccination, though obvious, isn’t very pressing – that it isn’t as important as trying to make sure that as many people as possible who want to be vaccinated get vaccinated; that as many people as possible who would rather not, don’t; and that as few people as possible end up believing that their health was damaged because they couldn’t get a vaccination they wanted or because they were pressured to get a vaccination they didn’t much want.
It is understandably difficult for doctors, and especially public health doctors, to endorse that view.
An aside: In the U.S., there is considerable official ambivalence about how strongly to signal overall concern about the H1N1 influenza pandemic. The United States Government officially calls the virus “novel H1N1” rather than “pandemic influenza H1N1” – avoiding the word “pandemic” as often as possible. (The “CDC Novel H1N1 Vaccination Planning Q&A” web page, posted on August 10, 2009, does not contain the word even once.) It will be interesting to observe the CDC’s decisions about how strongly to urge vaccination against something it doesn’t even refer to as a pandemic virus.
Communication professionals at the CDC understand the dilemma. In a PowerPoint presentation on “Guiding Principles for Pandemic H1N1 Influenza Communication,”  the CDC’s Director of the Division of Media Relations, Glen Nowak, wisely points out that “consumer demand for ‘choice’ will likely exceed consumer demand for H1N1 vaccine.” My extrapolation of Nowak’s point: If we can’t have it we’re likely to want it. If we’re pressured into getting it, we’re likely to resist it. And if we’re offered it without pressure, we’ll make whatever choice we make – and are far less likely to misinterpret the sequelae of our decision.
the CDC’s Director of the Division of Media Relations, Glen Nowak, wisely points out that “consumer demand for ‘choice’ will likely exceed consumer demand for H1N1 vaccine.” My extrapolation of Nowak’s point: If we can’t have it we’re likely to want it. If we’re pressured into getting it, we’re likely to resist it. And if we’re offered it without pressure, we’ll make whatever choice we make – and are far less likely to misinterpret the sequelae of our decision.
At a July 22 H1N1 communication meeting sponsored jointly by the Pan American Health Organization and the U.S. Department of Health and Human Services, Nowak expanded on the paradoxes of choice. If we have enough H1N1 vaccine doses for everyone, he pointed out, most of them may very well go unused. But if our supply is severely limited, the demand is likely to shoot through the roof.
Since the PAHO/HHS meeting, officials have announced that the U.S. novel H1N1 vaccine supply will not be as robust as hoped. Officials originally anticipated 120 million doses by October 15. Now they expect only 45 million by that date. Since two doses are required for adequate protection, that’s enough vaccine to protect only 22.5 million Americans, around 13% of the population. They hope for a lot more by the end of October.
Meanwhile, in a Washington Post/ABC News poll conducted August 13–17, respondents were asked whether they thought “you or someone in your household” would get a swine flu vaccination once it became available. 55% said yes; 41% said no; and 4% had no opinion. Other respondents were asked what they would do if their doctors recommended vaccination; that brought the percentage of yeses up to 65%, the nos down to 32%.
Respondents weren’t partitioned into those in prioritized groups versus those not in prioritized groups. But it’s probable that there were plenty of prioritized people among the 32% who wanted to say no even if their doctors urged yes, and plenty of non-prioritized people among the 55% who wanted to say yes without regard to what their doctors might think. In other words, there will be plenty of people likely to feel victimized either by pressure or by exclusion.
How will scarcity affect these numbers? Past flu vaccine scarcity problems have led to short-term runs on the vaccine, as people who had never especially wanted to get vaccinated suddenly decided to spend hours in line waiting for a shot. That’s what happened in 2004, for example, when manufacturing problems led to a shortfall in the U.S. seasonal flu vaccine supply. (See my column with Jody Lanard on “Flu Vaccine Shortage: Segmenting the Audience.”) Scarcity replaced pressure as a sufficient motivator for many people in prioritized groups to get vaccinated. As for the non-prioritized part of the population, the CDC asked them to stand aside voluntarily. We’ll never know how many would have done so, because state governments instantly converted the CDC request into official orders. I haven’t seen any data on how much resentment resulted from these orders.
It’s worth noting that there wasn’t a huge increase in flu vaccine demand in the year following the shortfall, compared with the year before the shortfall. So the prioritized people who stood in line for a shot in 2004 weren’t back in droves in 2005. And if getting frozen out in 2004 led a lot of non-prioritized people to feel an unaccustomed yen for flu vaccination, they were apparently over it by 2005.
My best guess: Pandemic vaccine scarcity will make it easier to talk prioritized people into deciding they want to get vaccinated, and harder to talk non-prioritized people into deciding they don’t mind doing without.
Will the scarcity environment make people in prioritized groups so amenable to vaccination that they don’t need to be pressured, or so responsive to the pressure that they don’t resent it? Or will it make officials so anxious to make optimal use of each dose that they exert even more pressure and incur even more resentment? It’s hard to predict.
In an August 2009 survey of nurses in the United Kingdom, 37% said they would get vaccinated against the pandemic, 30% said they wouldn’t, and 33% were undecided. Nurses are a prioritized group in most places, including the U.K. So that’s one prioritized group, at least, where it’ll probably take some considerable pressure to get the results officials are aiming for – and where the pressure is likely to incur the kinds of costs I have been worrying about. A proposed rule that would require vaccinations for healthcare workers in New York is generating a lot of pushback from the unions. Any bets on the likely frequency of side-effect allegations among healthcare workers forced to roll up their sleeves against their will?
If you merge Nowak’s focus on supply with my concern about messaging, you come up with the following risk communication worst case scenario:

- Officials urgently emphasize the importance of making optimum use of each dose since the supply is so limited.

- People in the prioritized groups are strongly pressured to get vaccinated as soon as possible.

- Everyone else is ordered to stand aside until more vaccine becomes available.
An alternative, “better case” scenario: Just give prioritized people the opportunity to get vaccinated first, and explain clearly why they are being given that opportunity. Then offer whatever vaccine is left after a certain date, if any, to people who aren’t prioritized. Save slightly fewer lives from this relatively mild pandemic flu virus. And pay a much lower price in vaccine safety controversy, psychogenic illness, future drops in vaccination rates, lost trust, and damaged public health relationships.
Specific Messages
To avoid the worst case and aim for the alternative scenario, I suggest the following pandemic H1N1 vaccination messages.
I have drafted these messages to be used once at least limited amounts of pandemic vaccine have become available. But of course communication shouldn’t wait till then. With minor changes in verb tense, the messages can be used immediately. They are written with the United States and other developed countries in mind. Vaccination messaging for countries with little or no vaccine will need to be very different.

So far, the pandemic H1N1 virus causes mostly mild disease.
We expect H1N1 to infect very large numbers of people – one-third or more of the population, based on our experience with the past few influenza pandemics. But nearly all the people it infects will experience mild symptoms. Some will experience no symptoms at all; they won’t even know they were infected. On the other extreme, some will get extremely sick, and some will die. But most will have respiratory symptoms for a few days, with or without aches and fever, and then they’ll be fine again. So far, if the CDC’s estimated case numbers and confirmed death counts are close to accurate, pandemic H1N1 is turning out milder and less deadly than the average year of the seasonal flu, although most of those dying are far younger than most seasonal flu victims.

The pandemic H1N1 vaccine is almost certainly a very safe vaccine.
(I am assuming that nothing alarming emerges from vaccine safety trials that are ongoing as I write this.) All vaccines have side effects, but the flu vaccine has very few. Nonetheless, some people are understandably concerned because the pandemic H1N1 vaccine was developed and tested very quickly. Others are understandably concerned because some versions of the vaccine – approved for use in some countries – relied on new cell-based vaccine manufacturing techniques instead of the tried-and-true egg-based method, or on new chemicals (called adjuvants) to boost the effectiveness of the vaccine, or on the mercury-containing preservative thimerosal that continues to be controversial despite strong safety evidence. Still others are understandably concerned because of serious side effects that are thought to have resulted the last time there was a rushed project to develop a human vaccine against a novel swine flu virus – in 1976, against a different H1N1 virus that in the end didn’t even launch a pandemic.
It is impossible to say with certainty that nothing unexpected will happen, that the vaccine developed from this swine-bird-human hybrid H1N1 virus won’t end up different in some way from other influenza vaccines … some way that does damage subtle enough that the safety testing misses it. We will be watching carefully to discover any such surprises fast once the mass vaccination program begins.
We are not saying the pandemic vaccine is risk-free. We are saying it is considerably lower-risk than the pandemic virus itself.

Almost everybody is better off vaccinated than unvaccinated against the pandemic virus.
But assuming no change in virulence, the decision doesn’t matter much for most people. This is a vaccine that is almost certainly safe, which will reduce your chances of catching a disease that will probably be mild. If you’re not pregnant, asthmatic, immunocompromised, or in some other high-risk group, the chances that the pandemic H1N1 virus will make you seriously ill are low. The chances that the pandemic H1N1 vaccine will make you seriously ill are far lower. On balance, everyone except people with known allergies to a vaccine ingredient is better off vaccinated than unvaccinated. We think the medical benefit of the vaccine is worth the hassle of two trips to the doctor.
But for some people getting vaccinated isn’t just a hassle. Some people are more anxious about the pandemic vaccine than they are about catching pandemic influenza – and anxiety is medically harmful too. If you don’t want to get vaccinated, or get your child vaccinated, we are not pressuring you to do so.
There are times when doctors strongly urge their patients to get past their anxiety and take some action that is medically important. So far, this is not one of those times.

The case for vaccination is stronger for people in high-risk groups.
If you’re pregnant, asthmatic, immunocompromised, or in one of the other high-risk groups, your chances of getting very sick if you catch the pandemic flu are higher than for most people. Still, even for you the odds are good that the disease will be mild if you catch it. Because there is a stronger case for vaccinating people in these high-risk groups than for vaccinating other people, and because we don’t yet have enough vaccine for everyone, we are making it available to people in the high-risk groups first. But we would rather vaccinate someone who wants to be vaccinated than someone – even someone in a high-risk group – who is reluctant to be vaccinated. So people in the high-risk groups get first dibs. But if you’re more worried about the vaccine than you are about the disease, feel free to decline and let the dose that is temporarily being held for you go to someone else instead. You may get a chance to rethink that decision if vaccine is still available later in the year.
This position is highly controversial among doctors and public health professionals. So it’s important to be really clear. Our medical advice to people in the high-risk groups is unequivocal: We advise you to get vaccinated against the pandemic flu. The vaccine could save your life. But getting you vaccinated is not so urgent that we are willing to pressure you into it – especially when there is not yet enough vaccine for everybody and there are people in lower-priority groups who really want that dose (and it could save their life too). So we hope you will understand our recommendation and make a well-informed choice.

There is a special case to be made for vaccinating children and healthcare workers.
In the U.S., children 0 to 4 years of age have the highest rate of hospitalization for pandemic H1N1; the 5- to 24-year-old age group has the second highest rate. In addition, both children and healthcare workers are significant transmitters of influenza. Experience so far shows that pandemic H1N1 can spread very quickly through schools, and that children who catch the disease at school can pass it along to family members. Healthcare workers come into close contact with pandemic flu patients, and also come into close contact with other patients in high-risk groups. They can all too easily catch the disease from the former and give it to the latter – often before they have any symptoms of their own, or when they have come to work feeling ill (which many healthcare workers tend to do, despite our strong advice to the contrary). In short, children and healthcare workers should be vaccinated both for their own good and also for the good of others.
Nonetheless, the pandemic disease is mostly mild so far. Some parents will prefer not to get their children vaccinated, and some healthcare workers will prefer not to get themselves vaccinated. While we believe that vaccination is medically advisable for both children and healthcare workers, we have no intention of pressuring people to change their personal health decisions in order to protect other people from a disease that is usually mild. Parents and healthcare workers who have decided against pandemic flu vaccination should know that the public health profession recommends in favor of pandemic vaccination, for the good of both the person vaccinated and the people that person has contact with. And then they should make their own decisions without any pressure from us.

All this could change.
Back in the spring, we judged it to be an urgent priority to order a lot of novel H1N1 vaccine, chiefly because it was not yet clear how virulent or mild the new virus was turning out to be. We were also concerned (and still are) that the novel (now pandemic) H1N1 virus might become more virulent at any time. We hoped then – as we hope now – that a vaccine against an early strain of pandemic H1N1 would be at least partly effective against a more lethal mutation of pandemic H1N1. Such a mutation has not happened so far, but it is still a possibility.
If the pandemic H1N1 virus does become more virulent, and if the vaccine still works against that new, more virulent strain, we will implement an emergency mass vaccination program. Such a program has already been developed in case it is needed. So far, there are no signs of increasing virulence, and there is no expert knowledge bearing on whether such a change in the virus is likely or unlikely. We are watching for it. If it happens we will push much harder for mass vaccination, and will try to persuade even those who are anxious about the vaccine to change their minds.
Other developments that would affect our advice would be: (a) If evidence emerges that the H1N1 virus is becoming more resistant to antiviral medications, making the vaccine our only effective pharmaceutical intervention; (b) If evidence emerges that a particular group of people is more vulnerable to serious H1N1 complications than has so far been evident; or (c) If evidence emerges that the vaccine has unexpected complications or is less effective than we anticipate.

