The last Swine Flu Pandemic Communication Update on this site was January 17 – five months ago. It made four points:
- We don’t know what’s coming next.
- It’s a real pandemic.
- It’s a mild pandemic, at least so far.
- It’s probably not over – but we don’t know what’s coming next.
That’s about it, really – still … except for the blame game, which is what we are going to analyze below. The extremely long assessment that follows advances an argument we can summarize in a single sentence:
That’s where we’re going.
Where is the pandemic going? In January, swine flu incidence in the northern hemisphere had peaked and was decreasing in many countries, but was still widespread. Now, as summer approaches, it’s quite low. It’s quite low in the southern hemisphere too, but with somewhat higher levels reported in some tropical countries. Seasonal H3N2, the most severe of the seasonal strains, is still circulating at low levels. At this point, unfortunately, it does not appear to have been replaced by the pandemic virus.
Column Table of Contents
WHO’s Failure to Acknowledge the Ongoing Mildness and Current Low Incidence of the Pandemic
Evidence that the swine flu pandemic has been mild so far
WHO’s unwillingness to call the pandemic mild
Explanations and impacts: Why WHO won’t call the pandemic mild, and why that matters
The mistake repeated: WHO’s failure to categorize the pandemic as “post-peak”
About definitions and redefinitions
How and why WHO changed its use of the term “influenza pandemic”
Mishandling the definitional controversy
In other words, there is no clear evidence yet that pandemic H1N1 is or is not going to “act” like a seasonal flu strain from now on, which is what former pandemic flu strains have done after 1–3 years. That’s certainly one of the possibilities, but there are two others. It could cause additional pandemic waves more or less like the ones it has already caused. Or it could get a lot more virulent – which most experts don’t expect at this point but don’t rule out either. (Experts do remember that the mild 1968 pandemic returned to cause a more severe European wave in the winter of 1969–1970, a full year after the very mild first European wave. Almost anything is possible with influenza.)
The pandemic is like a hurricane that initially and briefly looked like it might be a Category 4 whopper, turned out to be just barely a Category 1 hurricane – but still a hurricane – and then dissipated. But unlike a dissipated hurricane, the pandemic isn’t completely gone.
In our daily lives, though, the pandemic feels like it’s over, and for some people it feels like it never happened. Other than ongoing vigilance (surveillance and assessment), precautions are in abeyance in most of the world. The most expensive precaution, a new vaccine, wasn’t ready until after the 2009 northern and southern hemisphere waves were over or receding. Still, the vaccine could have prevented a lot of morbidity and some mortality if it had been ready sooner. And if the pandemic comes roaring back, many people will wish they had availed themselves of the vaccine they so disdained as the last wave receded.
Today, the only individuals continuing to take pandemic precautions are obsessed, and the only individuals complaining that we should never have taken precautions in the first place are ignorant.
As we write this in late June 2010, there is now a huge gap between WHO’s pandemic risk communication and the public’s pandemic risk perception. That is, what most people think they just lived through – a mild pandemic that has virtually disappeared – is radically different from what WHO tells them they are living through: a “moderate” pandemic that is still ongoing.
The result: Widespread skepticism about WHO’s credibility, and thus widespread receptiveness to previously fringe allegations.
“Widespread” is a relative term here. Most people pay virtually no attention to the World Health Organization. They didn’t realize it had a lot of credibility, and they didn’t notice when its credibility collapsed. And WHO’s most devoted followers – many of them public health professionals – have tended to rally round the organization in its hour of need. (Some of them have supported WHO publicly while muttering to each other that it really should stand down from some of its earlier pronouncements.)
But there’s a super-important group in the middle: people who don’t follow WHO closely but who do pay enough attention to have learned first that it seemed to be overstating the seriousness of the swine flu pandemic and then that it was accused of doing so on purpose to help Big Pharma make big bucks. That group includes many of the world’s opinion leaders: corporate executives, government officials, medical reporters, foundation heads, etc. Losing ground in their eyes matters for WHO, and may continue to matter for decades to come.
The collapse of WHO’s credibility is important not just in general because the world needs a credible international health agency, but also, in particular, because WHO’s pandemic warnings about the future (though not its status reports about the present) are right on target. H1N1 could mutate into a much deadlier virus. That would be unusual after a year, but not unprecedented. The world could also face another pandemic in the near future, caused by another novel flu virus. There was apparently a flu pandemic in 1830–31 and another in 1833. The 1968 pandemic started less than ten years after the 1957 pandemic ended. And of course all flu-watchers know that the extremely deadly H5N1 bird flu virus is still Out There. If bird flu ever starts transmitting easily from humans to humans, it’s a whole new ball game.
It is very hard for WHO to convince people – governments, journalists, ordinary citizens – to take the near-term pandemic risk seriously as long as WHO keeps describing the past year’s pandemic experience in ways they simply cannot take seriously.
Introduction
WHO’s Failure to Acknowledge the Ongoing Mildness and Current Low Incidence of the Pandemic
Evidence that the swine flu pandemic has been mild so far
WHO’s unwillingness to call the pandemic mild
Explanations and impacts: Why WHO won’t call the pandemic mild, and why that matters
The mistake repeated: WHO’s failure to categorize the pandemic as “post-peak”
About definitions and redefinitions
How and why WHO changed its use of the term “influenza pandemic”
Mishandling the definitional controversy
![]() The one-year anniversary of the identification of the new swine-origin H1N1 influenza virus came in late April, 2010. The media ran a lot of anniversary stories. Some health agencies issued anniversary news releases, often featuring “lessons learned” about what had gone well and not so well. The Center for Infectious Disease Research & Policy (CIDRAP) at the University of Minnesota did a whole series of anniversary stories. In preparation for one on communication lessons learned, Lisa Schnirring of CIDRAP sent us a list of questions. We dutifully wrote answers and posted them on this site.
The one-year anniversary of the identification of the new swine-origin H1N1 influenza virus came in late April, 2010. The media ran a lot of anniversary stories. Some health agencies issued anniversary news releases, often featuring “lessons learned” about what had gone well and not so well. The Center for Infectious Disease Research & Policy (CIDRAP) at the University of Minnesota did a whole series of anniversary stories. In preparation for one on communication lessons learned, Lisa Schnirring of CIDRAP sent us a list of questions. We dutifully wrote answers and posted them on this site.
The one-year anniversary of the World Health Organization’s (WHO) declaration of a full-fledged “Phase 6” pandemic was June 11, 2010. There were only a few anniversary stories.
This site’s Swine Flu Pandemic Communication Update about the Phase 6 declaration, posted on June 17, 2009, was entitled “Would you like another wakeup call?” It noted that: “For those who were already awake to pandemic realities and possibilities, [the WHO pandemic declaration] was basically a nonevent – a welcome if belated confirmation of what we knew.”
But in retrospect, the WHO pandemic declaration a year ago looks to many (though not to us) like a big mistake, or even an intentional deception. It was already pretty clear by mid-June 2009 that the pandemic was mild so far, more like the last two pandemics than like the nightmare possibility experts had warned about. But it was early days yet. It was perfectly possible that the pandemic could become much more virulent. (The first wave of 1918’s horrific pandemic was also mild.) Now, a year later, that possibility looks much slimmer. It can’t yet be ruled out; flu is famously unpredictable. But at this point it would be a big surprise. And so, with 20-20 hindsight, a lot of people think the initial pandemic declaration was unjustified.
Four things happened in early June 2010 that make this a compelling risk communication story, a fit but sad ending to the saga of Swine Flu Pandemic Risk Communication (Volume One).

WHO sticks to Phase 6.
On June 3, WHO Director-General Margaret Chan issued a statement summarizing the results of a June 1 teleconference meeting of the Emergency Committee that advises WHO on the H1N1 pandemic.
Dr. Chan said that “while pandemic activity is continuing, the period of most intense pandemic activity appears likely to have passed for many parts of the world.” That wasn’t sufficient, however, to persuade the committee to advise her to downgrade the pandemic to WHO’s “post-peak” phase, when “pandemic activity appears to be decreasing” but “it is uncertain if additional waves will occur.” All of the supporting data in the June 3 statement would seem to match the WHO definition of “post-peak,” but WHO did not stand down from Phase 6.
Nor did WHO seize the opportunity to stand down from its insistence that the H1N1 pandemic has been “moderate” so far, as opposed to “mild.”

The Council of Europe attacks WHO.
Also on June 3, the Parliamentary Assembly of the Council of Europe published an utterly bizarre report
 reiterating charges that WHO had foisted on the public a fake pandemic, and had done so partly in order to enrich the pharmaceutical industry. To facilitate this deception, the report claimed, WHO changed its definition of the term “pandemic” and systematically avoided transparency and accountability mechanisms that would have publicly exposed the conflicts of interest that underlay the fraud.
reiterating charges that WHO had foisted on the public a fake pandemic, and had done so partly in order to enrich the pharmaceutical industry. To facilitate this deception, the report claimed, WHO changed its definition of the term “pandemic” and systematically avoided transparency and accountability mechanisms that would have publicly exposed the conflicts of interest that underlay the fraud. The charges in the report were not unexpected, since they had been ventilated months earlier in public statements, a formal motion, and a hearing – at which WHO Special Advisor on Pandemic Influenza Keiji Fukuda was questioned. Still, publication of the report demonstrated Council support for the charges, even after hearing Dr. Fukuda’s defense. The Council of Europe isn’t part of the European Union; its decisions aren’t binding. But with 47 member states, it does influence public debate and sometimes future government decision-making.

BMJ joins the attack.
On the same day, BMJ (formerly the British Medical Journal) published an article charging that WHO committee members often have conflicts of interest that are not revealed to the public. The article was written jointly by the journal’s features editor and a journalist from the Bureau of Investigative Journalism, a nonprofit group launched on April 26, 2010, “to expose the exploitation of the weak by the strong” and “to reveal the failures of those in power to fulfill the trust placed in them.” The article focused on three members of an earlier WHO committee that in 2004 had advised WHO to recommend large national pre-pandemic stockpiles of antiviral drugs. It pointed out some connections between those three committee members and the companies that manufacture and sell antivirals.
Publication of the BMJ article and the Council of Europe report was coordinated. On June 4 the principal author of the latter, Paul Flynn, posted on his blog: “One of the joys today was giving evidence with the editor of the splendid British Medical Journal. We have never met before but we cooed in harmony and just avoided saying it was the Pharmas that did it.”

WHO responds to its critics.
WHO responded to the charges in a June 8 open letter to BMJ, and again in a June 10 response to both organizations. It asserted that the pandemic was real, that the definition of a pandemic had not changed, and that WHO’s pandemic decision-making was completely uninfluenced by commercial interests. But it conceded that changes were needed in transparency policies regarding conflict of interest.
That’s the big swine flu risk communication story now, the biggest in months: In June 2010, the credibility of the World Health Organization crashed and burned. Charges that it had manufactured a fake pandemic in deference to the economic interests of Big Pharma gained mainstream attention.
These charges gained traction at this time, in our judgment, not because they are valid (they are not) but because WHO has badly mishandled certain aspects of its pandemic risk communications.
WHO has made three fundamental errors. In diminishing order of importance, they are:
- Failing to acknowledge that the pandemic has been mild overall, and that its incidence is now quite low. By “mild,” we mean similar to certain previous flu pandemics that WHO has long characterized as “mild” or “relatively mild.” By contrast, WHO has insisted on calling this pandemic “moderate” instead. And its tone has often left people feeling as if it were claiming “severe.”
- Failing to acknowledge that WHO changed some flu pandemic definitions and descriptions just as H1N1 was emerging. The technical meaning of the term “influenza pandemic” is debatable, as is the question of whether a mild flu pandemic should be called a pandemic at all. When WHO changed some of its definitions and descriptions of flu pandemic phases in ways that de-emphasized severity, it opened the door to suspicion that it had “changed the definition of a pandemic” in order to make sure H1N1 would qualify.
- Failing to acknowledge – until June 2010 – that WHO transparency about conflicts of interest had become inadequate. WHO’s earlier response to conflict-of-interest charges was to explain its policies and offer reassurance that the policies work. It wasn’t until after the two recent attacks that WHO began to concede that in the face of the public’s profound loss of trust, it may need to be both tougher and more transparent about its expert advisors’ conflicts of interest.
We must immediately concede that “failing to acknowledge” in these three bullet points is an overstatement. In their millions of words about the swine flu pandemic, WHO officials have periodically made statements that can be read as acknowledging all the points we’re accusing them of failing to acknowledge. We would be on safer ground claiming that WHO officials have failed to get these acknowledgments across. But that would imply that they were trying to do so. They weren’t. The main thrust of WHO pandemic communications has been, and continues to be, that H1N1 is a pandemic of moderate intensity that requires a continued “Phase 6” response; that H1N1 unambiguously meets the consensus definition of an influenza pandemic which has not been changed; and that WHO deliberations about how to manage H1N1 have been sufficiently transparent and self-evidently free of dangerous conflicts of interest.
That, we believe, is why WHO’s credibility is seriously threatened, and its ability to warn the world about future pandemic threats seriously compromised.
To understand what is behind the serious recent damage to WHO credibility, we are going examine these three failures in detail.
Such a detailed examination is worthwhile, we think, for two reasons:
- First, we hope to make a contribution to the world’s understanding, and to WHO’s understanding, of what happened – of how the World Health Organization managed to do severe damage to its own credibility – not by the way it handled the technical side of the twenty-first century’s first influenza pandemic (it did a creditable job), but by the way it handled its risk communication during that pandemic. WHO has appointed an external review committee
 chaired by Dr. Harvey Fineberg to assess the “Functioning of the International Health Regulations (2005) in Relation to Pandemic (H1N1) 2009.” We hope this long column will help Dr. Fineberg’s committee see the pivotal role risk communication has played in WHO’s pandemic credibility crisis.
chaired by Dr. Harvey Fineberg to assess the “Functioning of the International Health Regulations (2005) in Relation to Pandemic (H1N1) 2009.” We hope this long column will help Dr. Fineberg’s committee see the pivotal role risk communication has played in WHO’s pandemic credibility crisis. - Second, we believe we are writing not just about what happened, but also about what happens. The H1N1 pandemic is not the only time WHO’s top scientists’ inattention to risk communication has been its Achilles heel, and WHO is not the only organization that has been damaged by its technical leaders’ inattention to risk communication. Many of the more specific phenomena discussed in this article – for example, WHO’s reluctance to make changes that might be seen as caving in to pressure – are also generic. We hope readers who don’t share our longstanding fascination with the World Health Organization and with influenza pandemics will nevertheless find parts of this analysis illuminating.
For readers who don’t want to delve that deep, we hope the foregoing introduction will have been of interest.
WHO’s Failure to Acknowledge the
Ongoing Mildness and Current Low Incidence of the Pandemic
Column Table of Contents
WHO’s Failure to Acknowledge the Ongoing Mildness and Current Low Incidence of the Pandemic
Evidence that the swine flu pandemic has been mild so far
WHO’s unwillingness to call the pandemic mild
Explanations and impacts: Why WHO won’t call the pandemic mild, and why that matters
The mistake repeated: WHO’s failure to categorize the pandemic as “post-peak”
About definitions and redefinitions
How and why WHO changed its use of the term “influenza pandemic”
Mishandling the definitional controversy
![]() In a sense the question of whether the swine flu pandemic is mild, moderate, or severe is a stupid question, because in a sense it’s unanswerable. Severity is intrinsically comparative: severe compared to what? A severe chest cold isn’t as severe as a severe case of pneumonia. A mild cold is milder than a mild case of pneumonia. An individual’s severe case of influenza during a “mild” influenza year is much more severe than flu’s impact on the community that year.
In a sense the question of whether the swine flu pandemic is mild, moderate, or severe is a stupid question, because in a sense it’s unanswerable. Severity is intrinsically comparative: severe compared to what? A severe chest cold isn’t as severe as a severe case of pneumonia. A mild cold is milder than a mild case of pneumonia. An individual’s severe case of influenza during a “mild” influenza year is much more severe than flu’s impact on the community that year.
Nevertheless, assessing pandemic severity during the course of a pandemic is crucial for planning and response.
There is no obvious methodology for constructing a flu pandemic severity scale. The twentieth century had three influenza pandemics. The most recent, in 1968, is thought to have killed around a million people worldwide. The previous one, in 1957, is thought to have killed around two million people – more than twice as bad, given the smaller global population then. The one before that, in 1918, is thought to have killed 40–50 million people (at a time when there were far fewer people in the world). Estimates of the severity of earlier pandemics are even less reliable than estimates of the severity of these three.
So try to construct a flu pandemic severity scale grounded in three data points – one million, two million, and 40–50 million. You can’t. Obviously, both one million and two million look incredibly mild compared to 40–50 million. Almost any pandemic is going to look mild compared to 1918.
So you throw in seasonal flu as another basis for comparison. And maybe you imagine the worldwide disaster – far worse than 1918 – that would result if the incredibly deadly bird flu started spreading easily among humans the way it already does among birds, without becoming drastically less virulent in the process.
Add some more context: Pandemics come in waves, and the severity of one wave isn’t much of a predictor of the severity of the next. The horrific 1918 pandemic had a mild first wave.
Maybe you abandon death tolls as your measure of severity and look instead at societal disruption. 1918 was huge, right up there with World War One as an epochal event for that generation. By contrast, the world took 1957 and 1968 in stride. Public health professionals considered them important events, and obviously so did the families of those who died. But for most ordinary people they were barely noticeable at the time, and they are barely remembered today by those who lived through them.
The best way to construct your pandemic severity scale: Combine several factors that make sense for planning and response purposes, and adjust them as you learn more about what factors correlate with useful planning and response decisions – an iterative process, similar to WHO’s attempts to improve its pandemic phase definitions over the years.
Here’s why characterizing the mildness of the swine flu pandemic matters. WHO’s most important job when H1N1 first emerged was to warn the world to get ready for an event that might be really deadly and really disruptive – maybe as bad as 1918; maybe even worse; maybe not that bad but still really deadly and disruptive. WHO did that job pretty well. WHO’s most important job a few months later was to stand down: to tell the world that swine flu wasn’t turning out very deadly or disruptive so far, though it still could take a turn for the worse. WHO failed at that job – largely because it was unwilling to call the pandemic “mild.”
This section of the column is in four parts, as follows:
Evidence that the swine flu pandemic has been mild so far
![]() If you already think the swine flu pandemic has been mild so far, as most people do, feel free to skip to “WHO’s unwillingness to call the pandemic mild.”
If you already think the swine flu pandemic has been mild so far, as most people do, feel free to skip to “WHO’s unwillingness to call the pandemic mild.”
One of us (Peter) has written extensively before about the mildness of the H1N1 pandemic in the United States, and the reluctance of U.S. officials to call it mild. See “It’s Official (sort of): The Swine Flu Pandemic Is Mild So Far,” a December 2009 Swine Flu Pandemic Communication Update that compares U.S. swine flu mortality estimates with estimates from other pandemics and from seasonal flu. That update provoked a fair amount of controversy, leading to a December 15 “Update on the December 2 Update” that accepted some criticisms and rebutted others.
We don’t need to recapitulate the entire previous argument, but we do need to look at some numbers.
There are no worldwide numbers – not even semi-official seat-of-the-pants guesstimates. WHO maintains a list of confirmed swine flu deaths, but everyone agrees that’s a gross underestimate, since most suspected cases around the world are never sent for laboratory confirmation; many never even make it to a hospital. The U.S. and a few other countries have developed ways to model national swine flu mortality, but there are no comparable models in the developing world. The same is true for other measures of pandemic severity, such as the number of cases, the number of hospitalizations, the amount of work absenteeism, etc. Once the pandemic has been declared over, there will eventually be an effort to estimate the relevant parameters. We’ll end up with numbers for worldwide swine flu deaths, cases, hospitalizations, etc. The numbers will be very approximate, but we’ll get some global numbers to compare with the even-more-approximate global numbers for past pandemics. We don’t have any yet.
So even though our overall focus is on WHO and the question of worldwide mildness/severity, here we’re going to rely on modeling data from the United States. Let’s look at some key severity criteria.

Death rate.
One obvious standard for assessing the severity of an infectious disease outbreak is how many people it kills. The U.S. CDC estimates that in recent years seasonal flu-related illness has killed an average of about 36,000 Americans a year. The CDC also estimates that in the first year of the H1N1 pandemic (April 2009 to April 2010), between 8,870 and 18,300 Americans died from swine flu – between one-quarter and one-half the number of deaths in an average seasonal flu year.
The assumptions underlying the two sets of estimates are different, but not different enough to account for this huge divergence. In the U.S., at least, swine flu was less deadly than the average flu season.
How about swine flu versus earlier pandemics? Here’s a chart of U.S. government estimates:
Year Est. deaths U.S. Est. pop. U.S. (3) Est. rate U.S. 1918–19 500,000 (1) 104 million 0.481% 1957–58 70,000 (1) 175 million 0.040% 1968–69 34,000 (1) 202 million 0.017% 2009–10 8,870–18,300 (2) 309 million 0.003–0.006% (1) http://www.hhs.gov/pandemicflu/plan/appendixb.html (Table B-1)
(2) http://www.cdc.gov/h1n1flu/estimates_2009_h1n1.htm
(3) http://www.census.gov/popest/archives/1990s/popclockest.txtWith today’s U.S. population of 309 million, a pandemic as deadly as 1968 would kill about 52,000 people in the U.S. – about the same as a severe H3N2 seasonal flu. According to CDC estimates, the first year of the 2009–10 swine flu pandemic was one-third to one-sixth as deadly as the mildest previous pandemic on record, 1968–69.
Prior to the start of the H1N1 pandemic, the U.S. Department of Health and Human Services developed a five-category Pandemic Severity Index
 (PSI). Category 1, the lowest level of pandemic severity, is defined as a pandemic with a case fatality rate (CFR) of less than 0.1% – less deadly than the average seasonal flu. Using the current U.S. population and the conventional assumption that 30 percent of the population gets sick in a flu pandemic, the PSI calculates that a CFR of less than 0.1% would lead to fewer than 90,000 U.S. deaths. That’s the mildest pandemic on the U.S. Pandemic Severity Index: fewer than 90,000 deaths. With an estimated 8,870 to 18,300 U.S. deaths so far, the H1N1 pandemic is essentially off the scale – the poster child of a milder-than-mild pandemic.
(PSI). Category 1, the lowest level of pandemic severity, is defined as a pandemic with a case fatality rate (CFR) of less than 0.1% – less deadly than the average seasonal flu. Using the current U.S. population and the conventional assumption that 30 percent of the population gets sick in a flu pandemic, the PSI calculates that a CFR of less than 0.1% would lead to fewer than 90,000 U.S. deaths. That’s the mildest pandemic on the U.S. Pandemic Severity Index: fewer than 90,000 deaths. With an estimated 8,870 to 18,300 U.S. deaths so far, the H1N1 pandemic is essentially off the scale – the poster child of a milder-than-mild pandemic. The 1968-69 pandemic, by the way, killed about one million people worldwide, according to a WHO estimate. The world’s population at the time was 3.6 billion, yielding a death rate of 0.028%. Today the world’s population is 6.8 billion. To achieve a death rate equal to that of the 1968 pandemic – almost universally remembered as mild – the 2009 global pandemic death toll would have to be about 1.9 million people.
The World Health Organization doesn’t have a Pandemic Severity Index. But long before swine flu, WHO did have an official estimate of how many people a mild pandemic would kill worldwide: two million to 7.4 million. (Sometimes the higher number appears as “7.8 million” or just “seven million.”)
A WHO document entitled “Avian Influenza: Assessing the Pandemic Threat,”
 for example, says: “The mortality of the previous century’s three pandemics varied enormously…. Best-case scenarios, modeled on the mild pandemic of 1968, project global excess deaths in the range 2 million to 7.4 million.” Another WHO document attributes the “two to 7.4 million” estimate to modeling of the more severe 1957 pandemic, still considered “mild” or “relatively mild” by most experts. And in a 2005 presentation
for example, says: “The mortality of the previous century’s three pandemics varied enormously…. Best-case scenarios, modeled on the mild pandemic of 1968, project global excess deaths in the range 2 million to 7.4 million.” Another WHO document attributes the “two to 7.4 million” estimate to modeling of the more severe 1957 pandemic, still considered “mild” or “relatively mild” by most experts. And in a 2005 presentation  to the Science and Technology Committee of the U.K. House of Lords, WHO’s then pandemic czar, Klaus Stöhr, attributes this estimate to both of the two “mild” prior pandemics:
to the Science and Technology Committee of the U.K. House of Lords, WHO’s then pandemic czar, Klaus Stöhr, attributes this estimate to both of the two “mild” prior pandemics:The models, which are being based on 1957 and 1968, would anticipate that in a mild pandemic between 25 to 35 per cent of the population would be infected…. Around about one per cent would be so ill that they would have to be hospitalised and 0.2 or 0.3 per cent would die. These are the figures that are being based on the pandemics in 1957 and 1968, which were very mild pandemics. The total number of deaths would then be two million to 7.8 million deaths and there would be up to 28 million hospitalisations.
Because of the general health of the population and the availability of health care, it is quite possible that the U.S. swine flu pandemic death rate, and that of other developed countries, will turn out to be lower than the death rate for the world as a whole. This was true for the U.S. vis-à-vis the world in past flu pandemics. Let’s guesstimate that the global rate will be three times as high as the estimated U.S. rate. Instead of 0.003–0.006 percent of the U.S. population, let’s assume that 0.009 to 0.018 percent of the world population dies of swine flu. That’s still a lot lower than the 0.028 percent WHO estimate for the 1968 pandemic. With the current world population of 6.8 billion, it comes out to 612,000 to 1,224,000 worldwide deaths – far lower than WHO’s “best-case planning scenario” of two to 7.4 million deaths.

Years of life lost.
Swine flu killed a smaller percentage of people in the U.S. than the average seasonal flu or any previous flu pandemic. However, most of the U.S. victims were significantly younger. The CDC estimates that about 90 percent of seasonal flu deaths in the U.S. are 65 or older; many are a lot older and very frail. By contrast, CDC data show that the swine flu pandemic killed a higher proportion of 50–64-year-olds than any other age group. U.S. death rates for people aged 25–49 and those aged 65+ were about equal. Young people 0–24 were least likely to die from swine flu – but their death rate was still a lot higher than for the seasonal flu.
When healthy young people die, of course, they lose more years of life expectancy than when elderly people die. And most of us feel that deaths of young people are more tragic than deaths of the elderly, especially elderly people who are sick and frail.
Measured in terms of years of life lost (YLL), swine flu has been more serious than simple death rates can show. It cut many young and middle-aged lives short.
A much-cited 2010 study by Cecile Viboud and colleagues tries to compare the swine flu pandemic in YLL terms with previous pandemics and seasonal flu averages. After adjusting for differences in population size, the authors build a case that the swine flu pandemic cost a lot more years of life in the United States than a bad flu season, and probably more years of life than the 1968–69 pandemic, though fewer years of life than the 1957–58 pandemic. Here are the key estimates:
1957 pandemic: 2,698,000 years of life lost 2009 pandemic: 1,973,000 years of life lost 1968 pandemic: 1,693,000 years of life lost Average recent bad flu season: 594,000 years of life lost The authors aren’t trying to say that the swine flu pandemic was worse than the two previous pandemics, which are conventionally called mild. Rather, they are disputing the convention, trying to change what “mildness” means when applied to an influenza pandemic. Based on YLL, they think that none of the three pandemics – 1958–59, 1967–68, or 2009–10 – should be called mild. Even a flu pandemic that kills fewer people than an average flu season and causes minimal societal disruption shouldn’t be called mild, their argument implies, simply because it kills significant numbers of non-elderly people.
Of course there would still be a need for some sort of flu pandemic severity index; perhaps theirs would start with “moderate” and go up from there.
The Viboud study concludes that H1N1 “had a substantial health burden in the US over the first few months of circulation in terms of years of life lost, justifying the effort to protect the population with vaccination programs.” We have no quarrel with this conclusion. Measured in terms of YLL, the swine flu pandemic was roughly comparable to the two previous pandemics, probably worse than 1968 but not as bad as 1957. Whether we call that “mild” or not, it certainly wasn’t a nonevent. Even if officials had somehow known from the start that swine flu wouldn’t get any worse than that, a swine flu vaccine could have saved many young and middle-aged lives if it had been ready sooner. It may still save many lives if further pandemic waves occur around the world.
It is a little off-putting to see so many flu professionals suddenly latch onto YLL as their rationale for claiming the swine flu pandemic wasn’t all that mild. These are the same people who have made maximum noise for years about the annual average of 36,000 U.S. flu deaths – without much inclination to restate that number in YLL terms, since so many seasonal flu victims are already old and frail. Flu specialists have complained for decades that influenza doesn’t get enough funding or attention. If public health departments decide to prioritize diseases in terms of years of life lost, influenza will get even less funding and attention.
To the best of our knowledge, no official pandemic planning document has ever quantified potential severity in terms of years of life lost – though such documents routinely point out that the 1918, 1957, and 1968 pandemics all killed much younger people on average than the seasonal flu, just as the 2009 pandemic has done. (Numerous published studies have used YLL calculations in influenza vaccine prioritization models.) The U.S. Pandemic Severity Index measures severity in terms of case fatality rates and the resulting death tolls. So does WHO’s oft-used scenario of two to 7.4 million deaths.
Not until the H1N1 pandemic turned out mild did flu experts start recommending that we look at pandemic deaths differently. YLL has entered the conversation about the “mildness” of the swine flu pandemic as an argument for the “don’t call it mild” side.
YLL is nonetheless a valid standard to consider, right along with death rate (and other standards), as a measure of infectious disease severity. Death rate ignores the age of the victims. YLL emphasizes the age of the victims. (Sometimes it over-emphasizes the age factor. Is it obviously a worse tragedy when a 30-year-old mother loses her baby than when a baby loses her 30-year-old mother? YLL calculations say it is.) Both YLL and death rate provide useful information. Either standard alone provides information that both informs and misleads. Cherry-picking the standard that helps you make the point you want to make is what propagandists do. Scientists and risk communicators should use a range of standards, so the public is informed enough to make its own assessment.
By the YLL standard, the swine flu pandemic was less mild than by the death rate standard. It was roughly on a par with the two previous pandemics, 1957 and 1968, which are generally considered to have been pretty mild pandemics. YLL points to a way in which all three pandemics can be seen as not so mild after all. And it points to a way in which the last decade of seasonal influenza, even the bad years, can be seen as much milder than flu experts usually imply, since it killed mostly the elderly who had very few years of life left.

Other standards.
Case attack rates and hospitalization numbers are two additional measures of pandemic severity. The U.S. CDC estimates that swine flu made more people in the U.S. sick than seasonal flu usually does, and that it sent more of them to the hospital than seasonal flu usually does. But it killed fewer of them, though the people it killed were much younger.
Those who argue that the swine flu pandemic hasn’t been mild often point to complaints by hospital staff that their intensive care units (ICUs) were periodically overwhelmed with swine flu patients, something that rarely happens during most flu seasons. Given that swine flu killed fewer of its victims, one possible explanation is the age bias of medical care: Perhaps frail elderly seasonal flu patients are more often left to die in nursing homes or at home, whereas younger pandemic patients (especially children) were likelier to be hospitalized … and usually cured. There are other possible explanations. In some places the pandemic may have been more concentrated in time than most seasonal flu outbreaks are. ICU disruptions are less a function of the number of urgent cases over an entire season than of the number of urgent cases at the same time.