-
Eventually we hope most people will be vaccinated against H1N1.
The novel H1N1 virus is here to stay. Odds are it will remain pandemic for a year or two, and will then become one of the influenza strains that circulate seasonally. If that happens, the pandemic H1N1 vaccine will become part of the seasonal flu vaccine. Eventually we want as many people as possible to have been vaccinated against this new strain of influenza. The sooner lots of people have antibodies against this disease, the safer we will all be. (Of course people who have had the pandemic flu already have these antibodies now, and therefore do not need to be vaccinated. Unfortunately, we have no reliable, cost-effective test that would enable us to screen these people out of a mass vaccination program.)
The best time to get vaccinated against pandemic H1N1 would have been last April, when the novel H1N1 virus first appeared. But we have all had to wait – involuntarily – until initial batches of pandemic H1N1 vaccine could be produced, tested, approved, and distributed. We don’t yet have enough vaccine for everyone in the country who wants it, so some people in non-prioritized groups will have to wait a few months more – once again, involuntarily. People in the developing world, where there is very little vaccine, will have to wait a lot longer than that – also involuntarily. If some people in prioritized groups also want to wait – voluntarily – to see how the virus develops and make sure nothing goes wrong with the vaccine, they should feel free to do so.

-
Don’t forget the seasonal flu vaccine.
The case for getting vaccinated against the seasonal flu is a little weaker this year than it is most years (at this point in the season), for two reasons. First, the pandemic strain may out-compete some of the seasonal flu strains – as happened in some countries in the Southern Hemisphere during their flu season this year – which means this year’s seasonal flu strains may cause less disease than usual. Second, one of the seasonal flu strains, H3N2, may be drifting from the one that’s in the 2009-2010 vaccine, which means this year’s seasonal vaccine may be less effective than usual. Despite these two possible (but not yet established) factors, getting vaccinated against the seasonal flu remains a good idea, especially for healthcare workers, people over 60, and people in other high-risk groups.
If you’re willing to do one or the other but not both, which one do we recommend? Of course we think ideally everyone would choose to get both vaccines, once they are available – and we don’t expect a shortage of the seasonal flu vaccine this year. Still, if you have decided to pick only one or the other, here’s our recommendation, with reference to your specific risk characteristics….
My wife and colleague Jody Lanard assisted on this update.
Posted: July 21, 2009
The Three-Legged Stool of Pandemic Messaging
by Peter M. Sandman
 Clients and others often ask me what I think the key messages ought to be about the ongoing H1N1 pandemic.
Clients and others often ask me what I think the key messages ought to be about the ongoing H1N1 pandemic.
To some extent, of course, the answer depends on when the question is asked and where the questioner is located.
- Is the virus currently spreading fast through your area, or has it receded for now, or hasn’t it really gotten started yet where you are?
- Is your local population still largely unaware, or newly aware and going through an alarmed adjustment reaction, or past the adjustment reaction and pretty complacent, or post-complacency and going through a second adjustment reaction?
What’s surprising is how little the specifics of when and where have mattered so far.
Obviously if the pandemic virus changes radically – if it becomes much more or much less virulent, for example, or if it becomes much more or much less transmissible – that will profoundly affect what we need to tell people.
But the only major change we have seen so far came in late April, during the first few days of the outbreak. The early data from Mexico had suggested a high case fatality rate. That proved mistaken and by early May it was clear that the novel H1N1 swine flu virus was causing mostly mild diseases and comparatively few deaths.
Since then, there have been lots of little surprises – but no big ones. The three most important things to tell people in early May are still the three most important things to tell people in late July.
And many, many people haven’t heard those three things yet. Or at least they haven’t heard them clearly yet – in sharp relief against the dozens of other things they may have heard about the pandemic. Various governments at various times have said all three, but no government has consistently built its pandemic messaging on the foundation of these three message points.

Pandemic H1N1 will almost certainly be pervasive.
If it’s typical of other flu pandemics, it will infect one-quarter to one-half of the population before it’s over. It has already infected far more people than the official numbers suggest – because only a small fraction of people with the disease are tested and then added to the tally of confirmed cases. Get ready for a lot more people in your community, your workplace, and your family to catch pandemic flu.

Pandemic H1N1 looks very mild so far.
Based on pretty good data about how many have died and rough estimates (grounded in surveillance and modeling) about how many have had the disease, the case fatality rate so far is apparently lower than the rate for the seasonal flu. But even a mild flu that infects 2–3 billion people worldwide (as this one probably will) will inevitably kill millions, many of them young and some of them previously healthy. And even a mild flu, when it’s that pervasive, can cause some disruptions due to absenteeism. That’s the most hopeful scenario, and it’s the path we are on so far: a pervasive but mild pandemic that causes widespread minor disruptions (school closings, supply chain problems, etc.) and some more serious disruptions (such as overloaded healthcare systems), and ends up killing something less than one-in-a-thousand of the billions who will get it.

We must prepare for the possibility that pandemic H1N1 could become more severe.
Flu is famously unpredictable, and some past pandemics (e.g. 1918) have had mild first waves and severe second waves. So we need to prepare – as a society and as individuals – not just for the pervasive-but-mild scenario (which is where we hope we’re headed), but also for the pervasive-and-severe scenario. Good hygiene practices like covering your cough and washing your hands will help only a little, though they’re better than nothing. There is much more to be done, from stockpiling supplies to cross-training people to cover for absent colleagues. But deciding what precautions to take against a disease that may or may not get more severe is a tough call, for individuals as well as for communities, companies, and governments. And if a severe pandemic materializes, it will be a very major threat to health no matter how much we have prepared.
I thought hard about adding a fourth leg to my pandemic messaging stool, devoted to the things people can do to reduce their chances of getting the flu, or of giving it to others if they have it already. I’m not averse to advising people to wash their hands and cover their coughs when they can (though it’s hard to do either on the bus or the assembly line). I’m not averse to advising people to stay out of crowded places when they can, and to think about wearing a mask if they have to venture into crowds. I’m certainly not averse to advising people – begging people! – to stay home when they feel sick, and to call a doctor if it starts getting bad. So I’m not averse to a fourth key message along these lines, as long as it doesn’t preempt any of the other three.
But a lot of hygiene advice is only marginally actionable and, when actionable, only marginally effective. The experts who say flu pandemics ultimately infect one-quarter to one-half of the population never go on to say it’ll be one-quarter if we all wash our hands and cover our coughs and one-half if we don’t.
In August 2009, a reader from Norway wrote to argue that this fourth leg – what people can do to protect themselves and others – deserved to be added. The more I thought about his arguments, the more I decided he was right – for a variety of reasons outlined in this exchange.
On balance, what I really want people to know right now is this: Regardless of hygiene, we’re all going to see a lot of flu in the coming months. If we’re lucky, it will stay as mild as it is so far, and most of us won’t know anyone who dies from it … even though it will still kill several million people out of the 2–3 billion it infects. If we’re not so lucky, it will get more severe, causing many more deaths and major disruptions in the supply of goods and services. Some governments are preparing for a possible severe pandemic, and companies, communities, and individuals should think about making preparations of their own.
My three paragraph-long messages may strike you as too long and complicated – especially if you’re working in a country where the media and the public are currently not very interested in pandemic information.
So I tried to shoehorn them into message maps.
Below are four message maps: a “big picture” map with all three key messages, followed by separate maps for each of the three. Unlike the paragraphs above, the message maps that follow are oriented specifically to the U.S. audience. But minor changes would make them suitable for other countries.
I didn’t struggle to make the information in the message maps below exactly the same as the information in the paragraphs above. Feel free to mix and match. And for that matter, feel free to add your own supporting facts.
What’s crucial, I think, is that until something major changes, this is the three-legged stool of pandemic messaging:
- Pandemic H1N1 will almost certainly be pervasive.
- Pandemic H1N1 looks very mild so far.
- We must prepare for the possibility that pandemic H1N1 could become more severe.
Note that Vincent Covello, the creator of the message mapping approach, is not in any way responsible for the message maps that follow, which are longer and more complicated than he would recommend. (These are my first published message maps, ever.) For one of Vincent’s several readily available articles on message mapping, see “Message Mapping.” 
What do we need to know about pandemic H1N1?
| Key Message 1 | Key Message 2 | Key Message 3 |
|---|
| Pandemic H1N1 will almost certainly be pervasive. | Pandemic H1N1 looks very mild so far. | We must prepare for the possibility that pandemic H1N1 could become more severe. |
| | |
| Supporting Fact 1–1 | Supporting Fact 2–1 | Supporting Fact 3–1 |
| Pervasiveness is one of the defining characteristics of a pandemic. In the early months that’s sometimes hard to see, but soon it will be unmistakable. | So far, for every 10,000 people in the U.S. sick with pandemic H1N1, only 2–3 have died. | Influenza is notoriously unpredictable. |
| Supporting Fact 1–2 | Supporting Fact 2–2 | Supporting Fact 3–2 |
| Pandemic H1N1 has already infected over a million Americans. It is infecting more every day, and will infect far more in the months ahead. | So far, pandemic H1N1 is much milder than the seasonal flu and much, much milder than the famous 1918 pandemic. | Some governments are preparing for the possibility of increased severity, although there is no such thing as “complete readiness” for a severe pandemic. |
| Supporting Fact 1–3 | Supporting Fact 2–3 | Supporting Fact 3–3 |
| Don’t be misled by the much smaller number of confirmed cases. That’s just the tip of the iceberg. | Even if the pandemic stays this mild – a big if – it will need to be taken seriously. | Companies, schools, civic groups, individuals, and families should also consider ways they can become more prepared. |
Pandemic H1N1 will almost certainly be pervasive.
| Key Message 1 | Key Message 2 | Key Message 3 |
|---|
| Pervasiveness is one of the defining characteristics of a pandemic. In the early months that’s sometimes hard to see, but soon it will be unmistakable. | Pandemic H1N1 has already infected over a million Americans. It is infecting more every day, and will infect far more in the months ahead. | Don’t be misled by the much smaller number of confirmed cases. That’s just the tip of the iceberg. |
| | |
| Supporting Fact 1–1 | Supporting Fact 2–1 | Supporting Fact 3–1 |
| Past flu pandemics have ultimately infected one-quarter to one-half of the world population before they ended. | Based on surveillance and modeling, the CDC estimates that over a million Americans have already had pandemic H1N1. | In the U.S. we stopped testing and counting most cases back in early June. |
| Supporting Fact 1–2 | Supporting Fact 2–2 | Supporting Fact 3–2 |
| This pandemic is also likely to infect one-quarter to one-half of the world population – and one-quarter to one-half of the U.S. population as well. | The pandemic has slowed for now in the U.S., but it is still here – and in other countries such as the U.K. and Argentina it is spreading fast right now. | Almost every case of influenza this summer is pandemic H1N1, regardless of whether it has been tested and confirmed. |
| Supporting Fact 1–3 | Supporting Fact 2–3 | Supporting Fact 3–3 |
| However, people over 50 may have partial immunity from earlier strains of H1N1, and vaccination will protect some people if we are able to produce an effective vaccine. | We don’t know when – but various U.S. locations are expected to become pandemic H1N1 hotspots at different times, in waves of 6–8 weeks over a year or two. | Even though the estimated total number of cases is an approximation, it is a much more useful number than the tally of confirmed cases. |
Pandemic H1N1 looks very mild so far.
| Key Message 1 | Key Message 2 | Key Message 3 |
|---|
| So far, for every 10,000 people in the U.S. sick with pandemic H1N1, only 2–3 have died. | So far, pandemic H1N1 is much milder than the seasonal flu and much, much milder than the famous 1918 pandemic. | Even if the pandemic stays this mild – a big if – it will need to be taken seriously. |
| | |
| Supporting Fact 1–1 | Supporting Fact 2–1 | Supporting Fact 3–1 |
| The total number of confirmed U.S. deaths from pandemic H1N1 so far is 263, out of an estimated 1,000,000+ Americans infected so far. | The seasonal flu is thought to kill roughly 36,000 Americans in a typical year. That’s one death for every 1,000 cases – about four times as severe as pandemic H1N1 so far. | Because the total number of infected people is expected to be so huge, the number of deaths will be substantial and may surprise and alarm some people, despite the very low percentage. |
| Supporting Fact 1–2 | Supporting Fact 2–2 | Supporting Fact 3–2 |
| This is the most informative number to look at: 263 U.S. deaths out of 1,000,000+ illnesses, not 263 U.S. deaths out of 40,000+ confirmed cases. The second comparison falsely implies a much more severe pandemic than we are actually experiencing so far. | On the other hand, 95% of those who die because of the seasonal flu are elderly. By contrast, a high percentage of pandemic H1N1 fatalities are young people. | Because it is likely to be so pervasive, even a mild pandemic will probably continue to cause intermittent disruptions, especially in schools and hospitals and potentially in the delivery of goods and services. Preparing for such disruptions is common sense. |
| Supporting Fact 1–3 | Supporting Fact 2–3 | Supporting Fact 3–3 |
| We are very, very lucky that this pandemic is so mild. If it stays that way, it will probably infect 2–3 billion of the 6.4 billion people worldwide, and over a hundred million in the U.S. But better than 999 in 1000 will recover. | The 1918 pandemic killed 2–3% of the people it infected – roughly a hundred times as deadly as this one so far. The other two pandemics in modern times, 1957 and 1968, were much more like the 2009 pandemic is shaping up to be so far – killing about one victim in a thousand (1957) or less (1968). | If the pandemic stays this mild, many people (especially without underlying health conditions) may be understandably uncertain about whether to get the new pandemic H1N1 vaccine, if and when it becomes available.
|
We must prepare for the possibility that pandemic H1N1 could become more severe.
| Key Message 1 | Key Message 2 | Key Message 3 |
|---|
| Influenza is notoriously unpredictable. | Some governments are preparing for the possibility of increased severity, although there is no such thing as “complete readiness” for a severe pandemic. | Companies, schools, civic groups, individuals, and families should also consider ways they can become more prepared. |
| | |
| Supporting Fact 1–1 | Supporting Fact 2–1 | Supporting Fact 3–1 |
| Influenza mutates easily, and some mutations could make it cause more severe illnesses. | We are watching for indications of increased severity – looking for changes in the virus itself, looking for changes in the symptoms of victims around the world, etc. | Everyone should have a plan – not just for a pervasive-but-mild pandemic, but also for the possibility of a pandemic that is both pervasive and severe. |
| Supporting Fact 1–2 | Supporting Fact 2–2 | Supporting Fact 3–2 |
| That’s what happened in 1918, the worst flu pandemic in modern history. | Pharmaceutical companies are working to develop a vaccine. If the pandemic virus does become more severe, we hope that the vaccine will still work against it, but we cannot know how well or even whether it will work. | Planning is partly about understanding and feeling – getting used to the idea that a severe pandemic is still possible and will be frightening if it happens. |
| Supporting Fact 1–3 | Supporting Fact 2–3 | Supporting Fact 3–3 |
| So far there is no indication whatever that this is happening – none. But it has happened before, and it could happen again. | This summer, the U.S. government has budgeted over a billion dollars for flu vaccine purchase and planning. It has budgeted additional money to help state and local health departments and local hospitals try to increase their ability to respond to a large surge in patients. | For individuals and families, planning also includes stockpiling food, medicines, and other essentials in case supplies run short or it’s unwise to go out for a few weeks. |
Posted: July 7, 2009
Why Pandemic Complacency Isn’t Okay
by Peter M. Sandman
 By now it’s so obvious that Americans aren’t very worried about swine flu that even the “people should stop panicking” commentators have moved on to other topics.
By now it’s so obvious that Americans aren’t very worried about swine flu that even the “people should stop panicking” commentators have moved on to other topics.
Gallup hasn’t polled on swine flu since June 14, right after the World Health Organization officially declared H1N1 a pandemic. Respondents were asked whether they worried about getting swine flu “yesterday.” The pandemic declaration notwithstanding, only 8 percent said they did – down from 25 percent in late April.
Eight percent of the U.S. population is still a lot of people. It’s apparently enough people to justify a thriving market in spam purporting to sell Tamiflu. Still, U.S. public opinion today is far closer to flu pandemic complacency than to flu pandemic panic … or flu pandemic fear, or flu pandemic anxiety, or even flu pandemic concern.
Note to readers in other countries
This update focuses on U.S. flu pandemic complacency, and why I think officials should do more to combat it.
Much of the world is still going through its pandemic adjustment reaction. Far from being complacent, people in many countries are overreacting – imagining that the disease is deadlier than it is and demanding that the government take futile steps to “stop” it: quarantine travelers, close schools, sanitize handrails and even streets.
If you live in such a country, this column isn’t for you. Read the column I recently wrote with Jody Lanard on “Containment as Signal” instead.
Will something happen to get people worried again? Nobody knows. Flu pandemics are notoriously unpredictable, and this pandemic is still in its early months.
It’s nearly a sure thing that swine flu will be much more pervasive in the U.S. next winter than it was this spring. The rule of thumb for flu pandemics is that they end up infecting one-third to one-half the population – not all at once, but over a couple of years. The typical pattern is intense local epidemics that last 6–8 weeks and then move on, often returning two or three times before the pandemic is over. Most people over 50 seem to have partial immunity to swine flu from early exposures to similar viruses. And before winter arrives, U.S. officials hope to have a vaccine they can offer at least to people in high-risk groups. So we may do better than one-third to one-half. Still, a lot of people are going to get sick.
The big unknowns: How sick will they get, how many will die, and how much impact will pandemic absenteeism have on supply chains for food, medicines, and other essentials.
Three pandemic scenarios
To anchor our expectations, consider three pandemic scenarios:

No big deal.
Pandemic H1N1 could turn out so mild that people barely notice they’re in the middle of a pandemic. This is the scenario that comes to mind when we consider that the CDC guesstimates that over a million Americans have already had swine flu and only 170 of them have died – a case fatality rate way below the rate for seasonal flu. It’s what comes to mind when we consider that the CDC thinks 7 percent of the New York City metropolitan area may have had the disease in a concentrated two-month period with relatively minor impacts on absenteeism (except in schools) and the flow of goods and services. We could dodge the bullet.

Serious but manageable.
Pandemic H1N1 could turn out comparable to seasonal flu in terms of how sick it makes people and what percentage of them die. Seasonal flu is the comparison U.S. health officials use most often – but it’s not clear if they’re trying to “err on the alarming side”  or if they actually think the second scenario is likelier than the first.
or if they actually think the second scenario is likelier than the first.
The second scenario is more serious than most Americans imagine, especially if the pandemic virus coexists with seasonal flu viruses instead of crowding them out. If swine flu infects one-third to one-half of the population and kills the same percentage as the seasonal flu does, we’re talking about roughly 100,000 U.S. deaths, most of them young people who considered themselves pretty healthy till the swine flu hit. Hospitals will be overloaded. In flu hotspots, debate will rage over whether to close schools, and whether to cancel concerts, football games, and other events that bring people – especially young people – close together. Absenteeism may interrupt some services, some manufacturing, and some shipping, possibly leading to shortages of essential supplies like food and medicine.
Many Americans will be surprised, probably worried, and possibly upset about these effects, especially if they feel they weren’t properly warned and aren’t properly prepared.

Nightmare.
Pandemic H1N1 could mutate into a more severe disease, as happened during the 1918 pandemic (which started mild). A change in the virus might also make the first pandemic vaccine useless, and make people over 50 and people who already had swine flu this spring vulnerable again.
1918 was the worst flu pandemic in recent history; two to three percent of victims died, compared to one-in-a-thousand for seasonal flu. Anything that deadly would be even more disruptive today, given our globally integrated economy and our just-in-time supply chains. A pandemic less severe than 1918’s but significantly more severe than an average flu year would be nightmare enough, and that’s the scenario pandemic preparedness discussions usually emphasize.
A replication of 1918 isn’t the worst case scenario. Pandemic H1N1 could mix-and-match genetic material with the H5N1 (bird flu) virus – which has infected very few people but killed an astounding 61 percent of them. A new virus as transmissible as H1N1 and as deadly as H5N1 is the ultimate pandemic nightmare, almost too awful to prepare for.
Public health officials know that all three scenarios (and intermediate ones, of course) are possible. They’re worried about the third, planning for the second, and hoping for the first.
Which scenario does the U.S. public expect? Certainly not Scenario 3, the nightmare. I suspect most Americans would say they think this new pandemic flu is a lot like the seasonal flu. That’s Scenario 2. But most Americans greatly underestimate the severity and impact of the seasonal flu, and very few have thought through what it means when a novel flu as severe as the seasonal flu strikes a population that hasn’t had years of prior exposure and prior vaccination. So in actuality, most Americans – those who have thought about it at all – probably expect something a lot like Scenario 1.
That’s the problem.
It’s not the problem I anticipated. I always figured risk communication during an influenza pandemic would be crisis communication: high-hazard, high-outrage. Well, we’re in the middle of a bona fide, WHO-certified influenza pandemic, my first influenza pandemic as a risk communication professional – and right now in the U.S. it is turning out to be a high-hazard, low-outrage event.
The riskcomm paradigm isn’t crisis communication after all; it’s precaution advocacy. The riskcomm task isn’t helping people cope wisely with their distress at the pandemic they’re enduring. The task is getting people to take the pandemic seriously enough – convincing them to prepare for the near-certainty that it will be pervasive and the distinct possibility that it may become severe. It’s as if we were still back in the World Health Organization’s Phase 3, rather than nearly a month into Phase 6.
U.S. public health officials do not see pandemic precaution advocacy as an important priority (other than advising people to wash their hands, cover their coughs, and stay home if they’re sick). It’s not that they’re hiding their judgment that the pandemic will be pervasive and may become severe. CDC spokespeople have been scrupulously forthright. But they’re not really stressing these predictions either. Only one country has repeatedly and vividly told its people to expect pervasiveness, and periodically (though less vividly) warned them about possible severity: New Zealand.
Squandering teachable moments
In our June 29 column on “Containment as Signal” Jody Lanard and I criticized officials – not for the first time or the last – for doing too little to battle public complacency. We received this response from the CDC’s Dan Rutz, a public health communication professional who is one of the most dedicated and thoughtful readers of this website:
Come on, guys. It’s OUR job in public health not to be complacent, and to provide that “just-in-time” push when people do need to pay greater attention. You just can’t keep folks in high alert all the time. Life’s too short.
He has a point. It is much more efficient to wait for “teachable moments” of high public concern than to try to arouse concern in people whose attention is elsewhere. Talking about teachable moments in my 2007 column, “‘Watch Out!’ – How to Warn Apathetic People,” I wrote:
Although the audience for precaution advocacy is typically apathetic, there are moments of interest, sometimes even pretty intense interest. These are the teachable moments, when people are temporarily paying attention…. Anticipate these teachable moments (or provoke them), and make the most of them.
Between teachable moments, do what you can to keep the issue alive, and work with the minority that is already interested (perhaps as a result of the previous teachable moment). But don’t invest too much effort striking while the iron is cold. Your time is probably better spent preparing for the next teachable moment.
Too often we get this exactly backwards. We’re out there struggling to arouse concern in an apathetic audience. And then when something happens and the audience is concerned at last, we succumb to our fear-of-fear and our panic that people may panic and start putting out reassuring messages. When a teachable moment comes along, capitalize on it!
The paradigmatic teachable moment is when people become newly aware of a risk and temporarily overreact. Jody and I have labeled this temporary overreaction an “adjustment reaction.”
Unfortunately, authorities are often tempted to criticize, ridicule, and try to squelch the public’s adjustment reactions, instead of using them as teachable moments.
Back when H5N1 (bird flu) was the main focus of experts’ pandemic concern, a country’s first widespread outbreak in birds predictably provoked an adjustment reaction. Every such outbreak gave authorities a chance to prioritize two messages: warning people that someday the virus might start causing similar outbreaks in humans, and reassuring people that poultry is safe to eat. In country after country, the second message totally drowned out the first.
When H1N1 (swine flu) emerged in April 2009, Acting U.S. CDC Director Richard Besser was refreshingly supportive of the public’s concern. “We hear from the public and from others about their concern,” he said, “and we are worried, as well.”
But while U.S. health officials didn’t try to squelch people’s adjustment reaction, they stopped short of capitalizing on that reaction to urge preparedness – for example, to ask people to stockpile food, medicine, and other supplies. This led me to entitle my first swine flu column: “The Swine Flu Crisis: The Government Is Preparing for the Worst While Hoping for the Best – It Needs to Tell the Public to Do the Same Thing!”
Since then, the U.S. has frittered away one swine flu teachable moment after another. Here are four examples:
- On June 11, the World Health Organization declared Phase 6. This formal pandemic declaration was an obvious teachable moment – so potentially alarming that many national governments had begged WHO to postpone it. The CDC’s statement about the declaration stressed that it had no immediate implications for the U.S., since we had accepted the reality of sustained community transmission some weeks earlier. That’s accurate. But is it really what you’d want to emphasize if you were looking for opportunities to warn people that things may get worse in the months ahead?
- On June 24, health officials in Rochester, New York announced that the city and county hospitals were “experiencing a tremendous strain” because of high volumes of pandemic flu cases. Rochester was the second metropolitan hospital system in North America to concede serious problems coping with pandemic cases; the first had been Winnipeg, Canada, two weeks earlier. It was a big local story. But national health authorities didn’t choose to dramatize it as a possible or probable harbinger of things to come.
- On June 26, the CDC announced that according to modeling estimates over a million Americans had already had swine flu. The story got pretty good coverage, considering the low level of journalistic interest in the flu pandemic these days. But imagine the coverage if a CDC official had taken reporters through the modeling predictions for the future, with graphics to match. Imagine if the CDC had released for television one of those computer simulations where the map of the United States turns red as the cases mount up. Imagine if the CDC had tried to make really vivid the likely pathway from 1 million cases to 100–150 million cases.
- As I write this, Argentina looks like the southern hemisphere’s pandemic Ground Zero. Parts of the country have declared a state of emergency, and Argentina has reported a larger death toll than anywhere else outside North America. The Buenos Aires health minister said that “hospitals are over-crowded, but not collapsed,” and the city’s mayor extended the 11-day school winter vacation to almost a month. U.S. officials keep saying they are watching developments in the southern hemisphere closely. They haven’t yet chosen to describe those developments vividly to the U.S. public.
It is sound risk communication strategy to capitalize on teachable moments rather than trying to flog the story when nothing’s happening and nobody’s listening. But how can officials justify downplaying developments rather than pouncing on them? There are plenty of swine flu pandemic teachable moments. We’re just not using them well.
Why talk now
Now isn’t the best time to talk to the public about preparedness for a potentially severe pandemic. The best time would have been several years ago. But better now than later, or never.
Back in Phase 3, far too many officials kept over-reassuring people during teachable moments, instead of guiding them in the direction of individual and group preparedness. It was frustrating. But I never imagined it would still be the case in Phases 4 and 5, and even now in Phase 6, after the pandemic has started. If the U.S. government isn’t going all out to encourage public preparedness in Phase 6, when does it plan to do so? There is no Phase 7.
Why is it urgent to get people preparing now? There are six main reasons.