A major worry about flu pandemics (and even bad seasonal flu years) is absenteeism, which can disrupt schools, hospitals, and workplaces. In today’s world, a severe pandemic (such as 1918 or worse) could have knock-on effects that contribute significantly to mortality and morbidity: garbage not picked up, crops not harvested, nothing on store shelves, power failures, etc. Before the appearance of swine flu, when pandemic thinking was dominated by the specter of bird flu – which still represents the Ghost of Pandemics Future – many commentators (including us) argued that threat to infrastructure was the biggest pandemic preparedness issue. For example, when vaccine is in short supply during a severe pandemic, vaccinating people in essential occupations should be a higher priority than vaccinating those made more vulnerable by pre-existing conditions.
It is a measure of how mild the swine flu pandemic has been that nothing like this happened in 2009. (Or in 1957 or 1968, two other mild pandemic years.) One of us (Peter) is part of an initiative directed by the University of Minnesota Center for Infectious Disease Research & Policy (CIDRAP) to prepare companies to cope with a pandemic. We have warned endlessly about the threat of supply chain disruptions when suppliers and shippers experience serious absenteeism because their employees are sick, dead, or frightened. The swine flu pandemic caused very few such disruptions – not because supply chains aren’t fragile (they are) but because the pandemic never got very bad.
It is important to stress that “mild” doesn’t mean the first year of the H1N1 pandemic was a nonevent. Many people died; more were hospitalized; many more endured a miserable week. The death toll of children, pregnant women, and other young and middle-aged people was far higher than in a typical flu season, even though the total number of deaths (in the U.S., at least) was lower. Some emergency rooms and ICUs were stretched to their limits. And there were places where high levels of pandemic anxiety – itself a significant health effect – began before the pandemic arrived and continued after the pandemic receded.
From a public health perspective, the most important fact about the H1N1 pandemic in 2009 isn’t what happened. It’s what could have happened. We believe the evidence is incontrovertible that the pandemic has been mild so far. But there was no way to know that at the outset. WHO and health officials around the world were absolutely right to sound the alarm. Their problem – WHO’s problem in particular – was failing to modulate the alarm as the months passed.
WHO’s unwillingness to call the pandemic mild
![]() On April 29, 2009, just days after the world found out about the new swine flu virus, WHO Director-General Chan announced that she was raising the pandemic level to Phase 5, signaling that a pandemic was almost certainly about to occur. Dr. Chan mentioned the severity question but wisely said there was no basis yet for an answer:
On April 29, 2009, just days after the world found out about the new swine flu virus, WHO Director-General Chan announced that she was raising the pandemic level to Phase 5, signaling that a pandemic was almost certainly about to occur. Dr. Chan mentioned the severity question but wisely said there was no basis yet for an answer:
The biggest question, right now, is this: how severe will the pandemic be, especially now at the start?
It is possible that the full clinical spectrum of this disease goes from mild illness to severe disease. We need to continue to monitor the evolution of the situation to get the specific information and data we need to answer this question.
She warned that “From past experience, we also know that influenza may cause mild disease in affluent countries, but more severe disease, with higher mortality, in developing countries.”
This well-nuanced speech ended with a pep talk that included an unfortunate phrase:
Above all, this is an opportunity for global solidarity as we look for responses and solutions that benefit all countries, all of humanity. After all, it really is all of humanity that is under threat during a pandemic.
Pretty clearly, Dr. Chan meant to say only that pandemics spread worldwide by definition, and thus a united global response would be important. But that final phrase – “all of humanity is under threat” – was later used as evidence that WHO had hyped the pandemic from the outset. And that phrase might actually have contributed to pandemic hype on the part of public health officials in developing countries, who started addressing their own populations with phrases like the “dreaded” H1N1.
Two weeks later on May 11, still very early in what was to become the H1N1 pandemic, WHO published “Assessing the severity of an influenza pandemic,” its first important overview of swine flu severity. It started by warning that such an early assessment was necessarily tentative:
Even a pandemic virus that initially causes mild symptoms in otherwise healthy people can be disruptive, especially under the conditions of today’s highly mobile and closely interdependent societies. Moreover, the same virus that causes mild illness in one country can result in much higher morbidity and mortality in another. In addition, the inherent virulence of the virus can change over time as the pandemic goes through subsequent waves of national and international spread….
During the previous century, the 1918 pandemic began mild and returned, within six months, in a much more lethal form. The pandemic that began in 1957 started mild, and returned in a somewhat more severe form, though significantly less devastating than seen in 1918. The 1968 pandemic began relatively mild, with sporadic cases prior to the first wave, and remained mild in its second wave in most, but not all, countries.
Notice that WHO was perfectly comfortable calling the first waves of the 1918, 1957, and 1968 pandemics “mild.”
Then WHO offered its “assessment of the current situation,” stressing that it was “preliminary, based on limited data in only a few countries.” The key paragraph said:
With the exception of the outbreak in Mexico, which is still not fully understood, the H1N1 virus tends to cause very mild illness in otherwise healthy people. Outside Mexico, nearly all cases of illness, and all deaths, have been detected in people with underlying chronic conditions.
WHO stressed that more of the world’s population in 2009 than in 1968 was living with such underlying chronic conditions. Moreover, the disease wouldn’t necessarily remain mild in healthy people:
In these early days of the outbreaks, some scientists speculate that the full clinical spectrum of disease caused by H1N1 will not become apparent until the virus is more widespread. This, too, could alter the current disease picture, which is overwhelmingly mild outside Mexico. Apart from the intrinsic mutability of influenza viruses, other factors could alter the severity of current disease patterns, though in completely unknowable ways, if the virus continues to spread.
This is just about perfect: So far H1N1 is “overwhelmingly mild outside Mexico,” life-threatening only for people with underlying conditions. But it’s very early days yet. Other flu pandemics have started out mild too, even the very severe pandemic of 1918. What WHO knew so far about the mildness of H1N1 could easily change, and so could H1N1 itself.
Some things did change. Swine flu turned out quite capable of killing previously healthy people, not just those with underlying conditions. Overall, however, the pandemic remained what WHO had called it on May 11: “overwhelmingly mild.”
But WHO stopped saying so. WHO wanted countries to prepare for an imminent pandemic of unknown virulence, even as gradually emerging data from developed countries hinted at a low fatality rate so far compared with past pandemics, with very stressful but mostly manageable increased demand on health care systems. Officials seem to have decided that calling the pandemic “mild” risked undermining WHO’s crucial message of preparedness. They couldn’t justify calling it “severe.” So they settled on “moderate.”
The concept of a “moderate pandemic” was a sort-of mixed message, given how terrifying the word “pandemic” had become. In just a couple of years it had made the jump from incomprehensible technical jargon to a scare word, largely courtesy of WHO’s bird flu messaging. So calling something a “moderate pandemic” was a little like calling it a “moderate disaster.” To many people today, even a “moderate” pandemic – like a mid-range Category 3 hurricane – sounds pretty bad.
On June 3, a British newspaper offered this quotation from Keiji Fukuda, then WHO’s senior flu official:
Fukuda appeared to contradict the official view in Britain that the virus was a mild one. “We do have some hesitation in calling such an infection mild,” he said. “It’s probably fair to call the situation something like moderate right now.”
Again on June 9, two days before the pandemic was officially declared, Dr. Fukuda reiterated the point ![]() at a “virtual press conference”: “As I discussed last week, right at this time, we considered the situation and the impact on countries to be relatively moderate.”
at a “virtual press conference”: “As I discussed last week, right at this time, we considered the situation and the impact on countries to be relatively moderate.”
By late summer in the northern hemisphere, and late winter in the southern hemisphere, the first wave of the pandemic could fairly be characterized as follows:
- Emerging data suggested that the first wave had been relatively mild overall in developed countries. These data were still less than definitive, but they were much more solid than in May and June. The first wave really was pretty mild. Worries now centered on a likely second wave, whose severity was unpredictable.
- There were almost no data available to characterize the severity of the pandemic in most developing countries. In countries with poor medical care and virtually no medical surveillance, even a relatively mild pandemic virus might have pretty severe impacts – and even a relatively severe pandemic might go almost unnoticed, hidden by even more severe endemic respiratory diseases.
We think that instead of emphasizing what they actually thought they had learned about the pandemic’s mildness in developed countries, and also emphasizing their uncertainty about what might happen next and what might be going on in developing countries, WHO officials “averaged” the two. They averaged the known and the unknown, what they saw and what they feared – and decided to keep calling the pandemic “moderate.”
But we may be wrong. Some good sources tell us that even today certain top WHO influenza officials genuinely do not judge the early waves of H1N1 to have been mild, despite having labeled as “mild” the first waves of the previous three pandemics.
Months later, in a November 9, 2009, virtual press conference, Dr. Fukuda explained WHO’s continued resistance ![]() to saying it was a mild pandemic so far:
to saying it was a mild pandemic so far:
Now, this fact that most people recover from the illness has led some people to speculate that this is really a very mild situation and really [to] dismiss the pandemic infection but at WHO we remain quite concerned about the patterns that we are seeing, particularly again, because a sizeable number of people do develop serious complications and death and again we are seeing most of these occur in people who are younger than 65 years – a picture which is different from seasonal influenza.
As late as mid-January 2010, as the pandemic waves in northern hemisphere countries were receding, and after a full southern hemisphere pandemic flu season, Director-General Chan was still describing the pandemic as “moderate” – even when her goal was to stress how mild it was. At a January 18 meeting of the WHO Executive Board she said: “For me, the best health news of the previous decade is the fact that the long overdue influenza pandemic has been so moderate in its impact.”
“Moderate” had become the new mild. WHO observers – including journalists covering the pandemic – got the clear impression that WHO would never go below “moderate.”
WHO’s resistance to “mild” has been openly attacked by many critics – but not often by influenza experts. (In most cases we don’t know what their private opinions are.) So a May 20, 2010, BBC interview with Dr. Klaus Stöhr is stunning. Dr. Stöhr directed WHO’s global influenza program until 2007, when the big concern was a potentially very severe bird flu pandemic. Here are some Stöhr quotations from Imogen Foulkes’s BBC story:
- “I personally think that moving to Phase 6 that early was, in hindsight, not needed.”
- “In July and August the Australia and New Zealand national influenza centres were indicating the southern hemisphere outbreak was mild. Virologists, myself included, thought well, it’s not so likely that this virus will become more severe.”
- “At the end of August the WHO website was still calling the virus severe. I personally would have thought there could have been more assessments, and more advice to governments.”
Dr. Stöhr is wrong when he says the WHO website called the pandemic “severe.” The term we kept seeing was “moderate” – even if the tone of WHO warnings may sometimes have conveyed a “severe” impression (and at other times, perhaps, a “mild” impression). And not all virologists were ready to stop worrying about the next wave as early as July and August 2009. But we share Dr. Stöhr’s sense that WHO never properly stood down from its justifiably alarming early warnings.
In our judgment, the key pandemic severity message should have been: “It’s mild but….” There were three key buts – so key we will capitalize them: the Three Buts.
- It’s mild so far but that tells us nothing about what another wave (or another pandemic) might be like.
- It’s mild in the developed world but we really don’t know what’s happening in the developing world.
- It’s mild for most healthy people but it’s more dangerous for people with certain pre-existing conditions, and it’s deadlier than the seasonal flu for young and middle-aged people.
WHO consistently communicated our Three Buts. It neglected to communicate what should have come before the Three Buts: “It’s mild….”
WHO officials were undoubtedly worried – and may still be worried – that saying the pandemic was mild (so far; in developed countries; for most people) might lead governments, communities, and individuals to let down their guard prematurely. That was a valid worry. After all, even without WHO certification that the pandemic was “mild,” many countries’ pandemic vaccination efforts failed dismally, as people reached their own conclusions about the pandemic’s mildness so far and shrugged off the possibility of future waves that could be a lot more virulent.
But WHO officials were not nearly worried enough about the other half of the problem: the risk that failing to say the pandemic was mild, when it obviously was, could undermine the credibility of the Three Buts. Why should people pay attention to the health warnings of an organization that doesn’t seem to recognize the single most salient fact about the pandemic so far, its mildness?
Here’s what we think the public needed to hear from WHO:
So far, limited global surveillance shows that this pandemic has been less devastating to the world than past flu pandemics. There’s no way to tell at first how severe a pandemic will be. At the start the watchword is always to hope for the best and prepare for the worst. So far, the H1N1 pandemic as a whole has been much milder than we feared.
Even so, it has taken a worse-than-mild toll on people with certain chronic health problems, and it has endangered young and middle-aged people more than seasonal influenza usually does. Furthermore, we don’t really know how severe the pandemic has been in developing countries with poor medical care and limited medical surveillance.
The biggest concern now: Past pandemics have sometimes become more severe over time. This one could too. We don’t know yet whether the world will face a more severe second or third wave. And the possibility of a new pandemic – perhaps bird flu – is just as credible a threat as it was before the swine flu pandemic started. We strongly urge continued vigilance, precaution-taking, and preparedness.
Most of the time, WHO gave us the second and third paragraphs without the first. It seemed to be denying the first paragraph, denying what almost everybody already knew: that the pandemic was mild. This severely damaged WHO’s credibility – including the credibility of its valid warnings about the Three Buts.
WHO’s loss of credibility is palpable even within WHO itself. While we were working on this article, we wrote to a number of WHO colleagues – not senior flu experts or top policy people, but professionals at the various WHO regional offices whom we felt we knew well enough to ask this question (not for attribution): Did they, or any of their WHO coworkers, or any of the national government officials they worked with, now see the H1N1 pandemic as having been anything but mild? We got back a chorus of no’s, often accompanied by discouraged asides about how out-of-touch top officials at headquarters appeared to be. (We don’t want to overvalue that last point; that is what branches of government agencies and corporations usually say about the Mother Ship.)
The fact that regional WHO personnel view the pandemic as having been mild doesn’t prove it was mild, obviously. It does, however, demonstrate the cost to the World Health Organization of its lonely insistence on the contrary position. It may also demonstrate the failure of WHO headquarters to pay enough attention to the views of its regional personnel.
Explanations and impacts: Why WHO won’t call the pandemic mild, and why that matters
![]() Keep in mind the Three Buts that should have accompanied any statement that the H1N1 pandemic was mild so far:
Keep in mind the Three Buts that should have accompanied any statement that the H1N1 pandemic was mild so far:
- …but that tells us nothing about what another wave (or another pandemic) might be like.
- …but we really don’t know what’s happening in the developing world.
- … but it’s more dangerous for people with certain preexisting conditions, and it’s deadlier than the seasonal flu for young and middle-aged people.
These Three Buts were not valid rationales for failing to say the pandemic was mild so far, though WHO officials may have thought they were. We understand WHO’s concern that acknowledging the pandemic’s mildness might lead people and governments to let down their guard too much and too soon. Our response is that WHO’s failure to acknowledge the pandemic’s mildness (with appropriate emphasis on the Three Buts, of course) had precisely that effect.
It is a fundamental principle of persuasive communication that you cannot convince people of a proposition if you don’t acknowledge what they already know that makes your proposition strike them as invalid. WHO wants to convince governments (in both the developed and the developing world) that the H1N1 pandemic may be more severe than we realize in countries with poor medical care and poor medical surveillance. It wants to convince individuals, especially individuals in high-risk groups, that getting a swine flu shot is still a sensible thing to do in places where there is vaccine available. Above all, it wants to convince the entire world that we must remain on guard against two scary possibilities: that this pandemic could still take a turn for the worse, and that another, more severe pandemic could materialize at any time.
The obvious counterargument that makes these messages unpersuasive to many people (including many local health officials) is the mildness of the pandemic year the developed world has just lived through. Before WHO can persuasively argue that there are still serious risks worth attending to, it must concede this crucial fact. But WHO hasn’t conceded it. It hasn’t seemed to notice it. It seems to have lived through a different year than the rest of us – and that virtually disqualifies WHO from warning us about anything.
WHO has sometimes had two other responses to charges that the pandemic was mild and that it was derelict in refusing to stand down from its early warnings and say so.

“We don’t want to give offense.”
Over the past year, the word “mild” has become anathema in many pandemic circles, on the grounds that the term itself is offensive to those who were severely affected by H1N1 – offensive to those who were hospitalized and to the families of those who died. “Mild? Tell that to little Timmy!” Flu experts in some countries have gotten into hot water when they called the pandemic “mild,” and thus many public health officials have resolved not to use the word at all.