-
Cognitive preparedness: People need to think through in advance what they will do if the pandemic causes widespread disruption.
Here are some excerpts from the “Individuals & Families Planning” section of www.pandemicflu.gov – the U.S. government website that was launched when there wasn’t any pandemic yet:
As you plan, it is important to think about the challenges that you might face, particularly if a pandemic is severe. It may take time to find the answers to these challenges….
- Plan for the possibility that usual services may be disrupted. These could include services provided by hospitals and other health care facilities, banks, stores, restaurants, government offices, and post offices.
- Prepare backup plans in case public gatherings, such as volunteer meetings and worship services, are canceled.
- Consider how to care for people with special needs in case the services they rely on are not available.
- Find out if you can work from home.
- Ask your employer about how business will continue during a pandemic….
- Plan for the possible reduction or loss of income if you are unable to work or your place of employment is closed.
- Check with your employer or union about leave policies….
- Help schools plan for pandemic influenza…. Plan home learning activities and exercises. Have materials, such as books, on hand….
- Think about how you can rely less on public transportation during a pandemic. For example, store food and other essential supplies so you can make fewer trips to the store….
Stock a supply of water and food. During a pandemic you may not be able to get to a store. Even if you can get to a store, it may be out of supplies. Public waterworks services may also be interrupted….
And from a different section of the same government website:
Plan now before a flu pandemic hits
You and your community need to start planning now while no flu pandemic exists. You need to be ready when the flu pandemic first arrives in your area….
Making plans now will help you to be ready for the next flu pandemic, which could last up to several months.
This website is still up there, unchanged. It is still referenced occasionally by the CDC and other government agencies. It hasn’t been disavowed. But now that we actually have a pandemic, a mild one so far, its actual recommendations are no longer mentioned much. Go figure.

Logistical preparedness: People need to take some advance actions to prepare themselves for possible pandemic disruptions.
In the early days of the emerging pandemic, when the outbreak in Mexico looked really severe, the CDC hesitated to recommend individual stockpiling of food, water, medications, batteries, facemasks, and other supplies. Officials from several agencies told me that such recommendations were considered, but rejected on the grounds that a sudden nationwide run on the stores would empty the shelves and could even precipitate a panic.
The pandemic has turned out fairly mild so far, and in many parts of the country it has receded for now. People are nowhere near panic. Most are complacent. And still the authorities are unwilling to recommend stockpiling.
Nobody knows if pandemic conditions will get bad enough that people will need their stockpiles. What we do know is this: After it’s clear that we might soon need our stockpiles, it will be too late for most people to stockpile. There are no non-medical supply chain problems right now, in early July 2009. Anyone who buys extra supplies now can be confident that the stores will restock promptly. The more people who buy extra supplies now, the fewer will need to do so at the last minute, if that time ever comes, when the risk of empty shelves (and conceivably even the risk of panic) will be real.
Government hesitates to urge people to stockpile when an emergency looks imminent because it’s too late; store shelves will empty and people may panic. That was the situation in late April when the swine flu news from Mexico looked bad, and that may be the situation later this year if pandemic conditions worsen. Then government should urge people to stockpile when there is no imminent emergency … like now.
Sometimes officials tell me they can’t recommend household stockpiling because not everyone can afford it. The rebuttal: That is a good reason to recommend community, faith-based, and charitable organization stockpiling as well. If poor Americans will need help to get through a pandemic, let’s at least try to make sure that affluent Americans won’t be competing for that help.
Government aside, companies have a deep continuity stake in their employees’ home pandemic preparedness. The value of masks and hand sanitizers in the workplace goes way down if employees don’t have them or don’t use them at home. An employee who gets the flu on the bus will be lost to the company as surely as one who gets the flu at work. Healthy employees are likelier to come to work in a pandemic if they believe their families are adequately prepared and adequately protected. Despite all this, companies – even those that are taking workplace pandemic preparedness seriously – are doing far too little to help their employees get ready at home.

-
Emotional preparedness: People need to feel their way into what a bad pandemic might be like.
The core of the adjustment reaction concept is that people need time to become emotionally accustomed to novel and scary risks. We pass through identifiable stages:
- At first we’re insufficiently concerned – initially unaware; then aware but uninterested; then interested but uninvolved.
- Then we’re excessively concerned, or perhaps prematurely concerned – acutely aware, anxious, hypervigilant, determined to “do something!”
- So we do something….
- Then we settle into the “new normal” – more concerned (and more prepared) than previously, but no longer so preoccupied with preparedness.
It’s an iterative process; each new alarm provokes a new adjustment reaction, followed by a new “new normal” at a higher level of preparedness. The third bullet point (“So we do something….”) is the stage where we decide what actions to take in response to our new awareness and alarm. If leaders are respectful of our adjustment reaction, they will have a better chance of influencing those decisions.
Most people cope as best they can, of course, even if a crisis catches them emotionally unprepared. But we cope better if we have had time to get used to what might be coming.
This is what worries me most about the reluctance of health authorities to scare people.
Scaring people isn’t the goal of pandemic warnings. A temporary fear reaction is a likely side-effect, not the goal, of providing vivid information about the potential course of the pandemic. The goal is to motivate precautionary planning and precautionary action before it is too late, and before it is needed.
If the pandemic becomes more severe, or if a mild-but-pervasive pandemic starts seriously disrupting our lives, people will be scared. The crisis itself will scare them. Too many officials think it’s a disservice to scare them in advance. But people who better understand a future hazard – including imagining how frightening it may be, and vicariously rehearsing what it may feel like – will be less frightened and more prepared (cognitively, logistically, and emotionally) when the time comes.

-
Trust: People need to remember that they were properly warned.
If and when the pandemic gets a lot worse, health officials won’t be terribly surprised. And they will say so. “This is not unexpected,” they’ll say. “It was always one of the possibilities we were preparing for.” They’ll even be able to point to moments when they mentioned what might happen.
Nonetheless, people who didn’t pick up on those moments will feel blindsided – even misled, maybe even betrayed. As a result, they will be less inclined to follow the recommendations of health officials.
A certain amount of mistrust is inevitable in a crisis. No matter how often and emphatically officials warn the public about an emerging threat, some people will shrug off the warnings – and then blame the officials for not warning them often and emphatically enough. But when officials really haven’t done much to warn the public vividly, the resulting mistrust will be greater. A government that isn’t remembered as having warned about the possibility of bad times cannot lead its people as effectively when bad times come.
What’s really sad is that the U.S. government has been extraordinarily candid about this pandemic. Unlike some governments around the world, it hasn’t suppressed information about cases. It acknowledged the inevitability of sustained community transmission from Day One. It reiterates periodically that influenza is unpredictable and that an increase in virulence is among the possibilities.
Some U.S. health officials may actually believe they are shouting their concerns from the rooftops. They always have the nightmare scenario in the backs of their minds; it keeps them working and may sometimes keep them from sleeping. So they may feel like they are warning loudly when they’re only whispering.
Others know they’re only whispering. But if bad times come and people feel blindsided, they too may experience a sense of grievance. They may even convince themselves, looking backward, that they did everything they could to alert the American public to the full range of pandemic risks, and the public simply wasn’t listening.
They’ll be wrong. The government is not doing for the flu pandemic what it has tried to do for smoking, for HIV, for hurricanes, even (since the last change in administration) for climate change. It is telling the truth about swine flu, but it is not making the truth vivid, and it is not making a serious effort to get people to prepare.
It’s not easy to get people to prepare – especially for a risk that has acquired the reputation of a paper tiger. SARS never went pandemic. Bird flu hasn’t gone pandemic yet. Swine flu was declared pandemic, and after the first few days it was barely noticeable in most places. People have learned to greet pandemic warnings with some skepticism.
I would respect an argument from government officials that they don’t dare try to alert the American public, for fear of just getting laughed at and further eroding the credibility of government warnings. I don’t agree, but it’s a respectable argument. And I respect the argument that under the circumstances it is wiser to let people live their lives and wait to urge preparedness until the risk is more visible and people are likelier to be responsive. I don’t agree with that either – I’m writing this update to rebut it – but I respect it.
Let the government give whatever reasons it wishes for its decision not to try to warn people vividly and persuade them to prepare. We can assess those reasons on the merits. But don’t let the government claim it is trying its best to warn people vividly and persuade them to prepare. It isn’t. And if the pandemic situation deteriorates, diminished trust will be part of the price it pays.

Interconnectedness: People need to know about the pandemic plans of their own organizations.
U.S. health authorities are in fact planning for the near-certainty that the swine flu pandemic will become more pervasive, and the possibility that it could become more severe. The plans aren’t secret. (At least most of them aren’t.) You can find them online – plans for everything from how to allocate vaccine  and other scarce medical supplies (from Tamiflu to ventilators) to how to store bodies if the mortuaries run out of room and it’s not safe to have funerals.
and other scarce medical supplies (from Tamiflu to ventilators) to how to store bodies if the mortuaries run out of room and it’s not safe to have funerals.
If these plans need to be implemented, public acceptance will depend partly on how many people were aware of them in advance.
But people have a still more urgent need to know about the pandemic plans of institutions closer to home – their local health department; their children’s schools; every institution they intersect, from soup kitchen to church to health club. Knowing that these institutions actually have pandemic plans may help motivate people to do their own household planning. Knowing what the plans provide may enable people to make their household planning more compatible.
People especially need to know about their employers’ pandemic plans. If a company expects employees to implement its pandemic plan when the time comes, then employees need to know about it beforehand. Employees are also much likelier to come to work in a pandemic if they know what sorts of preparations have been made in their workplace.
If the pandemic gets worse, pandemic information (and misinformation) will be everywhere. Competition for the public’s attention will be fierce. Any institution that hopes to be seen as a relevant and reliable source of pandemic information then needs to be building its pandemic credibility now.