As far as we know, WHO hasn’t offered this rationale explicitly as a reason why it refuses to call the pandemic mild. But WHO spokesperson Gregory Hartl did use the “Tell that to little Timmy!” argument against critics who doubted H1N1 was severe enough to be called a pandemic. “To insinuate that this was not a pandemic,” Hartl said, “is very disrespectful to the people who died from it.” If Hartl thinks it is disrespectful of victims to say H1N1 wasn’t a pandemic, then he would understandably be concerned that it might also be disrespectful of victims to say it was only a mild pandemic.
At a meeting in New Delhi in April 2010, the director of WHO’s Southeast Asia Regional Office, Samlee Plianbangchang, was asked if the “H1N1 scare” had been exaggerated by WHO. According to the Times of India, Dr. Samlee responded, “Yes, it was.” Within hours, WHO issued a retraction in his name, saying, “Any suggestion that the pandemic is an ‘exaggeration’ is to ignore recent history and science, and to trivialise the deaths of over 17,000 people and the many additional serious illnesses experienced by others.”
The notion that calling the swine flu pandemic “mild” disrespects those who have died or that calling it an “exaggeration” trivializes their deaths is quite a strange notion for public health officials. Everyone in public health knows full well that not every infectious disease death constitutes an outbreak, not every outbreak constitutes an epidemic, and not every epidemic constitutes a pandemic – or a “public health emergency of international concern.” Those who died of flu during the H1N1 pandemic had a very severe case of influenza. But every flu season, many people die of a very severe case of influenza – and no one is accused of disrespect or trivialization when they state that a given flu season has been mild, or below a country’s epidemic baseline.
It does not disrespect or trivialize individual deaths to notice whether the total number of deaths has been large or small.
No doubt some people find death more meaningful when it’s part of something important, widespread, and newsworthy. We can’t remember anyone ever mentioning that her great-grandmother died in the seasonal flu outbreak of 1917.
But that natural feeling has nothing to do with deciding how severe the world’s H1N1 experience has actually been. Every illness, every hospitalization, and every death is important to those it affects directly. This is the fundamental difference in perspective between medicine and public health.
The unit of analysis for medicine is the patient. The medical question is: How severe is this for the patient? But the units of analysis for public health are the community, the country, the region, and the world. The main public health questions are: How many people is this disease affecting, and how severely? What are the knock-on public health effects of so many people being sick from this disease at the same time? How is this disease spreading, and what may happen next in this community, this country, this region, and the world?
Every death may be a tragedy, but every death is not a public health emergency of international concern.
The above quotations from WHO spokespeople notwithstanding, the World Health Organization understands the difference between the medical perspective and the public health perspective. WHO routinely helps local and national health officials cope with infectious disease outbreaks and epidemics without calling them all “moderate” or “severe.”
In June 2010, the communicable disease bulletin of another WHO region, the Eastern Mediterranean Region, published a short article
 under the headline “Pandemic (H1N1): No room for complacency!” It noted that the current pandemic “appears relatively mild, certainly much milder than previous pandemics.” This recent statement (last accessed June 23, 2010) has not yet been retracted.
under the headline “Pandemic (H1N1): No room for complacency!” It noted that the current pandemic “appears relatively mild, certainly much milder than previous pandemics.” This recent statement (last accessed June 23, 2010) has not yet been retracted.
-
“It’s enough to point out that most cases are mild.”
After refusing to call any of the first year’s worth of pandemic waves “mild,” WHO now faces the bizarre accusation that it intentionally hyped a “fake pandemic.” It has defended itself, in part, by leaning on the fact that it has repeatedly said that most swine flu cases were mild.
In its response to the first wave of “fake pandemic” criticism, WHO pointed out:
WHO has consistently assessed the impact of the current influenza pandemic as moderate. WHO has consistently reminded the medical community, public, and media that the overwhelming majority of patients experience mild influenza-like illness and recover fully within a week, even without any form of medical treatment. WHO has consistently advised against any restrictions on travel or trade. Although influenza viruses are notoriously unpredictable, it is hoped that this moderate impact will continue throughout the duration of the pandemic.
A moderate flu pandemic, in other words, is one in which most people have mild symptoms.
But most people have had mild symptoms and recovered without any medical treatment in all influenza pandemics so far – mild ones, moderate ones, and severe ones. A mild flu pandemic isn’t a pandemic in which most cases are mild. A mild flu pandemic is a pandemic in which the number of deaths and the degree of social disruption are both on the low end of the spectrum, compared to other flu pandemics in recorded history. Swine flu meets that criterion so far. But WHO hasn’t said so. Merely saying that most cases are mild doesn’t mitigate the credibility problem caused by WHO’s refusal to say so.
And look again at the end of this quotation: “…it is hoped that this moderate impact will continue throughout the duration of the pandemic.” Why on earth would WHO hope that a pandemic would continue to have a moderate impact, rather than hoping the pandemic would become mild?
Similarly, in her June 8, 2010 letter responding to conflict-of-interest allegations in BMJ, WHO Director-General Chan wrote:
The implication that WHO provoked unjustified fear also needs to be addressed. The record is otherwise, and not a matter of interpretation. On 11 June 2009, when I announced the start of the pandemic, I drew attention to the fact that the worldwide number of deaths was small, and clearly stated that we did not expect to see a sudden and dramatic jump in the number of severe or fatal infections. In every assessment of the pandemic, WHO consistently reminded the public that the overwhelming majority of patients experienced mild symptoms and made a rapid and full recovery, even without medical treatment.
This is a perplexing statement. Dr. Chan’s first claim is misleading. For good reasons, WHO wanted to be clear on June 11 that its Phase 6 declaration did not mean it expected an abrupt increase in the number of severe or fatal infections as of June 12. But as H1N1 continued to spread in the months that followed, WHO did expect – and the world did experience – “a dramatic jump in the number of severe or fatal infections.”
Dr. Chan’s second claim, that WHO always said most cases were mild, is true but disingenuous. Yes, WHO has frequently pointed out that most swine flu patients recover quickly. This was also true during the mother of all flu pandemics, the horrendous pandemic of 1918. Even then, the overwhelming majority of patients made “a rapid and full recovery, even without medical treatment.” One authoritative source points out: “Despite the extraordinary number of global deaths, most influenza cases in 1918 (>95% in most locales in industrialized nations) were mild and essentially indistinguishable from influenza cases today.” As Dr. Chan knows full well, a pandemic that killed, say, 2.5% of its victims (as the 1918 pandemic did) would be a stunningly severe pandemic, orders of magnitude worse than the swine flu pandemic has been so far – even though 97.5% of its victims recovered.
We suspect three interrelated conscious or unconscious motivations may help account for WHO’s reluctance to label the pandemic as mild. All three are extremely common motivations, but are seldom acknowledged.

Nobody likes having to revise their messaging.
The bias against revised messaging is common not just in risk communication but in communication, period. Our clients don’t like having to change their tune. They want to figure out what their messages ought to be, craft them, and then stick to them.
It’s not mostly that revising your messaging takes effort. The main source of the resistance seems to be a fear of looking inconsistent and incompetent. Again and again, we have come up against this fear when we urge clients to switch from one message to another. “But we have been saying X for weeks already. If we switch now to Y, won’t people think we don’t know what we’re doing?”
Consistent messaging is a virtue – if your messages were right in the first place, and if both the situation and your understanding of the situation have remained constant. In crisis communication the second criterion is never met. Whether it’s an oil spill or a pandemic, the situation always keeps changing, and you always keep learning new things about it. Endlessly revised messaging goes with the territory.
In the case of pandemic severity, WHO’s early messaging was appropriately alarming. Any emerging influenza pandemic is potentially disastrous until proven otherwise; the core tasks of a public health agency at the start of such an event are to sound the alarm and organize the response. The specter of bird flu – an extraordinarily deadly virus that kept threatening to go pandemic – was in the back of every expert’s mind. And the early news from Mexico suggested that this new flu virus might have an alarmingly high death rate of its own. Then the news improved. More information came in from Mexico, suggesting that a lot of mild cases had gone unreported; this meant that H1N1 in Mexico was apparently much more prevalent but much less virulent than first believed. Early U.S. data led to the same tentative conclusion that H1N1 was proving mild, as did the early experience of most other countries in which the virus had begun to spread.
That’s when WHO’s “severity messaging” should have changed, and didn’t.
WHO had no problem revising its technical messaging as the pandemic waxed and waned. Its frequent situation updates routinely communicated changing conditions – for example, changing levels of influenza activity in various parts of the world. But WHO’s messages aimed at the public at large were far less responsive to changing conditions … most critically, changing assessments of the pandemic’s severity.

Nobody likes having to express uncertainty.
Part of what makes our clients fear that they’ll look inconsistent and incompetent if they change their messaging is this: Their messaging tends to be overconfident in the first place.
You earn the ability to convince people that the situation has changed (when it has) by having told them, early and often, that it was very likely to change. You earn the ability to convince people that your understanding of the situation has changed (when it has) by having told them, early and often, that your current understanding was very tentative.
WHO did try to express uncertainty and tentativeness early on. But its efforts to do so often failed. And when better evidence came in about the real-time situation in many countries, WHO’s later messages didn’t change enough to match the new data.
The June 3 BMJ conflict-of-interest article addresses this point explicitly:
Another factor that has fuelled the conspiracy theories is the manner in which risk has been communicated. No one disputes the difficulty of communicating an uncertain situation or the concept of risk in a pandemic situation. But one world expert in risk communication, Gerd Gigerenzer, director of the Centre for Adaptive Behaviour and Cognition at the Max Planck Institute in Germany, told the BMJ/The Bureau: “The problem is not so much that communicating uncertainty is difficult, but that uncertainty was not communicated. There was no scientific basis for the WHO’s estimate of 2 billion for likely H1N1 cases….”
The “two billion likely cases” example is a good one. There’s nothing mysterious about where this number comes from. The conventional and oft-repeated guesstimate is that flu pandemics tend to infect roughly 25–35 percent of the world population before they’re over. The world population is currently around 6.8 billion. So if you know absolutely nothing about a brand-new pandemic and are asked to guess how many people it will infect, 25–35% of 6.8 billion (1.7 to 2.4 billion people) is your best guess, and two billion is the right round number to use.
The actual number of swine flu cases so far is still highly uncertain. But we know more than we knew at the start, given sero-conversion data from a few countries. So maybe two billion is no longer the best guess at the number of swine flu cases worldwide. But it was the best guess when the pandemic began.
What’s clear is that most people who heard the “two billion” number in the early weeks of the pandemic, and experienced it as a very scary number, never understood that it was just a guess – albeit a guess based on past pandemics. Gerd Gigerenzer seems to have thought “two billion” was an arbitrary number drawn out of thin air to frighten the masses. And he obviously wasn’t alone; many people thought the number was WHO scare-mongering. Many others probably thought “two billion” was a scientific prediction based on carefully compiled data. Actually, it was neither. It was a best guess based purely on historical precedent, not on knowledge about the likely course of this particular pandemic.
Though WHO was willing to guess about the future incidence of what was to become the H1N1 pandemic, it wisely refused to guess about how severe the pandemic was likely to turn out. But WHO’s obvious (and justified) sense of urgency sent its own severity message. WHO and flu experts all over the world had bird flu on the brain. They composed uncertainty lyrics, but they sang those lyrics to a very alarming tune. The meta-message, the message underlying WHO messaging, seemed to be: “We don’t know what’s going to happen, but it’s probably going to be bad.”
WHO officials kept singing that alarming tune long after the swine flu pandemic appeared rather mild to normal people who didn’t know anyone who had died or almost died. WHO officials were still feeling alarmed, and still feeling uncertain, mostly because they realized that a mild first wave didn’t guarantee that a second or third wave would also be mild.
The right severity message by late summer 2009 would have been a mix of two messages: a fairly confident reassuring message about the present and a highly uncertain alarming message about the future. “As far as we can tell, it has been a mild pandemic so far. But that tells us nothing about the possibility of a much more severe second or third wave.”
Because it failed to validate the real-time apparent mildness of the pandemic, WHO wasn’t able to credibly and persuasively warn about the uncertain but scary potential future, a potential future that still justified intense, expensive, and upsetting preparedness efforts.
Thus WHO miscommunicated uncertainty on both sides of the coin: It refused to sound increasingly certain about what appeared to be happening so far (a mildish pandemic, at least in the developed world), and it refused to sound vividly and alarmingly uncertain about what might happen next (a mutated H1N1 that could cause vastly more morbidity and mortality).
Despite Gerd Gigerenzer’s comment in the BMJ article, communicating uncertainty is extremely difficult. It’s psychologically difficult: When talking to the media, experts are powerfully tempted to oversimplify in the direction of less uncertainty. And it’s organizationally difficult: Organizations dislike sounding like they don’t know the answers.
Even when officials are really trying to communicate their uncertainty, it’s still hard to get through journalists’ preference for definitive information. Reporters routinely turn nuanced statements into black-and-white paraphrases, and then headline writers dial down the uncertainty even more. Journalists consider what their sources don’t know a lot less newsworthy than what their sources know. And they think their sources know more, not less, than they claim, downplaying experts’ warnings that “we’re not sure yet” as pro forma. It is very difficult to get uncertainty-nuanced warnings into news stories, and extremely difficult to get them into news stories repeatedly. Yet a steady drumbeat of uncertainty is what it takes to get the uncertainty message across to the public.
Let’s go back to Gigerenzer’s example: two billion likely cases. Before swine flu was officially declared a pandemic, WHO’s Keiji Fukuda pointed out that “Perhaps a third of the world’s population could be infected with this virus.” He cautioned reporters that the number was based on past pandemics, stating explicitly: “I do not want you to walk out of here saying that there is an estimate that 2 billion will get infected in the next year or so…. Please do not interpret this as a prediction for the future.”
This is exactly what we would have recommended.
The next day’s headline: “2 Billion Infected? WHO Stokes Swine Flu Fear.” And that was the headline over an article that actually included Dr. Fukuda’s warning not to interpret the “two billion” as a prediction. Most of the news coverage headlined the “two billion” and scrapped the warning. Thus:
- “In 2 years, 2 billion will get swine flu: WHO” (Times of India)
- “WHO maintains 2 billion estimate for likely H1N1 cases” (Reuters)
The best way we know to address this problem is to keep “going meta” at press briefings any time previous coverage has been misleading or inaccurate. “Yesterday I tried to convey my uncertainty about how bad this might get, and the resulting stories quoted only the alarming half of my statement. I must not have been clear enough. I’ll try again today to convey both sides of what might happen, and I hope tomorrow’s stories get them both.”

Nobody likes looking like they caved in to pressure.
One of the core principles of outrage management is that outrage is almost always symmetrical. When other people are outraged at you, the odds are overwhelming that you are also outraged at them – for criticizing you unfairly, for publicizing your mistakes, for undermining your credibility, etc. It is the symmetry of outrage that makes it so hard to manage: Outraged people aren’t very skillful at responding to their critics’ outrage. Instead of admitting that their critics are right about some things, outraged people tend to get defensive and dig in their heels.
We see this with our clients all the time. They ought to admit that there are kernels of truth among the overbroad, mostly false claims of their critics. But they don’t admit anything. The critics keep repeating the same broad accusations that contain kernels of truth, and our clients keep denying the whole package. Over time, more and more people notice that some of the accusations are true or partly true, and start to wonder if the whole package is true.
Now three barriers come into play:
- Inside the organization, it’s not a good career move to recommend acknowledging that the critics are partly right. It makes your coworkers question whose side you’re on.
- Even if somebody makes the recommendation, the organization is bound to resist. “Not under pressure. No way. We’ll look like we’re caving in. It’ll feel like we’re caving in. Maybe later, when nobody’s attacking us anymore, we can quietly admit a few things.”