-
Collaboration: People have a right to influence the planning of government and other institutions – and the plans will be better if they participate.
When people become aware of governmental and institutional pandemic planning, they discover things they don’t like.
That may be one reason why governments can be reluctant to sound the alarm before it’s absolutely necessary – which sometimes means before it’s too late. An aroused public doesn’t just prepare cognitively, logistically, and emotionally. An aroused public interferes.
Like the rest of us, public health officials are understandably leery of interference. They wish the public would focus on something else and let them plan in peace.
But plans made without much public involvement are intrinsically illegitimate. People have a right to influence how governments and other institutions plan to cope with the pandemic.
All through May and June, local health and education officials made decisions to close or not close schools in response to local swine flu outbreaks. Parents often responded angrily to either decision, leaving officials feeling damned if they do, damned if they don’t. Yet very few local officials saw fit to share the dilemma and seek parents’ counsel on whether to close schools. And even fewer reached out before the decision was urgent, asking parents to help them develop guidelines for when schools should be closed.
Decisions made with public input aren’t just more legitimate. They are better decisions.
Read the New York Academy of Medicine report, “Redefining Readiness: Terror Planning Through the Eyes of the Public,”  by Roz D. Lasker, M.D. Her 2004 study convincingly demonstrates that most government terrorism-response plans are close to useless because they were developed without significant citizen involvement. Lasker asked people how they would react in specified terrorism scenarios. They told her they wouldn’t react the way planners thought they would. And then they told her how the plans had to change.
by Roz D. Lasker, M.D. Her 2004 study convincingly demonstrates that most government terrorism-response plans are close to useless because they were developed without significant citizen involvement. Lasker asked people how they would react in specified terrorism scenarios. They told her they wouldn’t react the way planners thought they would. And then they told her how the plans had to change.
Many government pandemic plans have the same potentially fatal defect: insufficient public involvement.
The big picture
Very few people in the United States are seriously worried about this pandemic. Maybe they were worried at first, and now they feel a bit foolish and very skeptical. Maybe they were never worried, and now they feel vindicated. Many talk about “the swine flu scare” in the past tense. Even if they know it hasn’t gone, even if they know it’s almost sure to get more pervasive in a few months, even if they know it could get more virulent at any time, even if they know that “mild” doesn’t mean trivial – even if they know all that, they still somehow feel that we dodged the bullet and it wasn’t much of a bullet to start with.
That’s why it’s so important for health officials to voice pandemic warnings and urge pandemic preparedness. And that’s why it’s so hard for health officials to voice pandemic warnings and urge pandemic preparedness.
The U.S. public has little appreciation of the potential dangers posed by this pandemic. As a result, experts (or officials) risk being dismissed as kooks simply for describing what’s ahead if the pandemic turns out like most flu pandemics in its transmissibility and like seasonal flu in its virulence. That’s my Scenario 2. It’s not the worst case by a long shot; it’s just an extrapolation of what most officials are saying already. But they’re saying it vaguely. Say it explicitly enough and graphically enough to be understood, and you’re likely to be labeled an irresponsible alarmist.
It’s not considered “alarmist” to tell people that flu pandemics typically infect one-third to one-half of the population. It’s not “alarmist” to tell people that on average the seasonal flu kills about one person for every thousand infected. But apparently it is “alarmist” to do the math out loud: to calculate that if this pandemic is as contagious as other flu pandemics and as deadly as the seasonal flu, that will mean about 100,000 dead Americans, many of them young and previously healthy.
To most people (and most journalists) in the United States, that sounds like fear-mongering.
U.S. health officials know it’s a reasonable prediction. The pandemic may turn out much milder than the seasonal flu, or much more severe than the seasonal flu. But officials routinely say it is “like” the seasonal flu – and then they don’t crunch the numbers with any flair.
On July 2, a U.K. official made headlines when he did crunch the pervasiveness numbers with some flair. “Cases are doubling every week and on this trend we could see over 100,000 cases per day by the end of August,” Health Minister Andy Burnham told the House of Commons. He didn’t point out that at the one-in-a-thousand seasonal flu fatality rate, that would be a hundred pandemic deaths a day in the U.K.
At media briefing after media briefing, U.S. health officials keep explaining that the first influenza pandemic since 1968 is serious business – but they do so in a reassuring tone that belies their words, and without doing the math out loud. And reporters, who are routinely accused of “sensationalizing,” are not doing their own math with the numbers and percentages they have been given.
It’s not that U.S. health officials are trying and failing to sound the alarm. Several have told me they don’t want to sound the alarm. One of their paramount goals is to avoid saying things about the pandemic that could alarm the public, or could even be seen as trying to alarm the public. So as swine flu evolved into the pandemic of 2009, there was no strong messaging about public preparedness in case the pandemic takes a turn for the worse.
This isn’t an accident. It’s a decision. I don’t know if the decision is grounded in officials’ judgment that people might get too frightened to bear it … or in their judgment that people wouldn’t get frightened at all but would just ridicule them for alarmism … or in their judgment that the pandemic might turn out so mild it’s virtually a nonevent and then any warnings would come back to haunt them … or in their judgment that there will be better teachable moments later and there’s no rush so let’s wait till they come along and then start sounding the alarm….
But it is a decision. I think it’s the wrong decision.
My wife and colleague Jody Lanard contributed to this update.
Posted: June 17, 2009
Would you like another wakeup call?
by Peter M. Sandman
 In many hotels when you arrange a wakeup call for the following morning, they ask you if you’d like another wakeup call a bit later, in case you sleep through the first one.
In many hotels when you arrange a wakeup call for the following morning, they ask you if you’d like another wakeup call a bit later, in case you sleep through the first one.
Ideally, the World Health Organization June 11 official declaration that swine flu H1N1 has now reached pandemic proportions was another wakeup call. For those who were already awake to pandemic realities and possibilities, it was basically a nonevent – a welcome if belated confirmation of what we knew. But for those who might have fallen back asleep after the previous wakeup calls – the initial North American discovery of a novel swine flu virus capable of killing humans, and the quick spread of that virus throughout much of the world – I hoped the June 11 wakeup call might help.
Michael Osterholm, director of the University of Minnesota’s Center for Infectious Disease Research and Policy, writes a fortnightly “Briefing” for business continuity managers. His post-declaration “Briefing” suggests that “now you’ve got the weight of the WHO in your camp. Take advantage of the renewed interest and media attention. Now might be prime time to seek extra funding for preparedness efforts and supplies.”
Three key messages
How might you “take advantage of the renewed interest and media attention” if you’re not a business continuity manager – if you’re trying to communicate about swine flu to the general public?
Assume that the WHO pandemic declaration was genuinely a teachable moment (a debatable assumption, especially in the U.S.). What should we have used it to teach the public?
Here are the three key messages, in my judgment:

Try to protect yourself. Flu is serious.
Even a mild flu is nothing to sneeze at. Especially if you have an underlying health condition with respiratory implications (as many millions do) and you live in a place where swine flu is circulating widely, take appropriate precautions to protect yourself. When you can, avoid crowds and people who are coughing or sneezing. If you can’t, consider wearing a facemask or respirator. When you get a chance, wash your hands, and in the meantime try not to touch your eyes, nose, and mouth. (There is a different list of precautions for those who already have flu-like symptoms and want to protect others.)
Don’t be misled by the fact that fewer than 200 people have died from swine flu so far. It’s early days yet. The virus has probably infected fewer than half a million of the world’s 6.7 billion people so far. If we extrapolate into the future, we can project that eventually H1N1 will infect two to three billion and will kill at least a million of them – mostly young – on top of the estimated 500,000 annual deaths worldwide from the seasonal flu, mostly among the elderly. That’s if it stays mild.

Picture how the virus may change.
The big public health risk isn’t the relatively mild flu that’s circulating now and that will presumably keep circulating as long as there are plenty of new victims without immunity. Most swine flu victims recover without antivirals or medical attention. The big risk is what this currently mild flu might (or might not) turn into.
Swine flu could come roaring back in a much more virulent second wave, as a different H1N1 did in 1918 (and that horrific 1918 second wave hit the U.S. not in late fall but in August!). Worse yet, swine flu could reassort with bird flu to produce many virologists’ nightmare scenario: a pandemic virus as transmissible as the former (one-third to one-half of us are expected to get it eventually, unless we’re vaccinated) and as deadly as the latter (three-fifths of those who have gotten it so far died). No one can estimate the probability that this mild novel H1N1 pandemic will mutate or reassort into a severe pandemic. But that’s what governments are worrying about and trying to prepare for (while not urging us to do the same).

Get ready for a much worse pandemic.
Preparing for the nightmare scenario is next-to-impossible, but we should all be preparing for the severe but not-really-worst case: an increase in virulence. That means stockpiling food, water, medications, batteries, and other supplies at home – enough for two weeks to two months or more, depending on how pessimistic you are and how much spare cash and spare space you have. And it means pushing the organizations you’re connected to – your company, your neighborhood, your school board, etc. – to imagine a world with overflowing hospitals, devastated supply chains, and empty stores, and then take steps now to be ready to ameliorate the disaster we may eventually face.
Messaging in the U.S.
So did WHO’s June 11 declaration turn out to be a good teachable moment? In a word, no. At least in the U.S., I haven’t seen much evidence of “renewed interest and media attention.”
The U.S. has had widespread community transmission of novel H1N1 for weeks now. We’re no longer trying to keep track of confirmed cases, only deaths. We’re accustomed to the fact that swine flu is here, that it’s usually mild, and that it seems to be receding for the summer in most parts of the country. We’ve been through our swine flu adjustment reaction already. There may be more adjustment reactions to come, especially if the nature of the pandemic changes, but this one is pretty much over.
The three messages above are the main things I would want to say to anyone who’s ready to listen (and to everyone else too, if I could get their attention). If WHO’s Phase 6 declaration has made someone in your life newly ready to listen, seize the teachable moment. Most of the people in my life were either already concerned or already complacent (despite my best efforts), and don’t seem to be noticeably more concerned or more complacent after the June 11 declaration.
But put that aside. Insofar as the Phase 6 declaration was a teachable moment for U.S. audiences, how was it used? I haven’t done a formal content analysis, but my wife and colleague Jody Lanard and I reviewed numerous news articles and health department news releases from the days immediately following the WHO pandemic declaration. Here are our conclusions:

Try to protect yourself. Flu is serious.
The U.S. gets a C+ on Message 1.
Most releases and stories included a list of things people can do about swine flu. The lists tended to overemphasize things you can do to protect others (like staying home if you’re sick and covering your cough) and deemphasize things you can do to protect yourself … except hand-washing, which was endlessly stressed. Masks were neglected as usual. And there was a tendency to call all these precautions “simple” – as though it were an easy thing to spend a few months avoiding crowds and sick people.
Still, the basics were there. And lots of stories seized the opportunity to sell vaccination as something Americans can do later this year, when the seasonal vaccine and perhaps a new swine flu vaccine become available.
What was most stunningly absent was a projection into the future – an explanation of why a disease that has killed only a few dozen Americans so far is nonetheless worth taking seriously. Surveys show that very few people in the U.S. expect to get swine flu. The pandemic declaration was an opportunity to stress that, without vaccination, one-third to one-half of us will get it eventually – an opportunity that few health authorities or reporters seized.

Picture how the virus may change.
The U.S. gets a D+ on Message 2 (though a few of the better states rate up to a B-). Everyone did fine on the easy part of the message; just about all U.S. information sources pointed out that the current pandemic is mild, and the Phase 6 declaration is all about increased spread, not increased severity. As for the hard part of Message 2 – that swine flu could get much more severe – some releases and stories said so explicitly, but very, very few said so dramatically.
Many state health department releases did point out that the government is monitoring the virus for any possible changes … which suggests (if you’re reading carefully and are already knowledgeable) that one possibility is a change for the worse. In fairness, this possibility has been a frequent theme of health department statements and media coverage over the past six weeks. But the stories accompanying the Phase 6 declaration put a lot more stress on current mildness than on possible future severity.
The nightmare scenario – reassortment with bird flu – remained virtually invisible (except on pandemic preparedness blogs), as it has been all along.

Get ready for a much worse pandemic.
The U.S. gets an F on Message 3. It is almost impossible to find a U.S. health department release or mainstream media news story that seriously addressed nongovernmental preparedness for a severe pandemic – for example, one that urged individual stockpiling of food, medication, and other supplies.
The U.S. government website devoted to nongovernmental pandemic preparedness advice is www.pandemicflu.gov. Once much-touted, it has pretty much disappeared since the arrival of swine flu. (The June 11 joint statement by the Homeland Security Secretary and the Health and Human Services Secretary did refer readers to the site.) That site includes the now never-officially-mentioned recommendations about individual stockpiling.
The Phase 6 declaration wasn’t much of a teachable moment for U.S. audiences. All through the period when WHO was channeling Hamlet, angsting publicly about whether or not to call novel H1N1 a pandemic, U.S. officials were declaiming that it doesn’t really matter to us, we’re in pandemic conditions (that is, epidemic conditions) already and we know it.
But to the extent that the pandemic declaration was a teachable moment for U.S. audiences, it didn’t get well-used.
Some detail on Message 2
Considering how worried many countries’ governments had been that WHO’s pandemic declaration might terrify their publics, the declaration itself was courageously candid about the seriousness of the threat. Director-General Margaret Chan described the virus as currently “moderate” rather than “mild,” and discussed some of the alarming “what ifs” about the future of the virus. She explicitly mentioned the possibility of a more virulent strain of H1N1, and even referenced the simultaneous threat  of H5N1 bird flu, although the reassortment nightmare scenario wasn’t discussed.
of H5N1 bird flu, although the reassortment nightmare scenario wasn’t discussed.
So on June 11 and 12, Jody surveilled eight state government official statements issued in response to WHO’s pandemic declaration, to see how they were using the teachable moment.
All eight states mentioned that the virus currently causes mostly mild disease, and that the pandemic declaration does not imply a change in severity. Only three of the eight added that there is concern about whether the virus will become more virulent in the future. Four mentioned ongoing “monitoring” of the virus, with no expression of concern about future virulence. And one, Hawaii  , simply said it’s mild:
, simply said it’s mild:
The situation in Hawai’i at this time remains the same with all cases recovering at home with no complications.
This failure to warn results from short-term thinking and an excessive desire to reassure (as if the public weren’t calm enough already). It is a set-up for more excessive alarm later, if the situation worsens and people haven’t had a chance to brace themselves. It is also a set-up for unnecessary mistrust and outrage, if the situation worsens and people start asking hard questions about why they weren’t more aggressively warned.
Here are the three comparatively good examples of state warnings about possible future increases in virulence.
From New York:
[We] continue to monitor the virus closely to quickly identify changes in trends and patterns…. We will be watching to see if the virus acquires traits that make it more virulent and contagious when it returns to the U.S. next fall and winter, as many expect.
From Minnesota:
Dr. Lynfield emphasized that health officials are still concerned about the new flu virus.
“There is a temptation, right now, to assume that any major threat from this new virus has already passed,” Dr. Lynfield said. “It is true that, for now, the virus seems to be causing illness that is generally not severe but that doesn’t mean we should let down our guard.
“Some people have been severely ill with this virus. Deaths have occurred, although not yet in Minnesota. We also don’t know whether this virus will change over time. It could go away over the course of the summer, only to reappear in the fall and cause more severe illness.”
Right now, health officials are responding to developments as they occur, carefully monitoring for changes in the severity of the illness and planning for the possibility of more severe disease. “We need to be alert, respond nimbly and be ready for change,” Dr. Lynfield said.
From Kansas:
“Fortunately most illnesses caused by this virus so far have been relatively mild,” Dr. Eberhart-Phillips said. He noted that of 97 laboratory-confirmed cases in Kansas, there have been only seven hospitalizations and no deaths.
“But that relatively benign picture could change as the virus infects more people around the world, and it has more opportunities to mutate or exchange bits of its genetic material with other flu viruses,” he added. “The severity of illness it causes could be different in the months ahead.”
None of these three details the reassortment nightmare scenario, and none describes what a severe pandemic might be like with any sort of vividness. None goes as far as I would go in warning people that we may be living on borrowed time. But these three states used the WHO Phase 6 declaration as an opportunity to at least mention the possibility of future severity. The other five states did not.
Messaging in the rest of the world
Arguably, the June 11 WHO pandemic declaration was – or could have been – a bigger teachable moment outside North America than it was here. Most of the rest of the world is several weeks behind in its adjustment to the reality of swine flu. The level of interest and anxiety is higher.
It was countries outside North America that led the successful campaign for WHO to delay the declaration, fearing that people would overreact. This is a fear I didn’t share, and one that hasn’t materialized – either the delay worked or there was never much risk of an overreaction in the first place.
Still, the WHO pandemic announcement was a more important event elsewhere than it was in North America. How well did the rest of the world use the event to communicate the three messages that I think are most important?
Once again, I am relying largely on Jody’s surveillance of English-language media and government documents from around the world.

Try to protect yourself. Flu is serious.
The world gets a B- on Message 1 – slightly better than the C+ I gave to the U.S. The international messaging on appropriate precautions is fairly similar to U.S. messaging, with an even stronger and thus more misleading emphasis on the benefits of hand-washing. This focus on transmission via objects (instead of face-to-face, which is how most flu is actually transmitted) seems to have led local officials in several countries to start enthusiastically disinfecting schools and offices and even – in Thailand – streets.
Still, officials in non-Western countries also recommended masks, for protection of both self and others. And we didn’t find any non-Western countries that called swine flu precautions “simple,” which is refreshing, considering how hard it is to follow instructions like “avoid people who are sick.”
Several countries warned explicitly that not all swine flu cases are mild, and that people should anticipate some severe cases and some deaths. Australia even mentioned that “WHO is concerned” about “occasionally severe disease in otherwise healthy young adults.” In many developing countries, in fact, the opposite problem surfaced: news stories and official releases failed to emphasize sufficiently that most cases are mild, and sometimes actually implied that most cases are serious. For example, stories and releases would stress that all of a country’s few local cases had been hospitalized, without noting that the cases were mild and the hospitalizations were more for isolation than for treatment.
One extremely bad example from the opposite end of the spectrum: The Indian health minister minimized the seriousness of swine flu by stating in his own press release, without any nuance, that “there is no cause for panic as the disease is curable.”

Picture how the virus may change.
On Message 2, the world gets a D, slightly worse than the D+ I gave the U.S. Although the WHO pandemic announcement emphasized that the H1N1 virus could become more virulent at any time, that message was seldom picked up in official releases or news stories. At best, countries sometimes implied the message indirectly:
- Singapore: “At this early stage, the pandemic can be characterised globally as being moderate in severity.”
- U.K.: “Flu viruses are known to be unpredictable.”
“At this early stage” and “unpredictable” are the merest hints at the possibility of a more severe pandemic to come. Officials may imagine they are sounding the alarm with statements like these, but only the most attentive and already well-informed citizens would get the message.

Get ready for a much worse pandemic.
Like the U.S., the world gets an F on Message 3. Since there were very few (and very vague) warnings that the swine flu virus might become more virulent, it isn’t surprising that there weren’t any recommendations for people to prepare for that possibility.
One lonely statement might represent a gleam of hope. In its explanation of the purposes of containment, the New Zealand government said that “every week we buy is important for … giving families, schools and businesses a chance to prepare.” The meaning was preparedness for the mild pandemic we’ve got, not the more severe one we might someday face – but at least New Zealand included a message urging nongovernmental preparedness.
The frustrating bottom line: Another teachable moment – at least outside of North America, where people were still paying attention – was largely frittered away.
Posted: June 4, 2009
Swine Flu Pandemic Prospects: Nobody Knows
by Peter M. Sandman
 Not much has changed on the swine flu risk communication front since my May 23 update. If you’re new to this page, I urge you to read that update. If you’ve already read it, here are some new developments (or new observations) of interest:
Not much has changed on the swine flu risk communication front since my May 23 update. If you’re new to this page, I urge you to read that update. If you’ve already read it, here are some new developments (or new observations) of interest:

More cases.
There are, of course, more cases. The gap between confirmed cases and actual cases has doubtless widened as more countries and states have stopped testing everyone with flu symptoms for H1N1. That makes the confirmed case tally less and less relevant, though the media continue to lead with it (in stories that are no longer high-visibility anyhow). But the CDC did recently update its May 15 guesstimate of the real number of U.S. cases from “upwards of 100,000” to “probably several hundred thousand.”
It’s not clear how much higher that guesstimate will get. In the CDC’s May 28 press briefing, Dr. Anne Schuchat said that U.S. influenza reports were declining except in the New York/New Jersey area and the Pacific Northwest/Alaska, “where the influenza-like illness patterns are still increasing.” One week isn’t enough of a trend to say H1N1 is receding for the summer, but it’s starting to look that way.
Outside North America, and especially in the southern hemisphere, there are no signs that swine flu is receding. Australia claims its number of cases is doubling every two days.

Still mild.
Ironically, the focus on the confirmed case tally makes swine flu look much more deadly than it actually is. Reporters – innumerate as always – routinely report both the confirmed case tally and the number of patients who have died. The most recent U.S. totals, for example, are 11,468 cases and 19 deaths. The WHO worldwide totals are 19,315 cases and 117 deaths (97 of them in Mexico). Anyone who divides the latter by the former gets a case fatality rate much higher than the actual rate (since the denominator is missing the 95% or so of probable cases that don’t get tested and confirmed).
Fortunately, reporters don’t do the math. And if they did, most of them wouldn’t realize the resulting CFR was frighteningly high … and grossly misleading. Actually, most swine flu cases continue to be mild. And the real case fatality rate is lower than the rate for the seasonal flu, at least in developed countries, though a much higher proportion of victims are young people (usually young people whose preexisting health problems were manageable until they were badly exacerbated by the onset of flu).

Phase 6 is coming.
The news media have reported leaks from WHO indicating that it plans to ratchet up soon to Phase 6 – declaring swine flu a bona fide pandemic. At around the same time, WHO apparently will subdivide Phase 6 into several (probably three) different severity levels, and will declare the swine flu pandemic to be the lowest of the three so far. I think this is eminently sensible:
- The delay in declaring Phase 6 will have given people time to get used to the idea, and given governments and companies time to scour their pandemic plans for any automatic triggers linked to the WHO phases. But not all countries’ leaders have used the delay to help their citizens anticipate the inevitable declaration of Phase 6. If their citizens overreact when it happens, the leaders will undoubtedly blame them for being “hysterical,” and blame the media for sensationalizing. While we all waited for the Phase 6 declaration, by the way, the world’s stock markets rose substantially, suggesting that investors, at least, do not expect an overreaction with economic repercussions.
- The new severity scale will enable WHO to acknowledge that H1N1 has achieved the widespread, sustained community transmission that characterizes a pandemic, while still emphasizing that H1N1 isn’t a very severe pandemic so far. That should help allay the fears of some governments that their people might overreact to the pandemic declaration. The new severity scale will also let WHO hold two severity categories in reserve, in case H1N1 gets worse (or in case a different pandemic virus emerges) and WHO needs to make a new and more alarming declaration.

Low U.S. interest.
In the U.S., sadly, the public’s interest in swine flu has sunk to near-zero. Except for the panflu preparedness community, and a few places with explosive school outbreaks, H1N1 is discussed – if it is discussed at all – in the past tense, as a scare we all went through a few weeks ago. And interest in pandemic preparedness never rose in the first place. Even when swine flu was big news, pandemic preparedness wasn’t.
The teachable moments to date have been lost. Instead of experiencing swine flu as a warning that a severe pandemic is likely sooner or later (and that even the seasonal flu is a serious disease), many people experienced swine flu as evidence that flu pandemics are no big deal (and that health officials are fear-mongers). It will be harder now, not easier, to find ways to motivate more preparedness.
Even in places like New York City that have experienced intense local outbreaks, interest has begun to wane. Even there, most people seem to have gone through their adjustment reactions and settled into the New Normal. And the New Normal, sad to say, is not much more attuned to flu risks and pandemic preparedness than the old normal was. It might even be less attuned.
The CDC and WHO media briefings have become less frequent. The U.S. media still dutifully cover them, but the resulting stories don’t get very big play. Most medical reporters have resumed their regular routines, and those who are struggling to keep the swine flu story alive end up trying to interest their editors in human-interest swine flu features. Local cases – and especially local deaths – still merit local coverage … so far.

Higher interest elsewhere – for now.
Outside of North America, media and public interest are more intense. Countries with only a few confirmed cases so far are following those few with nervous fascination. Countries that have just begun to confirm larger numbers of cases are following the rising tally with the same nervous fascination.
Unless something changes – like an increase in severity – there is every reason to expect that the rest of the world will probably follow North America’s example: People will get through their adjustment reactions. Then they will sink into complacency and accuse officials and the media of fear-mongering.
The first half of this prediction is virtually guaranteed. People will get through their adjustment reactions. Conceivably, health officials will do better elsewhere than they have done in North America at seizing the teachable moment, so the New Normal is more attentive to pandemic preparedness (and seasonal flu risks) than the old normal was. But don’t count on it. It is very, very difficult to get people to see a mild pandemic as a warning to prepare for a severe one, rather than as evidence that pandemics aren’t such a big deal after all. It is especially difficult to accomplish this when officials are frightened of frightening the public (or being accused of frightening the public) – when their “warnings” that things could get worse are tepid, surrounded by endless assurances that there is no need to worry, much less to prepare.