- And if the organization does decide to go ahead and “admit a few things” now, it’s almost sure to pretend the decision had nothing to do with pressure from its critics. “We’re updating based on new data.” Or: “The revised approach has been in the works for months.” Or: “We’re just clarifying a misunderstanding the media got wrong.” So: no apology, no acknowledgment, no credit.
We think WHO missed its moment. It should have starting modulating its pandemic warnings in July or August of 2009. But for all the reasons we have discussed, and maybe some more we don’t know about, WHO didn’t modulate its message. It was afraid people would let down their guard; it was worried the pandemic would take a turn for the worse and it would be blamed for encouraging people to let down their guard; it wanted to wait till the data were clearer; it didn’t want to give offense to those who had been hardest hit … etc. More and more local and national officials, influenza experts, journalists, and ordinary citizens noticed that the pandemic had been mild so far. But WHO didn’t say so.
Then, in late 2009, the “fake pandemic” criticism started – a false, unfair attack grounded in some genuine WHO risk communication errors. Humanly but unwisely, WHO got defensive, and it stonewalled.
Understandably resentful of the fake pandemic allegation, WHO (and its supporters) have found themselves steadfastly insisting that the pandemic isn’t mild. The issue is thoroughly polarized: “the pandemic is fake” versus “the pandemic is serious” (moderate or worse). It’s hard to find anyone willing to take the sensible position that the pandemic is both (a) real and (b) really pretty mild.
Imagine if WHO had managed not to stonewall. Imagine if WHO had responded to its critics this way instead:
It’s not true that we hyped the pandemic because we wanted to see Big Pharma make big profits. But it is true that we have never properly stressed what millions of people were learning on their own – that the pandemic has been mild so far, at least in the developed world. By the standards we use to judge pandemics, the standards that led us to call the 1968 pandemic “mild,” this pandemic is also mild.
We were very worried at the start. And we’re still worried about what the future will bring; the next wave (or the next pandemic) might tell a very different story. And of course even a mild pandemic causes significant mortality and morbidity, as well as health care system impacts.
But we never properly stood down from our early warnings. We never properly acknowledged that the pandemic was turning out mild so far, so mild that some people weren’t even sure it ought to be called a pandemic at all.
Once our initial fears about Mexico had subsided, our failure to modulate our warnings frightened some people unnecessarily about the current situation. It undermined the credibility of our warnings about the future. And it gave credence to the inaccurate charge that we had declared a fake pandemic in order to enrich the pharmaceutical industry.
It’s not too late for WHO to say exactly that, with the additional admission that the time lag has been unconscionably long. Coming clean in this way won’t be a panacea. But it will help begin to clear the air.
Why do we think WHO’s failure to call the H1N1 pandemic mild is such an important mistake? Because it has undermined both WHO’s credibility as an organization and the credibility of WHO’s pandemic warnings.
No warning system can work if it moves only in one direction, if it ratchets up when there are grounds for immediate alarm and gets stuck there, unable to drop down again when those grounds abate, for the moment at least. Consider for example how children respond to an over-protective parent, who seems to think everything is dangerous. Such a parent’s warnings soon lose any meaning.
The same is true in the other direction. Right now, BP is widely and justifiably seen as having understated the severity of its oil spill in the Gulf of Mexico. Suppose BP were to find evidence that less oil was leaking than previously believed, or that the spill’s impact on marine ecosystems was less than had been feared. BP would lack the credibility to drive home these important new findings. It would be completely unable to persuade most people to worry less, precisely because it had failed to tell them to worry sufficiently in the first place.
In exactly the same way, and for exactly the same reasons, WHO cannot credibly tell people that the H1N1 pandemic might still get worse – when it appears to be the only organization left that believes it is “worse” now (except perhaps for India’s Ministry of Health). Nor can WHO credibly warn that the world needs to undertake strenuous and expensive preparations for the possibility of a really bad pandemic in the future – when it appears to believe that what the world has been experiencing since April 2009 is already a pretty bad (“moderate”) pandemic.
Over the long term, the ability of officials to issue credible public health warnings depends on their ability to stand down from those warnings when the risk is found to be lower than initially feared, or when the risk is mostly gone (even if it may return – which is something else they can’t credibly warn about when they’re not yet saying it’s mostly gone for now).
It is as if hurricane forecasters were unwilling to say so when a hurricane veered off its likeliest course or decayed into a much milder storm.
Alarming and reassuring communications about evolving situations, in short, are fundamentally about change in the context of uncertainty: how you think the situation has changed since yesterday, and how you think the situation may change tomorrow. You can’t credibly tell people that it looks like things have improved unless you have demonstrated your ability and willingness to tell them when things looked really bad. And vice-versa: You can’t credibly tell people that you’re worried things might get a lot worse unless you have demonstrated your ability and willingness to tell them when things didn’t look so bad.
With regard to WHO’s perpetually “moderate” pandemic, a health journalist we know put it this way: “WHO seems to be reporting from another planet.”
None of this is new. This site’s Swine Flu Pandemic Communication Update for May 6, 2009 – very, very early in the course of the pandemic – began: “At the moment, the H1N1 swine flu is still spreading around the world, but s-l-o-w-l-y, not explosively. And the new cases are usually mild….” A reader criticized the update for over-optimism. Peter responded in the website Guestbook as follows:
Here’s the core communication issue.
In the early days of the swine flu outbreak, the authorities were right to sound the alarm, and people were right to become alarmed. In fact, too many people didn’t become alarmed enough – and very few did much actual preparing.
But then the situation changed. Later information suggested that the short-term prognosis was much better than it had initially looked, both because the virus was turning out less deadly than we feared, and because it was spreading less quickly than we feared.
A lot of people reacted to this new information by deciding that they had been gulled by official fear-mongers. So they felt foolish and irritated … and in no mood to take heed of the possibility that things could get worse again.
Somehow, three key messages need to get communicated to an audience that isn’t in a mood to hear them:
- Things looked bad for a while. You were right to worry (and we were right to warn you).
- Things look better now. In most places, your chances of catching swine flu today are very slim, and few if any immediate precautions are called for. You are right to worry less about the current situation. (And we can understand why some of you may feel we should have kept our earlier warnings to ourselves till we were surer.)
- Things could easily get worse again. You would be right to remain vigilant, and to use this apparent “slow period” to prepare in case things do get worse. (And we know it may be hard to gear up in response to yet another warning.)
These messages will be very difficult to sell. I don’t think we can get anywhere at all with the first and the third unless we pay sufficient attention to the second. Yes, things looked bad. Yes, we’re not out of the woods. And yes, so far the news is better than expected.
This messaging advice might have helped WHO when it was written on May 10, 2009. It might still help WHO today, accompanied by repeated apologies for having failed to “stand down” sooner.
The mistake repeated: WHO’s failure to categorize the pandemic as “post-peak”
![]() The eighth and most recent meeting (via teleconference) of the Emergency Committee that advises WHO on pandemic management took place on June 1, 2010. There are no public transcripts of Emergency Committee meetings, but on June 3 Director-General Chan issued a statement summarizing and affirming what she said were the unanimous results of the meeting:
The eighth and most recent meeting (via teleconference) of the Emergency Committee that advises WHO on pandemic management took place on June 1, 2010. There are no public transcripts of Emergency Committee meetings, but on June 3 Director-General Chan issued a statement summarizing and affirming what she said were the unanimous results of the meeting:
After extensive discussions and questions, the Committee expressed the unanimous view that from a global perspective while pandemic activity is continuing, the period of most intense pandemic activity appears likely to have passed for many parts of the world. Committee members stressed that it remains critical for countries to continue to maintain vigilance concerning the pandemic, including all necessary public health measures for disease control as well as influenza virus and disease surveillance.
The Emergency Committee and the Director-General wisely didn’t say the pandemic is over. Ends of pandemics are hard to define, since the pandemic virus usually (or maybe always) turns into a seasonal virus. Past pandemic viruses that experts know about haven’t suddenly disappeared to mark the end of the pandemic; they just gradually stopped producing cases and deaths significantly above pre-pandemic levels. But the pandemic H1N1 virus is not yet obviously seasonal, so another pandemic wave is possible. A more virulent wave is also possible, though experts consider it much less likely after this much time. Likeliest of all is that H1N1 is already on its way to becoming a new strain of seasonal influenza. But that’s not yet certain or even close to certain, so declaring the pandemic over would be premature.
What is harder to understand – in fact, incomprehensible – is why the Emergency Committee and WHO didn’t declare the pandemic to be past its peak by early June 2010.
The “post-peak period” is defined in WHO’s April 2009 revised pandemic phases ![]() as follows:
as follows:
Levels of pandemic influenza in most countries with adequate surveillance have dropped below peak levels. The post-peak period signifies that pandemic activity appears to be decreasing; however, it is uncertain if additional waves will occur and countries will need to be prepared for a second wave.
That sounds a lot like Dr. Chan’s own description of what is happening as of June 2010, though she used more than the usual number of qualifying phrases: “…the period of most intense pandemic activity appears likely to have passed for many parts of the world.”
In the revised phases, “post-peak” comes after Phase 6, a full-fledged pandemic. There are two more phases after “post-peak”: “possible new wave” if surveillance shows flu levels rising again above seasonal levels, and “post-pandemic period” when the levels “have returned to the levels seen for seasonal influenza in most countries with adequate surveillance.”
All over the developed world, it looks to public health officials and ordinary people like the pandemic peaked in their countries ages ago, and isn’t dramatically surging upwards again so far, even in the southern hemisphere where flu season has already begun. Yet there sit WHO and its Emergency Committee, still sticking with Phase 6.
So again, it looks like WHO is being unduly alarming about the current pandemic situation, while normal people all over the world have noticed that the amount of influenza around is low. The potential exists for more pandemic waves of H1N1 in the future, just as the potential has always existed for H1N1 to turn more virulent in the future. But as with the mild-versus-moderate first and second waves, WHO is labeling the current pandemic situation in a way that is higher on the “seriousness” scale than appears to be the case.
The world’s current situation appears to be exactly the situation for which the “post-peak” category was created: Levels are down but officials aren’t convinced there won’t be another wave. It is likely that when they added the “post-peak” phase, WHO officials were thinking of a moment just like this. The definition of the post-peak phase even has a built-in defense against over-optimism and premature relaxation: It includes the warning to stay prepared for possible additional waves.
So why didn’t WHO jump at the chance to declare H1N1 post-peak in early June 2010? We can only guess at the answer: When WHO officials created the post-peak phase, they weren’t imagining that they would be feeling so embattled when the moment came – that acknowledging “post-peak” would feel more like caving in to their enemies than like tracking an important moment in the life cycle of the pandemic.
Dr. Chan’s statement says the Emergency Committee was unanimous that the pandemic is not yet post-peak. Like the decision itself, the committee’s unanimity is a little hard to understand. Many top influenza experts have publicly opined that the pandemic’s peak has passed. So why did the committee vote unanimously to the contrary? Did the committee have information not available to outside experts? We doubt that. Is the committee wildly unrepresentative of the range of expert opinion? That would be surprising too. Did the committee give in to subtle (or not so subtle) arm-twisting from WHO officials? That’s the least unimaginable of the hypotheses we can think of; like many U.N. organizations, WHO prefers consensus decisions over majority votes.
Or perhaps the committee wasn’t actually unanimous that the peak isn’t over. Dr. Chan’s statement certainly doesn’t affirm that the pandemic is now in the post-peak stage, but it doesn’t explicitly deny it either. It just says “the period of most intense pandemic activity appears likely to have passed for many parts of the world,” and promises the Emergency Committee will meet again in mid-July. It’s almost as if the “post-peak phase” definition/description didn’t exist – which it didn’t until the new April 2009 guidance document ![]() was published.
was published.
That April 2009 guidance document is hotly controversial for other reasons entirely. It was in that document – published just as H1N1 was beginning to spread – that WHO inaugurated new definitions and descriptions of the pandemic phases that de-emphasized severity, leading later to charges that WHO had changed its definition of a pandemic in order to make sure H1N1 would qualify. (We will turn to these charges in the next section.) But if WHO has decided to abandon the April 2009 version of the pandemic phases, it hasn’t said so, and it hasn’t proposed a replacement. And under the April 2009 document, it looks to all the world – except the World Health Organization itself – like the H1N1 pandemic of 2009–10 is now in the post-peak phase, according to the WHO’s own definition of that phase.
Though Director-General Chan’s June 3 statement may be a little ambiguous about whether we’re still in Phase 6 or have progressed to the post-peak phase, the WHO website leaves no doubt. The page to check is entitled “Current WHO phase of pandemic alert.” Here’s what it looks like as of June 22, 2010:
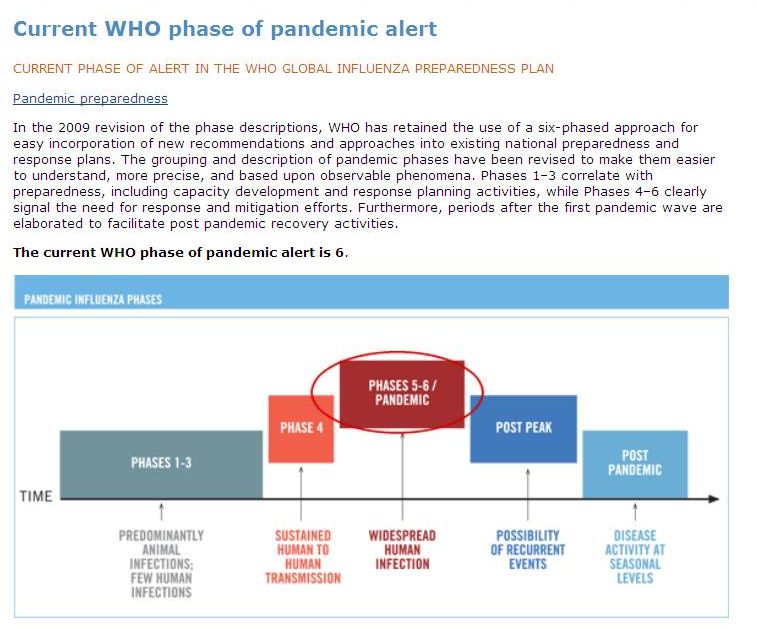
We are not influenza experts. WHO and its Emergency Committee are chock-full of influenza experts. If they truly perceive the pandemic as “moderate” compared with pandemics previously assessed as “mild,” and if they truly perceive the pandemic as still being in Phase 6 rather than post-peak, then of course that’s what they have to tell the world. But the communication challenges in that case are as difficult as any we can imagine, because WHO’s perception doesn’t match the reality that most people have experienced.
WHO’s Failure to Acknowledge that It Changed Some Flu Pandemic Definitions and Descriptions Just as H1N1 Was Emerging
Column Table of Contents
WHO’s Failure to Acknowledge the Ongoing Mildness and Current Low Incidence of the Pandemic
Evidence that the swine flu pandemic has been mild so far
WHO’s unwillingness to call the pandemic mild
Explanations and impacts: Why WHO won’t call the pandemic mild, and why that matters
The mistake repeated: WHO’s failure to categorize the pandemic as “post-peak”
About definitions and redefinitions
How and why WHO changed its use of the term “influenza pandemic”
Mishandling the definitional controversy
![]() Here’s all you really need to know about what should have been a tempest-in-a-teapot, if not for WHO’s stonewalling:
Here’s all you really need to know about what should have been a tempest-in-a-teapot, if not for WHO’s stonewalling:
- WHO’s critics have endlessly charged that just as swine flu was starting to spread, WHO “changed the definition of a pandemic” in a way that omitted severity, thus making sure that swine flu would qualify as a pandemic regardless of its mildness. This was done, the critics say, to cause national governments to buy lots of vaccine and antiviral drugs, swelling the profits of Big Pharma.
- WHO did not change the generic definition of the word “pandemic.” But past definitions of the term “influenza pandemic” have been inconsistent with regard to many factors, including the role of severity and whether a very mild pandemic should still be called a pandemic. WHO usage has been inconsistent too, but WHO certainly didn’t mastermind a sudden, profit-motivated change in the definition of “pandemic” or of “influenza pandemic.”