Unrealistic expectations.
In countries where swine flu is not yet known to be circulating widely, experts agree that it’s only a matter of time before it does so. That doesn’t mean it’s futile to try to “contain” the initial spread of the H1N1 virus. Although containment will ultimately fail, it can slow the spread of H1N1. That buys time – for the development of a vaccine, for example, and for teaching people about non-pharmaceutical interventions. And it flattens the curve so fewer people are sick all at once, which reduces workplace and school absenteeism and the pressure on hospitals and other medical resources.
But instead of explaining that containment is a temporary strategy to slow the spread of the disease, many countries are allowing their people to imagine that they actually intend to stop it. When officials identify and quarantine their first incoming travelers with swine flu, for example, they typically issue self-congratulatory statements implying (or claiming outright) that they can keep the disease from spreading. This failure of anticipatory guidance – “containment will eventually fail, and then here’s what we will do…” – sets governments up for public perplexity and even outrage. People will feel blindsided when their government eventually announces that the virus is now firmly entrenched, and containment measures – screening travelers, tracing contacts, testing all people with flu symptoms, giving them all (and even their contacts) Tamiflu – are abandoned in favor of measures that make more sense once sustained community transmission is established.

Precautions as reassurance.
Another extremely common phenomenon has been the use of swine flu precautions that most experts consider unnecessary, futile, or unwise, presumably in order to reassure anxious members of the public that “everything possible is being done.” (The most extreme possibilities here – such as border closings and swine culls – have been mercifully rare so far.)
In many places, for example, swine flu school closing policies have been vastly different from the policies in place for seasonal flu outbreaks. This was a wise precaution in the early days, before it was clear how severe swine flu illnesses would be. But schools continue to close in response to significantly lower illness and absenteeism rates than have previously been required for such a measure. While closed, the schools are often disinfected far beyond normal flu season cleaning protocols – even though the flu virus lasts only hours to a few days on most surfaces, and even though recontamination is inevitable if the school reopens while H1N1 is still circulating.
Similarly, Tamiflu has often been distributed to healthy young people with mild or even no symptoms – also a defensible measure early on, but much less so as knowledge has increased about H1N1’s relative mildness and which specific groups are at elevated risk. Continuing untargeted use of Tamiflu is a waste of a potentially scarce resource, a risk factor for the development of drug-resistant strains, and a far cry from standard medical practice with regard to the seasonal flu.
These examples of “precaution as reassurance” raise very difficult risk communication issues. Assuming some people are genuinely overanxious and in need of reassurance – a big assumption – is it helpful to respond to their anxiety with precautions that are technically marginal or even potentially harmful? The right answer for potentially harmful precautions is virtually always no. The answer for marginal precautions, I think, depends on whether such precautions will actually be experienced as reassuring. Often they are experienced instead as evidence that the risk is huge, and later (when these marginal precautions are abandoned) as evidence that the authorities are irresolute, inconsistent, and uncaring: “Why aren’t you giving my kid Tamiflu? All the kids in the other school got Tamiflu.” Marginal precautions are probably likelier to be experienced as reassuring if they are explained as responses to public anxiety, rather than simply being deployed as if the authorities thought they were technically sound.
Perhaps most important is to remember that the initial assumption is questionable. Is it really necessary for officials to reassure parents and others about swine flu, or should they be sounding the alarm instead – stressing the seriousness of influenza and the possibility of an increase in H1N1’s severity?
The dilemma of whether to use marginal precautions to reassure people who are overanxious about swine flu is a short-term dilemma. Soon enough the public progresses from anxiety to calm to complacency, and the rationale for precautions as reassurance disappears. But trust in the competence and credibility of officials may have been damaged along the way.

Antipathy to masks.
While some unwise precautions are widely adopted for reasons of reassurance, other precautions are widely shunned … also for reasons of reassurance.
Surgical masks, for example, are in common use in Asia, but in much of the rest of the world (including the U.S.) officials have strongly discouraged their use except in healthcare settings. There isn’t a lot of evidence one way or the other to show whether masks are of any value against influenza. But the logic is inescapable. Most flu is transmitted by droplets. Masks catch many but not all droplets – surely more droplets than sleeves and tissues. And unlike sleeves and tissues, masks provide at least some protection from other people’s droplets. (We all know from experience that we can’t rely on the “kindness of strangers” to cover their coughs and sneezes in crowded places.) Another benefit of masks: In non-Asian cultures, most people try to keep some distance from mask-wearers (is she sick? is she crazy?), which helps accomplish social distancing objectives. So if you’re in a crowded place like a bus or subway, in a community where H1N1 is circulating, and if you want to do your share to slow its spread, wearing a mask makes some sense.
The experts are right that there is no convincing evidence that mask-wearing in crowded public places reduces influenza transmission. But why do they never point out that there is no such evidence for coughing into your sleeve either? Why do they extol the virtues of covering your cough by any means other than masks? Why do they emphasize hand-washing even more than cough hygiene, and far more than protection against other people’s coughs, when they are pretty sure that flu is transmitted less often by hands than by face-to-face droplets? Why do they worry aloud that wearing a mask might give people a false sense of security, a concern they never express about tissues, sleeves, or hand-washing?
There are some sound reasons for questioning the use of masks: cost, discomfort, and possible shortage are the main ones. But it’s reasonably clear that officials are down on masks chiefly because masks vividly convey a sense of risk – and officials don’t want to send any scary messages about swine flu. In many cases, employees with extensive face-to-face public contact (ticket agents, customs officials, bus drivers) have been forbidden to wear masks. The rest of us have merely been discouraged.
Posted: May 23, 2009
Swine Flu Pandemic Prospects: Nobody Knows
by Peter M. Sandman
 The H1N1 swine flu is still spreading slowly around the world, and still usually mild. It hasn’t fizzled. It hasn’t disappeared for the summer in the northern hemisphere. It hasn’t grown more virulent. Any of those changes is possible. Or the spread could stay slow and the cases could stay mild.
The H1N1 swine flu is still spreading slowly around the world, and still usually mild. It hasn’t fizzled. It hasn’t disappeared for the summer in the northern hemisphere. It hasn’t grown more virulent. Any of those changes is possible. Or the spread could stay slow and the cases could stay mild.
“Slow” and “mild”
“Slow” and “mild” are relative terms, of course.
The World Health Organization and the U.S. Centers for Disease Control and Prevention are both continuing to keep a tally of cases. But both organizations concede that the tally greatly underestimates the real number. (No countries are testing every new flu case for H1N1.) On May 15, the CDC estimated the number of U.S. cases as “upwards of 100,000” – a guess it uses fairly routinely in media briefings but hasn’t increased since the 15th. WHO reports only laboratory-confirmed cases, and has offered no estimate for the number of cases worldwide.
So far only a few cities in a few countries have seen explosive local outbreaks, usually in schools. The level of public concern briefly becomes much higher when and where these outbreaks occur. Some parents demand that the authorities close schools where there are only a few cases; some want Tamiflu for all students, healthy as well as sick; some take their almost symptomless children to hospital emergency rooms.
This is still a long way from panic. It’s an adjustment reaction – and it will fade as communities become more accustomed to swine flu outbreaks (as they have become accustomed to seasonal flu outbreaks). School closings, for example, seem to decrease once initial containment efforts fail, except where significant absenteeism interferes with the educational mission.
No one knows how widespread these explosive outbreaks will become, provoking new adjustment reactions in new places. Nor do we know how broadly the virus will spread. Geometric progressions are deceptive. If we assume that H1N1 keeps spreading at a constant rate, it will take the same number of days to grow from a million to a hundred million cases as it took to grow from a thousand to a hundred thousand. Unless the epidemic/pandemic fizzles, at some point “slow” growth will start looking fast.
As for mildness, on May 15 Jody Lanard and I used some preliminary and very tentative guesstimates of swine flu’s case attack rate (CAR) and case fatality rate (CFR) to come up with a projection of 432,000 U.S. swine flu deaths in the coming year. That’s 12 times the estimated number of deaths from a typical flu season – and swine flu deaths so far have included a high proportion of healthy, young people, whereas the seasonal flu takes mostly the elderly. (See “Visualizing a mild pandemic,” where you can also find links to the CAR and CFR estimates, which were published in Science and on the WHO website.)
I doubt that 432,000 U.S. deaths are what most people imagine when they hear that swine flu is “mild.” But 432,000 U.S. deaths may also be a gross overestimate. More recently, WHO and the CDC have said repeatedly that H1N1 is pretty much like the seasonal flu. I haven’t seen any new studies updating and correcting the preliminary ones (based largely on Mexican data) that estimated a CAR roughly three times as bad as the seasonal flu and a CFR roughly four times as bad as the seasonal flu. But I’m guessing that the two agencies have informally decided the early studies were mistaken. The U.S., for example, has reported only ten H1N1 deaths so far; if there have really been upwards of 100,000 U.S. cases, that’s a CFR a lot lower than the seasonal flu, not four times higher.
It’s too soon to tell how disastrous even a mild H1N1 pandemic might be in developing countries, especially those with large immunocompromised populations. But in the developed world, so far, swine flu has kept a lot of kids home sick from school for a week or less … and that’s about all.
Keeping everybody calm
In North America, at least, surveys have shown a decline in public worry about swine flu from low to lower. In a CNN poll conducted May 14–17, for example, 17% of U.S. respondents said they were worried that they or someone in their family could “fall victim to the flu.” Another 20% said they had been worried previously but weren’t anymore; 63% said they were never worried.
For reasons I can’t quite fathom, many governments remain extremely worried about the prospect of a huge public overreaction. They are gripped by what I call “panic panic” – unreasoning fear on the part of officials that their people won’t be able to cope.
Governments vary in how candidly they explain that H1N1 could turn virulent the way the 1918 pandemic did (it also started out mild). But even those that make this point rarely do so with any sense of drama, and rarely urge the public to prepare for the possibility of a more severe pandemic.
Nor are they making much effort to dramatize that even a mild pandemic can have more impact than people are imagining. I have yet to see any health agency produce a video showing how many flu cases and how many flu deaths the world can expect by year’s end if current trends are extrapolated.
To the contrary, a number of governments (including the U.K. and China) have aggressively urged WHO to change its definition of “pandemic” to include some sort of severity measure. The goal is to avoid having to declare H1N1 a pandemic, for fear that the word alone will so terrify people that they’ll demand unwise control measures such as border closings. If these countries get their way, a mild pandemic won’t get called a pandemic anymore. (That will presumably airbrush out not just the mild pandemic of 2009 but also the mild pandemics of 1957 and 1968, so we’ll also be able to say that the twentieth century actually experienced only one influenza pandemic, not three. What a relief!)
It seems those panic-panicked governments are going to get their way. On May 22, WHO said it would consider redefining “pandemic” to take severity into account. Interim Assistant Director-General Keiji Fukuda said: “The bottom line here is that we are trying to walk a very fine line between not raising panic and also not becoming complacent.”
There is no fine line between panic and complacency. There is a yawning chasm between panic (which is rare) and complacency (which is all too common). The dominant swine flu problem remains complacency.
Although I see little merit in WHO’s rationale for redefining “pandemic,” the decision itself is defensible. Arguably, WHO shouldn’t signal its highest level of concern about a virus that is still comparatively mild – not because such a signal would precipitate panic, but for precisely the opposite reason: because such a signal would leave WHO with no viable way to talk about the possibility (or, if it happens, the reality) of a pandemic that is much more virulent.
My concern over the past week has been that WHO would declare a pandemic, people would notice that nothing much had changed in their daily lives, and they would conclude that pandemics are no big deal. That is an outcome worth avoiding.
My wife and colleague Jody Lanard has a different concern. She is saddened that WHO announced it was rethinking its pandemic phase definitions without acknowledging that according to its current definitions (abruptly announced about three weeks ago) swine flu has already gone pandemic, and without acknowledging that according to its previous definitions swine flu went pandemic even earlier.
I am worried mostly about public complacency. Jody is worried mostly about WHO’s credibility. Neither of us is worried about what many of WHO’s member states say they’re worried about: public panic.
Phases of swine flu reaction
In the U.S., I have seen four phases of swine flu reaction so far:

- When the early news from Mexico looked really bad, many people took the risk seriously, especially in North America. The public wasn’t nearly as alarmed as a lot of experts were; reports in the first few days suggested a Mexican case fatality rate as high as eight percent, three times as bad as the 1918 pandemic. Still, it was a pretty big story, and a lot of people took it pretty seriously. Some (not many) even stocked up on food, medicines, and other supplies.

- After a few days, it became clear that things weren’t as bad as the early Mexican reports had suggested. So those who had taken Swine Flu Phase One to heart quite properly reconsidered. They concluded, rightly, that the current situation wasn’t so serious after all. And many of them also concluded, wrongly, that the experts and the media had overreacted in Phase One. Words like “fear-mongering” started to be used. Vigilance and preparedness in case the situation deteriorated began to seem not merely unnecessary, but foolish, even lunatic.

- Over the next couple of weeks, H1N1 kept spreading. The media diligently reported the tally of cases, but not usually the CDC’s explicit assumption that these were just the tip of the iceberg. It became the accepted mainstream opinion that swine flu was a minor medical problem. The judgment that even a mild pandemic could have significant impacts was pretty much ignored, as was the possibility that H1N1 might not stay mild.

In a few places – New York City, for example – explosive local outbreaks made swine flu a major story again. The public (but not the experts) were taken by surprise, and some people therefore (temporarily) overreacted … though they did not panic. During Swine Flu Phases Two and Three many people had accused the authorities of fear-mongering in Phase One; now those same people accused the authorities of failing to take the swine flu problem seriously enough … and failing to warn them that Swine Flu Phase Four was coming.
Here are three alternative predictions for Swine Flu Phase Five:

- People will get used to occasional explosive local outbreaks. They’ll take the belated WHO pandemic declaration (if it happens) in stride. The 2009 pandemic, like the 1957 and 1968 pandemics before it, will be a significant source of mortality and morbidity but not a significant concern for the general public. The teachable moment will have been lost, and preparedness for a more severe second wave of H1N1 – or a more severe H5N1 (or other) pandemic in some future year – will become once again a fringe preoccupation.

- Partly because they were allowed to underestimate the possible health impacts of a “mild” pandemic, people will continue to overreact (but not panic) in response to occasional explosive local outbreaks. When and if WHO belatedly declares H1N1 to be a pandemic after all, public demands for governments to do something – even something foolish – to protect them will be too strong to ignore. Preparedness for a possible severe pandemic to come, or a possible severe second wave of this pandemic, will be impeded by the widespread misperception that the current pandemic is severe already.

- Aided by government messaging that is both candid and dramatic, people will get it that even a mild pandemic isn’t the non-event they might have imagined, and that a more severe pandemic (or pandemic wave) is a possibility too serious to ignore. People will want to take appropriate steps to mitigate what they are facing now and to prepare for what might be coming – and will want their governments to do likewise.
The first #5 is the one I expect. The second #5 is the one most governments are worried about. The third #5 is the goal.
Core risk communication tasks
So we have three core risk communication tasks at the moment:

- Warning people now that the current situation isn’t as benign as they’re imagining – that this mild pandemic will entail a lot of illness and more than a few deaths … and persuading them to take commonsense hygiene measures seriously.

- Warning people now that the situation could get a lot worse than it is so far – helping them envision a severe pandemic and motivating them to prepare for that possibility, emotionally and logistically … all while also helping them bear in mind that it’s only a possibility, not a prediction.

- Planning now what we will say if the situation actually does start getting worse – if a severe pandemic once again looks like it might be imminent (as it looked in the early days of the Mexican outbreak).
All three tasks will be extremely difficult. SARS didn’t go pandemic the only known time it emerged from the wild. Bird flu still afflicts millions of poultry and a tiny number of extremely unlucky humans, but it hasn’t gone pandemic yet either. And swine flu is a mild pandemic (so far) – so mild that the World Health Organization still refuses to use the term. Many laypeople who scoffed at swine flu in the early days think they have been proved right. Many laypeople who took swine flu seriously in the early days think they have been proved wrong. Both groups are going to be very, very skeptical about any new swine flu warnings. (For a typology of swine flu audiences, including these two all-important groups, see “Selling pandemic prep to family and friends.”)
Two years ago, back in WHO Pandemic Phase 3, Jody Lanard and I wrote a long four-part column entitled: “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.” We had two goals for the column.
- The first goal was to offer standby risk communication guidance for the moment when a pandemic looked imminent and potentially severe, and the customary public complacency had given way to riveted attention.
- The second goal was to help officials think through in advance the things they’d need to be saying on the eve of a potentially severe pandemic, in the hope that doing so would make them less skittish about appropriately scary pre-pandemic messaging, and thus more willing to forewarn the public before a pandemic looked imminent.
When swine flu first emerged in late April, I posted a link to that column on my website home page. I thought the first goal applied. It looked like we might very well be on the brink of a potentially severe pandemic, and public attention was substantial.
Nearly a month later, the second goal applies more than the first. Swine flu is now a pandemic in all but name, but a pandemic so mild (so far) that WHO is not yet willing to call it a pandemic at all. Public attention has waned from its late April heights, though it is still considerably greater than it was before the advent of H1N1. More problematically, public attention has become increasingly skeptical.
Though it is not a severe pandemic, at least not yet, swine flu continues to provide teachable moments for talking about preparedness for a severe pandemic. The 25 messages discussed in “What to Say When a Pandemic Looks Imminent” are still the core messages. But they’re going to have to be delivered with a lot of empathy for people’s understandable reluctance to gear up again for a risk that keeps threatening and has yet to deliver.
Posted: May 16, 2009
Swine Flu Pandemic Prospects: Nobody Knows
by Peter M. Sandman
 At the moment, the H1N1 swine flu is still spreading around the world, but s-l-o-w-l-y, not explosively. And the new cases are usually mild.
At the moment, the H1N1 swine flu is still spreading around the world, but s-l-o-w-l-y, not explosively. And the new cases are usually mild.
“Slow” and “mild” are relative terms, of course. As of May 15, the U.S. had recorded at least 173 hospitalized swine flu patients and five swine flu deaths. Out of how many swine flu cases? The CDC maintains a tally of “confirmed” and “probable” cases (which stands at 4,714 as of May 15), but it isn’t trying to keep count; it has expressed the view that the real number of “novel H1N1” infections in the U.S. is upwards of 100,000.
If you assume that swine flu will eventually go pandemic and will remain as mild as it is now, how many Americans will it kill? Using the WHO preliminary and very tentative guesstimates of swine flu’s attack rate and case fatality rate, Jody Lanard and I did the math and came up with 432,000 U.S. swine flu deaths in the coming year. That’s 12 times the estimated number of deaths from a typical flu season – and swine flu deaths may be mostly healthy, young people instead of the sick and elderly. (See “Visualizing a mild pandemic.”) I doubt that’s what most people imagine when they hear that swine flu is “mild.”
But that’s far from the worst (or best) case scenario. Both the attack rate and the case fatality rate could go up, precipitating a much more severe pandemic. Or they could go down, yielding numbers much lower than the ones in the previous paragraph.
So we have three core risk communication tasks at the moment:
- Warning people now that the current situation isn’t as benign as they’re imagining – that guesstimates of what might happen if swine flu goes pandemic without getting any worse (or any better) add up to some pretty upsetting numbers: maybe 100,000,000 new cases of flu (around three times as many as usual) and 432,000 flu deaths in the U.S. alone.
- Warning people now that the situation could get a lot worse than that – helping them envision a severe pandemic and motivating them to prepare for that possibility, emotionally and logistically … all while also helping them bear in mind that it’s only a possibility, not a prediction.
- Planning now what we will say if the situation actually does start getting worse – if a severe pandemic once again looks like it might be imminent (as it looked in the early days of the Mexican outbreak).
All three tasks will be extremely difficult. SARS didn’t go pandemic (yet). Bird flu didn’t go pandemic (yet). Swine flu hasn’t gone pandemic (yet). Many laypeople who scoffed at swine flu in the early days think they have been proved right. Many laypeople who took it seriously in the early days think they have been proved wrong. Both groups are going to be very, very skeptical about any new swine flu warnings.
Two years ago, Jody Lanard and I wrote a long four-part column entitled: “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.” We think the 25 messages discussed in that column are still the core messages. But they’re going to have to be delivered with a lot of empathy for people’s understandable reluctance to gear up again for a risk that keeps threatening and has yet to deliver.
Posted: May 6, 2009
Swine Flu Pandemic Prospects: Nobody Knows
by Peter M. Sandman
 At the moment, the H1N1 swine flu is still spreading around the world, but s-l-o-w-l-y, not explosively. And the new cases are usually mild, although of 1,105 probable and confirmed cases in the U.S., 35 patients are hospitalized (some on ventilators) as of May 5.
At the moment, the H1N1 swine flu is still spreading around the world, but s-l-o-w-l-y, not explosively. And the new cases are usually mild, although of 1,105 probable and confirmed cases in the U.S., 35 patients are hospitalized (some on ventilators) as of May 5.
Neither of these welcome facts – slow spread and mostly mild cases – is guaranteed to remain true. But for now, it looks like we probably have some time: time to figure out what we’ll want to say to people if a severe pandemic starts to look like an imminent possibility again, and time to figure out what to say to people now so they’ll prepare more now and be better primed to hear what we’ll have to say then.
Both tasks – warning people now that the risk is still real, and warning them at some future moment that it looks imminent again – will be extremely difficult. SARS didn’t go pandemic (yet). Bird flu didn’t go pandemic (yet). Swine flu looks to be an extremely mild pandemic if it goes pandemic at all, despite WHO warnings that it may “come back with a vengeance” in the fall. People are going to be very, very skeptical.
Two years ago, Jody Lanard and I wrote a long four-part column entitled: “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.” We think the 25 messages discussed in that column are still the core messages. But they’re going to have to be delivered with a lot of empathy for people’s understandable reluctance to gear up again for a risk that keeps threatening and has yet to deliver.
Posted: April 29, 2009
Swine Flu Pandemic Scare Gets Serious
by Peter M. Sandman
 A never-before-seen influenza virus is transmitting human-to-human. It has infected people in an increasing number of countries and U.S. states – with a significant number of deaths in Mexico. WHO has ratcheted up to Pandemic Phase Five, which means a pandemic is almost certainly inevitable and probably imminent – though its likely severity is still unknowable.
A never-before-seen influenza virus is transmitting human-to-human. It has infected people in an increasing number of countries and U.S. states – with a significant number of deaths in Mexico. WHO has ratcheted up to Pandemic Phase Five, which means a pandemic is almost certainly inevitable and probably imminent – though its likely severity is still unknowable.
Two years ago, Jody Lanard and I wrote a long four-part column entitled “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.”
READ IT NOW.
Posted: April 28, 2009
Swine Flu Pandemic Scare Gets Serious
by Peter M. Sandman
 A never-before-seen influenza virus is transmitting human-to-human. It has infected people in five U.S. states and Mexico – with a significant number of deaths in Mexico. It is by no means a sure thing that a flu pandemic is imminent … but it is now a definite possibility.
A never-before-seen influenza virus is transmitting human-to-human. It has infected people in five U.S. states and Mexico – with a significant number of deaths in Mexico. It is by no means a sure thing that a flu pandemic is imminent … but it is now a definite possibility.
WHO ratcheted up to Pandemic Phase Four on April 27. If it ratchets up to Phase Five, as it may very soon do, that will mean a pandemic is almost certainly imminent – though its likely severity will still be unknown.
Two years ago, Jody Lanard and I wrote a long four-part column entitled “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.”
READ IT NOW.
Posted: April 26, 2009
Swine Flu Pandemic Scare Gets Serious
by Peter M. Sandman
 A never-before-seen influenza virus is transmitting human-to-human. It has infected people in five U.S. states and Mexico – with a significant number of deaths in Mexico. It is by no means a sure thing that a flu pandemic is imminent … but it is now a definite possibility. WHO may ratchet up to Pandemic Phase Four very soon.
A never-before-seen influenza virus is transmitting human-to-human. It has infected people in five U.S. states and Mexico – with a significant number of deaths in Mexico. It is by no means a sure thing that a flu pandemic is imminent … but it is now a definite possibility. WHO may ratchet up to Pandemic Phase Four very soon.
Two years ago, Jody Lanard and I wrote a long four-part column entitled “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.”
READ IT NOW.
Posted: April 24, 2009
Swine Flu Pandemic Scare Gets Serious
by Peter M. Sandman
 A never-before-seen influenza virus has infected people in California, Texas, and Mexico – with a number of deaths in Mexico. It is by no means a sure thing that a flu pandemic is imminent … but it is now a definite possibility. WHO may ratchet up to Pandemic Phase Four very soon.
A never-before-seen influenza virus has infected people in California, Texas, and Mexico – with a number of deaths in Mexico. It is by no means a sure thing that a flu pandemic is imminent … but it is now a definite possibility. WHO may ratchet up to Pandemic Phase Four very soon.
Two years ago, Jody Lanard and I wrote a long four-part column entitled “What to Say When a Pandemic Looks Imminent: Messaging for WHO Phases Four and Five.”
READ IT NOW.
Copyright © 2009–2010 by Peter M. Sandman