- What did WHO do that generated these charges? Right after the novel H1N1 virus was identified, WHO published revised definitions and descriptions of the phases of influenza pandemics. These revisions incorporated many changes, including the elimination of five references to “severity of illness” as a factor that “may be considered” in deciding when to ratchet up from one pandemic phase to the next. Since influenza pandemics can have mild first waves and severe later waves, this seemed like a sensible change.
- Although these revisions had been in the works for years, WHO decided to publish the revised guidance document urgently when it looked like a new pandemic was about to burst on the scene.
- Whether it was wise of WHO to de-emphasize severity in its new flu pandemic phase definitions is legitimately debatable. So is whether it would make sense to set a minimum level of severity required to justify using the word “pandemic” about a novel flu virus. But there is no evidence whatever that WHO made the changes it made in order to enrich Big Pharma.
- WHO’s critics have been linguistically careless about the distinction between “changing the definition of a [generic] pandemic” and “changing the definitions and descriptions of influenza pandemics and influenza pandemic phases.” They accuse WHO of doing the former (false) and then cite evidence that WHO did the latter (true).
- WHO has been legalistic and disingenuous about this same distinction. Instead of candidly acknowledging what it changed in its definition and description of influenza pandemics, and then explaining why, WHO has categorically denied, again and again, that it ever changed the definition of a [generic] pandemic. And it has accurately but irrelevantly insisted, again and again, that severity was never part of the definition of a [generic] pandemic.
- In the “definition of a pandemic” imbroglio, the damage to WHO’s credibility did not result from its decision to redefine the flu pandemic stages in a way that eliminated references to severity. WHO’s damaged credibility resulted from its decision to take advantage of the confusion between generic pandemics and influenza pandemics. “We never changed the definition of…” and “Severity was never part of the definition of…” are true about generic pandemics and false about influenza pandemics. WHO told legalistic, intentionally misleading truths that made it look like a liar.
That’s it, really. Feel free to skip to the next section if you wish.
But if you decide to read on, try to keep in mind the distinction between “the definition of a [generic] pandemic” and “definitions and descriptions of influenza pandemics and influenza pandemic phases.” WHO’s critics have failed to grasp this distinction. WHO officials have pretended not to grasp it. So they have had a gloriously irrelevant dispute over whether WHO changed the definition of a pandemic (it didn’t), instead of a potentially useful discussion about why WHO did change its definitions of the flu pandemic phases and its definitions/descriptions of flu pandemics in a way that de-emphasized the importance of severity.
About definitions and redefinitions
![]() All definitions are stipulative. Words don’t come with their meanings stenciled on their foreheads. We forge their meanings by how we use them. That’s not to say that we’re in an Alice-in-Wonderland world. From Through the Looking Glass:
All definitions are stipulative. Words don’t come with their meanings stenciled on their foreheads. We forge their meanings by how we use them. That’s not to say that we’re in an Alice-in-Wonderland world. From Through the Looking Glass:
“When I use a word,” Humpty Dumpty said, in a rather scornful tone, “it means just what I choose it to mean – neither more nor less.”
“The question is,” said Alice, “whether you can make words mean so many different things.”
“The question is,” said Humpty Dumpty, “which is to be master – that’s all.”
WHO cannot decree that the word “pandemic” (or the term “flu pandemic”) means just what it chooses. Definitions are negotiated agreements … and sometimes the negotiations break down.
It is always dangerous to use a word in a way you know your audience is likely to misperceive. One of us (Peter) wrote a column on this topic in 2005, entitled “Risk Words You Can’t Use.” If he were revising that column today, “pandemic” might end up on the list. But we really need the word “pandemic.” That’s why we have to negotiate what it means, not just stop using it.
Sometimes you redefine a word – use it differently than your audience uses it – in order to point out something important about other people’s mental models. That’s what the “Risk = Hazard + Outrage” formula tries to do. It redefines “risk” in an effort to persuade people to change how they see the risk communication task. But any time you do that, you know before you start that you’ll need to allocate a lot of time and effort to troubleshooting: “People understandably think I mean X when I say that, but I don’t. I mean Y. Let me tell you why I’m using the term in such an unexpected way….”
It may have been a mistake for WHO to take on the extra burden of changing its definitions and descriptions of pandemic phases just as novel H1N1 appeared. It was certainly a mistake for WHO to take on this extra burden without taking it seriously as a potential risk communication problem.
And as skepticism and suspicion emerged and then grew, it was a mistake for WHO to avoid conceding (and appear to be denying) the particular changes that had become most salient to the skeptics, and then to a broader audience: the changes in WHO’s definitions of the pandemic phases, and the changes in WHO’s most prominent definition/description of an influenza pandemic.
If the swine flu pandemic had been more severe, the changes in WHO’s pandemic phase definitions wouldn’t have mattered much. And the absence of a severity criterion in WHO’s definition/description of an influenza pandemic would have made no difference at all. But once the moderate/mild mismatch arose between WHO’s portrayal of the pandemic and the public’s view of it, the need to acknowledge and explain the redefined flu pandemic phases and the revised definition/description of an influenza pandemic became urgent. Yet WHO chose not to provide the needed acknowledgments and explanations.
For years, the word “pandemic” and the phrase “flu pandemic” meant absolutely nothing to most people. These were terms of art, used almost exclusively by experts. In much of the world, even the word “influenza” still doesn’t ring a bell, while the word “flu” often refers to any mild respiratory infection, and sometimes even non-respiratory ones.
Experts, meanwhile, have often used “pandemic” and “flu pandemic” rather loosely.
In the professional literature, there are varying definitions of influenza pandemics. Pretty much all the definitions specify that a flu pandemic is a widespread outbreak of a novel flu virus subtype that does significant health harm to humans. But how widespread, how novel, and how much harm are sometimes specified in discrepant ways, and often not specified at all. With regard to novelty, for example, some definitions state that a population must have “no” immunity, while others state that there must be “little immunity.” Some definitions say categorically that a “new subtype” of influenza is required, implying that a reassorted, antigenically shifted virus of the same subtype as one that is currently circulating cannot be considered “novel” enough to cause a pandemic, nor can one that re-emerges from a laboratory freezer decades after it last circulated. Other definitions stipulate that a subtype can be considered “novel” enough even with the same H and N as a currently or previously circulating flu virus.
Moreover, there is a huge professional literature that describes flu pandemics in ways that often go beyond the specifications in formal definitions. The boundary between definitions and descriptions isn’t a bright line. This unclear boundary has figured periodically in the controversy over what exactly WHO did just as the novel H1N1 virus was beginning to spread. Leave aside the poorly framed charge that WHO changed the definition of a pandemic. Did it change the definition of a flu pandemic? Or did it merely publish yet another description of what flu pandemics are like? Do new definitions of the phases of flu pandemics constitute, collectively, a new definition of a flu pandemic – or do they just describe it differently?
This much is indisputable: WHO did change the role of severity in its definitions and descriptions of the phases of an influenza pandemic. It is those phase definitions and descriptions that ultimately determine whether and when WHO declares that an influenza pandemic has begun. Whether or not WHO redefined the term “flu pandemic,” it did rejigger the criteria for declaring a flu pandemic. In particular, it took severity off the list of potential criteria.
Over the years, how has severity figured in the various definitions and descriptions of influenza pandemics? For one thing, it has often played a crucial role when a flu pandemic seems to be winding down. The end of a flu pandemic has often been defined/described as the point when it is clear that the influenza death rate has come back down to “normal flu season” levels. This strongly suggests that a flu pandemic has to be deadlier than the average seasonal flu. But we haven’t found any formal definitions that specify that a flu pandemic must be deadlier than the average seasonal flu, nor have we found any that specifically claim a flu pandemic can be milder than the average seasonal flu. Some definitions or descriptions are explicit that a flu pandemic must cause excess mortality in at least some age group. Others are less explicit, leaving open the possibility that a new flu virus that was less deadly to everybody than the seasonal flu might still be said to cause a pandemic.
Like the professional literature generally, World Health Organization documents also use the term “influenza pandemic” inconsistently. Among the inconsistencies: How severe does a flu pandemic have to be to qualify as a flu pandemic?
For instance, most WHO documents do not call the 1977 global spread of a 1950 strain of H1N1 a pandemic. But at least one document on the WHO website ![]() makes the opposite judgment:
makes the opposite judgment:
The most benign pandemic was when type A(H1N1) viruses from 1950 re-appeared for unknown reasons in 1977, and affected mainly infants and children. Mortality did not increase…. The 1977 pandemic was quite different from the previous ones.
How and why WHO changed its use of the term “influenza pandemic”
![]() The word “pandemic” came into common use among nonprofessionals only when WHO and other health agencies started issuing warnings about the specter of bird flu. Bird flu (H5N1) in humans is certainly a novel subtype. And it is potentially incredibly serious; so far, it has killed over half the people who caught it – compared to 2–3 percent for the 1918 pandemic (the poster child of serious flu pandemics) and well under one tenth of one percent for swine flu so far.
The word “pandemic” came into common use among nonprofessionals only when WHO and other health agencies started issuing warnings about the specter of bird flu. Bird flu (H5N1) in humans is certainly a novel subtype. And it is potentially incredibly serious; so far, it has killed over half the people who caught it – compared to 2–3 percent for the 1918 pandemic (the poster child of serious flu pandemics) and well under one tenth of one percent for swine flu so far.
The saving grace of bird flu is that it’s extremely difficult to catch. Except for a handful of conspiracy nuts who murmur about cover-ups, there is universal agreement that bird flu is a panzootic or epizootic (among birds), but not a pandemic or epidemic because as a human disease it is rare and hard to catch, not widespread and easy to catch. Bird flu won’t go pandemic unless the virus acquires the ability to pass easily from one person to another. If that ever happens, and if the bird flu virus remains anywhere near as virulent as it is today, it will be by far the worst influenza pandemic (and the worst disease catastrophe) in history.
Bird flu warnings said, in essence: “A bird flu pandemic might well be horrific. Thank God bird flu hasn’t gone pandemic yet. Hope to God it never does.” So if the general public learned any definition of a pandemic, it learned a scary one.
With bird flu in the backs of their minds, WHO officials kept on refining and streamlining the complex WHO guidance document for phased planning and response before, during, and after influenza pandemics.
In the 1999 and 2005 versions, severity had been one of many factors that would (1999) or could (2005) be taken into account in decisions about whether to raise the pandemic phase in the run-up to declaring a pandemic.
Here’s a key reference to severity ![]() in the 1999 version:
in the 1999 version:
The Pandemic will be declared when the new virus sub-type has been shown to cause several outbreaks in at least one country, and to have spread to other countries, with consistent disease patterns indicating that serious morbidity and mortality is likely in at least one segment of the population.
In the 2005 version ![]() , severity appears most prominently in this footnote, appended to the definitions of pandemic phases and reiterated five times throughout the document:
, severity appears most prominently in this footnote, appended to the definitions of pandemic phases and reiterated five times throughout the document:
The distinction between phase 3, phase 4 and phase 5 is based on an assessment of the risk of a pandemic. Various factors and their relative importance according to current scientific knowledge may be considered. Factors may include: rate of transmission; geographical location and spread; severity of illness; presence of genes from human strains (if derived from an animal strain); other information from the viral genome; and/or other scientific information.
Officials and their expert advisors had reservations about both of these formulations. The severity of a flu outbreak can vary from region to region. It isn’t necessarily obvious in the early days of a new flu virus, and it can change suddenly (or slowly) as the virus mutates. It was clear that severity should be considered in figuring out what to do about a pandemic, but it was also clear that a pandemic, even a very serious pandemic, could look mild at the outset. Two of the last three pandemics had second waves more severe than the first – in the case of 1918, vastly more severe.
So when WHO published its revision of the 2005 guidance document in April 2009 ![]() , the newest version included the warning that “if symptoms are mild and not very specific, an influenza virus with pandemic potential may attain relatively widespread circulation before being detected; thus, the global phase may jump from Phase 3 to Phases 5 or 6.” The new version also removed the footnote that had been in the 2005 version, the footnote that had specified severity as one of the factors that “may” be considered when ratcheting from pandemic Phase 3 to 4 to 5. In the 2009 document, the revised phases were introduced in a section explicitly entitled “Definition of the phases.”
, the newest version included the warning that “if symptoms are mild and not very specific, an influenza virus with pandemic potential may attain relatively widespread circulation before being detected; thus, the global phase may jump from Phase 3 to Phases 5 or 6.” The new version also removed the footnote that had been in the 2005 version, the footnote that had specified severity as one of the factors that “may” be considered when ratcheting from pandemic Phase 3 to 4 to 5. In the 2009 document, the revised phases were introduced in a section explicitly entitled “Definition of the phases.”
Of course the official WHO influenza pandemic “guidance document” wasn’t the only document WHO published that talked about flu pandemics. There were lots of others. One that became controversial after novel H1N1 emerged was a document entitled “Pandemic Preparedness,” which had been on the WHO website since as early as February 2003. (Note: This page, originally on the WHO website, is now privately archived and may load very slowly.) Its very first paragraph offered a flu pandemic definition/description of its own that put severity front-and-center – far more so than any version of the guidance document:
An influenza pandemic occurs when a new influenza virus appears against which the human population has no immunity, resulting in several, simultaneous epidemics worldwide with enormous numbers of deaths and illness.
The 2009 updated guidance document had been in the works for a couple of years. But it was hurriedly posted on the WHO website just two or three days after H1N1 was first identified in late April 2009. Posted at the same time was a two-paragraph note explaining why WHO thought a new version was needed. The explanation did not mention anything about severity as an issue in the run-up to a pandemic declaration, most likely because it never occurred to WHO that eliminating references to severity was going to look evil later when people started wondering whether WHO had invented a fake pandemic-for-profit … a possibility that never crossed WHO officials’ minds.
It is crucial to remember that at the time the new guidance document was posted, the early news from Mexico was terrifying. On April 24, WHO issued its first announcement about the mysterious pneumonia cases in Mexico City:
In the Federal District of Mexico, surveillance began picking up cases of ILI starting 18 March. The number of cases has risen steadily through April and as of 23 April there are now more than 854 cases of pneumonia from the capital. Of those, 59 have died.
If that initial assessment from Mexico had been representative of swine flu’s ultimate case fatality rate, we would have been at the start of a pandemic about three times as bad as the pandemic of 1918. Fairly quickly – but not instantaneously – it became clear that there were far more cases (and thus a much lower percentage of deaths) than the earliest Mexico City news had suggested. Within weeks, the case fatality rate of the new flu virus began to look more like the data from the much milder pandemics of 1957 and 1968. By mid-summer it begin to look like the new pandemic might even be milder than the seasonal flu, in terms of its case fatality rate. But the first official Mexican report, in conjunction with cases popping up in California and Arizona, was justifiably terrifying to anyone who understood how bad a flu pandemic could be.
In April 2009, when WHO posted its newest version of its pandemic guidance document, it simply wasn’t worrying about a pandemic that might be too mild to qualify as real.
When WHO posted its new 2009 guidance document, it took the 2005 version off its website – though of course any reasonably skilled computer user could easily find cached copies and repost them. (Note: It is back on again.) Nor did WHO scour its website for other WHO documents with inconsistent references to pandemic severity. There were higher priorities. And officials were no doubt used to such inconsistencies, and used to reading past them.
But about a week after the new guidance document was posted, a CNN reporter asked WHO officials about that “Pandemic Preparedness” document, the one that said a flu pandemic involved “enormous numbers of deaths and illness.” WHO immediately removed the document from its website – and, needless to say, the critics (and even non-critics) immediately found cached versions to post on their own websites.
The version of the “Pandemic Preparedness” page that’s posted on the WHO website today has new definitions/descriptions of both a generic pandemic and an influenza pandemic. It doesn’t say anything about enormous numbers of deaths. It emphasizes that “Pandemics can be either mild or severe in the illness and death they cause, and the severity of a pandemic can change over the course of that pandemic.” So “mild” is still a contender. It also states that “An influenza pandemic may occur when a new influenza virus appears against which the human population has no immunity.” No immunity? Does that mean that novel H1N1 can’t have caused a pandemic, since many people had some immunity? It is really hard to get these definitions/descriptions just right, especially if people are going to hold you to them. So it’s silly to get defensive when you decide to change them.
What about the earlier version of “Pandemic Preparedness,” the one that specified “enormous numbers of deaths”? Here’s what WHO communication officer Natalie Boudou told the CNN reporter who first asked about it: “It was a mistake, and we apologize for the confusion…. [That definition/description] was put up a while ago and paints a rather bleak picture and could be very scary.”
Months later, much more senior WHO officials would repeatedly insist that they had never, ever, changed the “definition” of a “pandemic,” and that severity had never been a potential criterion – ignoring both their abandonment of that footnote in the 2005 guidance document and their quick effort to disappear the older version of the “Pandemic Preparedness” document. Natalie Boudou could have taught them how to acknowledge an indisputable reality more gracefully.
WHO did not update its pandemic guidance and pandemic phase definitions in order to justify declaring swine flu a pandemic. We can find nothing in the 1999 or 2005 guidance documents that would have stopped WHO from declaring that a pandemic was underway in June 2009. In fact, WHO might have declared swine flu a pandemic earlier under the old standards than the new, because the new ones had tougher criteria for geographical spread, requiring WHO to wait until the disease was spreading widely in at least two WHO regions. Because North and South America were part of the same WHO region, the new guidance document meant waiting until the swine flu virus was spreading widely in Europe as well.
WHO was simply trying to give national governments the benefit of its best, most recent thinking about flu pandemic phases as the world confronted the novel H1N1 virus.
Throughout May and June 2009, WHO – advised by its new Emergency Committee – kept trying to assess whether H1N1 met the criteria for Phase 6, a full-fledged influenza pandemic. Many influenza experts argued that it did, and chafed at WHO’s hesitation. But many national governments were afraid of over-alarming their publics, and successfully convinced WHO to wait. Their best technical argument was that H1N1 didn’t yet meet the new widespreadness criteria.
There wasn’t a lot of discussion back then about whether H1N1 was too mild to be called a pandemic. Mortality data in May and June were far less alarming than the earliest news from Mexico had been. H1N1 was beginning to look like a mild pandemic, more like the 1957 and 1968 pandemics than the horrific 1918 pandemic. But it was early days yet. The data on pandemic severity were still extremely spotty and tentative, and no one had any basis for deciding that H1N1 would or wouldn’t become more virulent as it spread.
So yes, right after H1N1 was identified as a novel flu virus causing human-to-human spread in Mexico, WHO introduced new flu pandemic phase definitions that did not include an earlier footnote specifying that “severity of illness” “may be considered” as one of many factors in assessing the distinctions among phases 3, 4, and 5.
But WHO didn’t make this change in order to make it easier to declare H1N1 a pandemic. If anything, the new phase definitions/descriptions made it harder for WHO to declare H1N1 a pandemic, because they gave national governments an argument that the virus wasn’t widespread enough yet. But we don’t think they were introduced for that purpose either. They were introduced because they were more in line with current knowledge, and with changes in the International Health Regulations and other protocols that had been updated since 2005. And they were introduced because they had been in development for about two years, and suddenly it looked like they were urgently needed right now.
Mishandling the Definitional Controversy
![]() Swine flu was never as scary as bird flu – not even close. But in the early days it looked pretty scary. It was killing people. It was certainly a new flu strain, even though it wasn’t an entirely new subtype; there had been other H1N1 strains in humans, but never this weird swine-bird-human hybrid H1N1. And unlike bird flu, it was spreading rapidly between humans and was virtually certain to spread everywhere. Early on, calling it a pandemic seemed like a no-brainer.
Swine flu was never as scary as bird flu – not even close. But in the early days it looked pretty scary. It was killing people. It was certainly a new flu strain, even though it wasn’t an entirely new subtype; there had been other H1N1 strains in humans, but never this weird swine-bird-human hybrid H1N1. And unlike bird flu, it was spreading rapidly between humans and was virtually certain to spread everywhere. Early on, calling it a pandemic seemed like a no-brainer.
Things looked different by January 2010. By then it was pretty clear – at least in developed countries with good surveillance – that swine flu had been mild and was already receding in most places. National governments that had ordered millions of doses of vaccine and antiviral drugs were realizing that they had bought far more than their people wanted – and many were imagining in hindsight that they had bought more than they could possibly have needed. Individuals who had been aroused to a state of alarm by their governments’ justified early warnings were realizing that their fears had turned out unnecessary – and many were imagining in hindsight that the warnings had been foolish (or intentional) scaremongering.
And so controversy started to emerge about whether swine flu was a real pandemic at all. In January 2010, the controversy was still limited. You might say it was in Phase 4, with extensive community transmission in one WHO region: Europe.
That was the context in which the question of the definition of a (flu) pandemic came back to haunt WHO.
Critics claimed, with some justice, that WHO had changed its definition of a (flu) pandemic right after swine flu’s arrival. The webpage entitled “Pandemic Preparedness” had been replaced; its dramatic reference to “enormous numbers of deaths and illness” was gone. The revised guidance document no longer had a footnote under the subhead “Definition of the phases” specifying that “severity of illness” “may be considered” in assessing the distinctions among the phases. There were hundreds of other differences between the 2005 guidance document and the April 2009 guidance document. But skeptical, suspicious, and conspiracy-minded people zeroed in on the severity factor.
It’s interesting to speculate on the very different controversy that might have arisen if the pandemic had been severe. Then the critics’ microscopes would probably have focused on the new geographical spread criteria in the April 2009 guidance document, ignoring that document’s de-emphasis on severity. “Just as the deadly new virus was starting to spread,” the critics might well have pointed out, “WHO introduced new definitions of the pandemic phases. Because of those new definitions, invaluable time was lost while WHO waited till H1N1 was widespread not just in North and South America but also in Europe.”
But the pandemic was mild, and so the controversy was all about the de-emphasis on severity.
WHO responded categorically that it had not changed the definition of the word “pandemic.” It even urged critics to Google the phrase “definition of pandemic” ![]() and see for themselves. WHO officials insisted, accurately, that the word “pandemic” had always referred to widespreadness, not severity. This was legalistically true but willfully disingenuous. WHO was right that the generic definition of “pandemic” hadn’t changed, but that wasn’t what the critics were charging (even when those were the words they used). They were accusing WHO of changing its definition/description of a flu pandemic.
and see for themselves. WHO officials insisted, accurately, that the word “pandemic” had always referred to widespreadness, not severity. This was legalistically true but willfully disingenuous. WHO was right that the generic definition of “pandemic” hadn’t changed, but that wasn’t what the critics were charging (even when those were the words they used). They were accusing WHO of changing its definition/description of a flu pandemic.
Instead of respectfully discussing that claim on its merits, WHO ended up leaning heavily on two distinctions: “pandemic” versus “influenza pandemic” and “definition” versus “description.” (At times it seemed to be debating the definition of “definition.”) The critics kept finding WHO descriptions of the characteristics of flu pandemics that included severity, and accusing WHO of ignoring that key feature. WHO kept insisting that the definition of a (generic) pandemic had not been changed. It was like watching two angry, coachless debate teams.
The January 2010 controversy was led by a small group of European politicians, working through a non-Parliamentary organization of European governments called the Council of Europe. Their webcast hearings and news releases attracted significant media attention in Europe but virtually none in the U.S.
What made the charges hard to rebut is that they were partly dead right and partly off-the-wall wrong: right that WHO had eliminated several references to severity as a factor related to the declaration of flu pandemics; right that WHO had issued alarming warnings about a pandemic that was turning out fairly mild; right that WHO had shown great reluctance to concede the mildness and downgrade the tone of its warnings … and wrong that swine flu was a “fake pandemic” declared by WHO in order to enrich Big Pharma.
Shortly before the Council of Europe meeting at which WHO and pharmaceutical trade association officials were to be questioned, we contacted the most senior WHO decision-makers we know and urged them to concede the critics’ valid charges, and contest only the core (and false) charge of a “fake pandemic for profit” conspiracy. But apparently top WHO officials had convinced themselves that the critics had no valid charges. They chose to contest every charge the critics were making.
After watching the maddening Council of Europe interrogation of the WHO’s Keiji Fukuda, and his defensive and disingenuous-sounding responses, we wrote about it all in a piece entitled “It’s Not a Fake Pandemic – but WHO’s Defense Lacks Candor.” (To its credit, even after that WHO has continued to hire one of us (Jody) for short-term work on outbreak communication in Asia.)
Pretty much the same issues came roaring back on June 3, 2010, with the coordinated release of the Council of Europe report ![]() and the BMJ article.This time the media attention has been far greater, not just in Europe but also in North America, India, and elsewhere. This time we’re getting piles of emails from friends, colleagues, and clients, not just “flubies” or WHO-watchers, asking what we think about the charges against WHO. It’s clear that most of our correspondents don’t know that the “fake pandemic for profit” charges are false. If the controversy was at Phase 4 in January, it is now at Phase 6, a full-fledged pandemic. And for WHO, it is severe – a severe crisis of credibility.
and the BMJ article.This time the media attention has been far greater, not just in Europe but also in North America, India, and elsewhere. This time we’re getting piles of emails from friends, colleagues, and clients, not just “flubies” or WHO-watchers, asking what we think about the charges against WHO. It’s clear that most of our correspondents don’t know that the “fake pandemic for profit” charges are false. If the controversy was at Phase 4 in January, it is now at Phase 6, a full-fledged pandemic. And for WHO, it is severe – a severe crisis of credibility.
This definitional controversy would never have arisen if the swine flu pandemic had turned out obviously “severe” or “intermediate” (to use two of the three WHO severity assessment categories in the 2009 guidance document ![]() ; the third category is “mild”).
; the third category is “mild”).
And the controversy wouldn’t have mattered nearly as much if WHO had been non-defensively candid about how and why it changed its definitions/descriptions of the term “influenza pandemic,” and why language that referred to severity was absent from its revised definitions of the pandemic phases.
The ideal time for this WHO candor would have been in April, May, and June, when nobody knew yet how severe swine flu would turn out to be. The explanation would have made good sense to most people if it had been offered in real time: “We can’t know for some time yet how severe this new influenza virus will become. So we can’t afford to wait until we know about severity before ramping up to the higher phases of pandemic alert. That’s one main reason why the new phase definitions don’t mention severity.”
Of course WHO did point out that the pandemic’s future severity was uncertain. But as far as we can tell, it never did so in the context of the changed pandemic phase definitions. It’s not hard to understand this omission. WHO officials were all really busy (we almost can’t imagine how busy) trying to protect global public health during the early months of a pandemic that might turn more virulent at any time. Nobody was thinking back then: “Uh-oh, we better proactively make sure we’re not setting ourselves up to be accused of hyping a fake pandemic under the influence of Big Pharma.”
But WHO certainly should have been much more candid and much less defensive when the controversy started to take root, and when it participated in the January 2010 Council of Europe hearings.
The definitional controversy also wouldn’t have mattered nearly as much if WHO had taken official note – aggressively and repeatedly – that swine flu was turning out much milder so far than its initially justified pandemic warnings had led many people to expect. Here’s a list of message points that would have helped:
- Our use of the word “pandemic” to describe H1N1 is confusing many people – and the confusion is our fault.
- Generically, scientists use the term “pandemic” to mean a disease that is spreading widely.
- But we have often used the same term as shorthand for a severe or potentially severe disease that is spreading widely, or that we worry may begin to spread widely. That has been especially true when we talked about influenza pandemics.
- We have to admit: We often just say “pandemic” when we mean “influenza pandemic,” even though our definitions and descriptions of flu pandemics are narrower and in some cases scarier than the generic definition of a pandemic.
- In recent years we taught the world to fear a possible bird flu pandemic, which we worried could be catastrophically deadly. That pandemic hasn’t happened, at least not yet.
- Instead of the bird flu pandemic we feared, or another severe flu pandemic, we have this H1N1 flu pandemic, which is turning out much milder in terms of global public health, despite its tragic impact on many individuals.
- If things continue the way they are going so far, swine flu could end up killing fewer people than the average flu season.
- Is swine flu a pandemic? Yes. It is a new flu subtype that has spread throughout the world and caused significant harm to health.
- But it is not – at least not so far – the horrific sort of influenza pandemic that our bird flu warnings led many people to associate with the word “pandemic.”
- We must remain vigilant, since swine flu could take a turn for the worse. But so far, swine flu is a comparatively mild flu pandemic. In terms of the overall death rate, it may turn out to be the mildest flu pandemic in modern history. In hindsight, when it is finally over, some experts might even judge that it wasn’t severe enough to qualify as an influenza pandemic at all. Most, we think, will judge that it was a mild flu pandemic.
Only occasionally, and belatedly, has WHO accepted the blame for this terminological misunderstanding. These two paragraphs from a June 8, 2010 Medscape Medical News story are on target:
In addition, WHO spokesperson Gregory Hartl told Medscape Medical News that the previous agency description of a pandemic with the reference to “enormous numbers of deaths and illness” was just that – a description, not an official definition.
“It’s not a definition, but we recognize that it could be taken as such,” said Hartl. “It was the fault of ours, confusing descriptions and definitions.”
Other officials have sometimes acknowledged that their earliest swine flu warnings were unintentionally influenced by their years of nightmares about a drastically high-mortality pandemic launched by H5N1 bird flu.
But much more commonly, WHO has stonewalled:
- Accurately but legalistically denying that it ever changed the definition of the word pandemic.
- Failing to acknowledge that it did change the flu pandemic phase definitions in a way that de-emphasized severity, and did so right after novel H1N1 appeared.
- Refusing to admit that this statement, which was on the WHO website from 2003 until May 2009, sounds a lot like a definition: “An influenza pandemic occurs when a new influenza virus appears against which the human population has no immunity, resulting in several, simultaneous epidemics worldwide with enormous numbers of deaths and illness.”
That’s what WHO’s Keiji Fukuda did in January, when he was questioned at a Council of Europe hearing.
WHO’s June 10, 2010 response to the continuing criticism at least mentions the “enormous numbers of deaths and illness” document, though it implies – misleadingly – that this was an exception triggered by bird flu fears and that otherwise WHO has never stated or implied that flu pandemics need to meet any minimum severity requirement:
WHO regards severity as an important feature of pandemics and a critical factor when deciding on which actions to take. However, WHO has not required a set level of severity as part of its criteria for declaring a pandemic. Experience shows that all pandemics cause excess deaths, that severity can change over time, and that severity can vary according to location and population.
WHO has published three definitions of an influenza pandemic in the context of phases of pandemic alert…. The 2009 guidelines, including definitions of a pandemic and the phases leading to its declaration, were finalized in February 2009. The new H1N1 virus was neither on the horizon at that time nor mentioned in the document. The media make frequent reference to a 2003 document, available on the WHO web site, stating that an influenza pandemic results in “enormous numbers of deaths and illness”. At the time, this was considered a likely scenario should the highly lethal H5N1 avian influenza virus develop an ability to spread readily among humans, but it was never a formal definition.
But as we have seen, long before WHO got into trouble for abandoning severity as a potential factor for assessing the start of a flu pandemic, WHO had shown itself unwilling to take official notice that the pandemic was turning out mild, compared to other flu pandemics in history.
Consider the sequence of events:
- WHO warns the world that it faces possible disaster if bird flu ever goes pandemic. Millions learn that “pandemics” are disasters.
- Swine flu is discovered. No one know how severe it will turn out to be.
- WHO quietly introduces new pandemic phase definitions that de-emphasize severity as one of several factors that “may be considered” along the road from Phase 3 to Phase 5.
- Swine flu starts to look mild, but it’s way too soon to tell for sure. Governments appropriately prepare for things to get worse, ordering lots of vaccine and antivirals.
- WHO declares swine flu a pandemic.
- Swine flu looks more and more obviously mild. People start wondering why WHO isn’t saying so.
- WHO keeps sounding the alarm about swine flu, continuing to call it “moderate” rather than “mild.”
- Swine flu incidence declines almost everywhere; it’s not only mild, it’s nearly gone, though it may come back.
- WHO doesn’t say that either; it turns down several opportunities to declare that swine flu is “post-peak,” even though its definition of the new “post-peak” phase has looked right for a couple months at least.
- To more and more people, it looks like WHO is hyping the pandemic – and they start wondering if it wasn’t all hype from the start.
- Trying to come up with a motive for WHO’s reluctance to stand down from its swine flu severity assessment and alert level, more and more people fasten on possible conflict of interest – all those outside advisors with ties to the drug industry. The question becomes: Is WHO partnered with Big Pharma, or was it only duped by Big Pharma?
Two solutions to a non-problem
![]() Today, a few top influenza experts privately say they don’t think H1N1 is really a pandemic. They don’t say so publicly because they want to remain in solidarity with WHO; they certainly don’t want to sound like they’re agreeing with those who claim WHO intentionally foisted a fake pandemic on the world for the benefit of the pharmaceutical industry. What these few top experts believe is simply that H1N1 turned out to be a false alarm. The world was right to take it seriously, and WHO was right to push the world to take it seriously – but it didn’t turn out bad enough to qualify as a pandemic.
Today, a few top influenza experts privately say they don’t think H1N1 is really a pandemic. They don’t say so publicly because they want to remain in solidarity with WHO; they certainly don’t want to sound like they’re agreeing with those who claim WHO intentionally foisted a fake pandemic on the world for the benefit of the pharmaceutical industry. What these few top experts believe is simply that H1N1 turned out to be a false alarm. The world was right to take it seriously, and WHO was right to push the world to take it seriously – but it didn’t turn out bad enough to qualify as a pandemic.
Most top experts say they consider H1N1 a pandemic, albeit a mild one (though perhaps not as mild as many people imagine, having boomeranged from excessive alarm to insufficient awareness that H1N1 really did kill a lot more young and middle-aged people than seasonal flu kills, at least in some countries). These experts – by far the majority – figure that we’ve been lucky enough to have three mild pandemics in a row: 1957 was pretty mild, 1968 was very mild, and 2009 was mildest of all in terms of overall mortality (so far). Nonetheless, they were all obviously pandemics: infectious disease outbreaks that spread throughout the world.
A few top experts seem to believe the whole concept of pandemic severity needs rethinking. They truly consider H1N1 a moderate pandemic, not a mild one. Some of them now refuse to call the 1957 and 1968 pandemics “mild” either, even though they used to.
What the first two groups of experts are disagreeing about isn’t how mild the H1N1 virus has turned out to be so far. There is still some debate on that question, as we have seen. But this is the best-studied pandemic (or in some views, almost-pandemic) ever, and eventually everyone will know with considerable precision how bad it was. The experts will ultimately reach something like consensus on that empirical question. They may never reach consensus on the definitional question: How bad should a new, globally widespread influenza virus have to be to end up qualifying as a pandemic?
We have been here before. In 1977, an H1N1 strain virtually identical to one that had circulated in 1950 made a sudden new appearance in Anshan, China, and began to spread. (It was called the Russian Flu; many flu experts think it escaped from a lab somewhere in Asia.) Some experts count it as a pandemic. Most don’t – partly because it was mild and caused little or no excess mortality; and partly because it affected mostly people younger than 25, while most people over that age seemed to have protective immunity from previous exposure to the strain.
Flu experts don’t spend much time “debating” whether 1977 was a real pandemic or not. They agree on what happened in 1977. They disagree on whether to call what happened a pandemic. What’s to debate, now that it’s over?
But how would it have looked at the start, if there had been good enough surveillance in 1977 to pick up on it quickly, and if the WHO pandemic phase definitions had existed then? Presumably, there would have been no scary wake-up call like the one from Mexico in April 2009, because hardly anyone had died or become deathly ill from the Russian Flu. So maybe it wouldn’t have been called a pandemic or even a potential pandemic. But flu experts knew in 1977 that pandemics can start mild and then become more virulent. Maybe it would have made more sense to call the Russian Flu a pandemic or a potential pandemic when it first appeared, and then downgrade it later when there was no excess mortality.
Similarly, we believe we already know that what happened in 2009 was mild. By some measures it was slightly worse than the “mild” 1968 pandemic. By other measures it was milder than 1968, at least so far. Is swine flu a mild pandemic, or is it too mild to call a pandemic? Either of two answers will work fine. The choice just needs to be negotiated.
- Answer One: Flu pandemics have to be reasonably severe in order to count as pandemics. Here’s what we mean by “reasonably severe” – the minimum impact to qualify includes these criteria…. Of course when a new flu virus first appears, we won’t know if it’s going to be severe enough to count. We’ll have to treat every new influenza virus that’s starting to spread widely as a potential pandemic. WHO will recommend that countries start the process of developing a vaccine, increase stockpiles of antiviral drugs, activate their pandemic plans, remind people about hand-washing and staying home when they’re sick, etc. And of course we’ll have to ramp up surveillance. Over time, we will learn more and more about how severe the potential pandemic is. By the time it has been around for some months, we’ll have preliminary answers. But both because surveillance is spotty in many countries and because new flu viruses can become more or less virulent over time, we may not have a final answer until the pandemic – or not-quite-pandemic – is over.
- Answer Two: Flu pandemics don’t have to be severe in order to count as pandemics. Here’s our severity scale, distinguishing very mild, mild, moderate, severe, and very severe pandemics…. Of course when a new flu virus first appears, we won’t know how severe a pandemic it is going to be. We’ll have to treat every new influenza virus that’s starting to spread widely as a potentially severe pandemic. WHO will recommend that countries start the process of developing a vaccine, increase stockpiles of antiviral drugs, activate their pandemic plans, remind people about hand-washing and staying home when they’re sick, etc. And of course we’ll have to ramp up surveillance. Over time, we will learn more and more about how severe the pandemic is. By the time it has been around for some months, we’ll have preliminary answers. But both because surveillance is spotty in many countries and because new flu viruses can become more or less virulent over time, we may not have a final answer until the pandemic is over.
We can live with a pandemic definition that requires a minimum level of severity. A “potential pandemic” whose severity isn’t known yet will still require serious precautions. Eventually we’ll know if it was a pandemic or just a widespread outbreak of a mild new flu virus.
Or we can live with a pandemic definition with no minimum severity level. A pandemic whose severity isn’t known yet will require the same serious precautions. Eventually we’ll know how mild or severe the pandemic was.
The former solution has the advantage of not requiring public re-education. Most non-experts who have any opinion today think pandemics are at least somewhat more severe than seasonal flu. But if the technical experts prefer to teach people a new definition, that’s okay with us.
Either way, WHO will need a severity index for pandemics, a task WHO officials have long been pondering. Like the severity index for hurricanes, a pandemic severity index is essential so people and governments can make decisions based on expert assessments of how much risk a particular spreading flu virus poses – bearing in mind that severity can vary over time, place, population vulnerability, and response capacity. The question isn’t whether WHO needs to measure pandemic severity. It already tries to measure pandemic severity. The question is how low the severity index should go before a widespread flu outbreak is no longer called a pandemic. That too is analogous to hurricane severity. We have Category 1 hurricanes – which are the mildest of hurricanes, but certainly not the mildest of tropical storms (not to mention balmy tropical breezes).
If you are ending this section feeling that the answer doesn’t make much difference as long as there is consensus on what the terms mean, you get the point. As we said at the outset, definitions are stipulative and negotiated. It doesn’t matter where we draw the line between pandemic and not-quite-pandemic. What matters is that we all understand where the line has been drawn – so a WHO announcement calling a flu outbreak a pandemic means the same thing to WHO as it means to the journalists, governments, and ordinary people hearing the announcement and deciding what to do.
WHO’s Failure to Acknowledge until Recently the Legitimacy of Concerns about Transparency and Conflict of Interest
Column Table of Contents
WHO’s Failure to Acknowledge the Ongoing Mildness and Current Low Incidence of the Pandemic
Evidence that the swine flu pandemic has been mild so far
WHO’s unwillingness to call the pandemic mild
Explanations and impacts: Why WHO won’t call the pandemic mild, and why that matters
The mistake repeated: WHO’s failure to categorize the pandemic as “post-peak”
About definitions and redefinitions
How and why WHO changed its use of the term “influenza pandemic”
Mishandling the definitional controversy
Peter M. Sandman and Jody Lanard Declaration of Interests
![]() This seems to be the right place for us to share our own conflicts of interest.
This seems to be the right place for us to share our own conflicts of interest.
Peter started doing risk communication consulting for the World Health Organization during the SARS outbreaks of 2003, and has since consulted intermittently for senior WHO officials (including the Director-General) on a range of topics, including both bird flu and swine flu. Some of this work was paid, some unpaid; some was solicited, some unsolicited; some was used, some ignored. He has done risk communication seminars for the European WHO regional office, for the regional office of SEARO in New Delhi, and for the WHO/China country office in Beijing (the last two jointly with Jody Lanard). He also served on two WHO expert advisory groups, one to develop a SARS research agenda and one to develop outbreak communication guidelines, as well as an informal WHO communications advisory group that commented on proposed revisions of the 1999 pandemic phases.
Peter’s other pandemic-related government clients have included the U.S. Centers for Disease Control and Prevention, the Singapore Ministry of Health, Health Canada, and a number of state and local health agencies. His pandemic-related non-government clients have included Roche, American Airlines, Monsanto, Deutsche Bank, and the American Red Cross. Neither list is complete. Peter is also affiliated with the University of Minnesota Center for Infectious Disease Research & Policy, whose work focuses primarily on pandemic preparedness and response and is funded in part by pharmaceutical companies. Outside the pandemic realm, Peter has worked with literally hundreds of government and corporate clients, including many of the world’s leading pharmaceutical companies. Nearly all of this work, pandemic and non-pandemic, is paid; it is Peter’s principal source of income. His conflicts of interest, in short, are legion.
Jody’s conflicts of interests are narrower, but perhaps deeper.
- Her work with the World Health Organization began, as Peter’s did, when we volunteered our advice on how best to handle SARS risk communication.
- This led to her being hired in 2004 to research and write the first draft of a Background Document for WHO’s now-published “Outbreak Communication Guidelines.”

- She served on an informal WHO communications advisory group that commented on proposed revisions of the 1999 pandemic phases.
- Jody was hired again in 2005 for a three-month term in Geneva as senior WHO advisor for pandemic influenza risk communication. This position was funded indirectly by the U.S. CDC.
- She has also done extensive risk communication training and consulting for many WHO regional and country offices in Asia and Latin America, most recently in April 2010.
- WHO’s Western Pacific Regional Office and its Pan American Health Organization have sponsored Jody to do further work with the national governments of many countries in their regions, most intensively in the Philippines and in China.
- Much of Jody’s work in Asia and Latin America focused on risk communication aspects of bird flu and later swine flu. But much of the work focused on other risk communication problems entirely, from oil spills to natural disasters.
- Jody’s other pandemic-related clients have included the Australia Department of Health and Ageing, the Australia Department of Prime Minister and Cabinet, the Singapore Ministry of Health, Health Canada, Public Safety Canada, and a number of state and local health agencies.
- She has received travel expenses, and sometimes fees, to participate in flu pandemic planning conferences held by organizations such as the Center for Infectious Disease Research & Policy (CIDRAP); some of these conferences are funded in part by pharmaceutical companies.
- Jody has established ties with a large, worldwide network of current and former WHO officials, as well as officials of many national governments.
Both Peter and Jody have written extensively on various aspects of risk communication, including pandemic communication. Nearly all of this writing was unpaid and appears on our website, www.psandman.com. The pandemic-related writing is indexed at www.psandman.com/index-infec.htm.
Nearly all of our investments are in mutual funds and municipal bonds. Among the exceptions, however, are stock shares or bonds issued by three pharmaceutical companies: GlaxoSmithKline, ImClone (a wholly owned Lilly subsidiary), and Wyeth (now part of Pfizer).
The declarations above are not exhaustive, but we are pretty sure that a complete list would illuminate conflicts similar to those we have listed.
The content of this article does not violate any confidentiality agreements we have, or have had, with WHO.
No client, ex-client, or prospective client has asked us to write this assessment, and none has asked us to refrain from writing – but many have asked us what we think about WHO’s handling of the “fake pandemic” controversy. As to whether the content of this article has been influenced by our relationships with all the clients we have had and hope to have (including WHO on both counts): Of course it has.
There is nothing remotely new about recent “revelations” that WHO solicits and accepts advice from scientists with connections in the pharmaceutical industry. It has done so forever. It really has no choice but to do so, since the majority of top experts in many public health fields – infectious diseases among them – have such connections.
That too has been true forever. And that too could hardly be otherwise, given that the majority of research on the treatment of infectious diseases is funded by pharmaceutical companies. Some infectious disease experts work directly for Big Pharma. Some work directly for governments, where they can mostly steer clear of industry money. But most are academics, employed by universities, medical schools, and their affiliated hospitals. They take Big Pharma money to advise on what research is likely to prove fruitful; then they take Big Pharma money to do the research; then they take Big Pharma money to lecture on what the research revealed; then they take Big Pharma money to help convert the research results into marketable drugs that they hope will save lives. Along the way – for no money or virtually no money – they also give advice to the World Health Organization.
WHO is grateful for their advice. It ascertains the various conflicts of interest of its advisors; it tries to balance them; it keeps the conflicts in mind as possible sources of distortion or undue influence. And it goes about its business.
Nor is there anything remotely new about the “discovery” that WHO does not reveal to the public all there is to know about this network of advice and influence. There’s nothing secret about the facts in the previous paragraphs, though WHO hasn’t routinely emphasized them publicly. (Except now and then, the public isn’t much interested in how WHO vets its advisors.) The details that underlie these facts – the specific drug industry connections of specific WHO advisors – are sometimes publicly available and sometimes confidential. WHO insists on knowing them; it requires prospective members of its committees to fill out long “Declaration of Interests” forms detailing everything from consulting clients to stock ownership. (We have both worked for WHO – Jody more than Peter – and have both filled out these forms time and again.) WHO does not release the forms for public inspection, and most experts would be highly irritated if it were to do so. Sometimes it releases a broad summary or a few especially salient details, sometimes nothing, sometimes not even the names of the experts from whom it is receiving advice.
Thanks to the Internet, interested (or suspicious) outsiders can easily collect considerable information on the drug industry connections of various experts. Some is included in their curricula vitae; some is reported in the “competing interests” acknowledgments attached to journal articles; some turns up in other sources, including the online agendas of industry meetings. If you know the names of a few experts who sit on a particular WHO committee, it’s a matter of a few minutes’ work to come up with some Big Pharma connections for some of those experts that WHO “failed to disclose.”
So what’s new?
Only this: In June 2009, WHO declared H1N1 a pandemic without emphasizing that it was looking pretty mild so far (though it had looked pretty dire back in April), and without emphasizing the possibility and hope that it would remain mild. In addition, WHO declared the pandemic without acknowledging that there were grounds for debate over whether a mild pandemic ought to be called a pandemic at all, and without pointing out that it had just recently altered its own definitions/descriptions of influenza pandemic phases in a way that de-emphasized severity.
As events unfolded, the pandemic did in fact remain mild. And then it receded before vaccine was widely available. Prospective vaccinees noted that the pandemic was both mild and receding, and lost interest in getting vaccinated. This meant that a great deal of public expenditure on vaccines – which WHO calls ![]() “the most important intervention for preventing influenza and reducing its health consequences during a pandemic” – has turned out to be only marginally useful in the pandemic so far.
“the most important intervention for preventing influenza and reducing its health consequences during a pandemic” – has turned out to be only marginally useful in the pandemic so far.
The substantial cost of manufacturing a pandemic vaccine was justified at the outset because the pandemic’s virulence and future course were unknowable – but by 2010 that cost looked excessive to many because the pandemic was mild and nearly gone.
WHO had appropriately warned the world that things might get very bad. That didn’t happen (not yet, anyway). WHO should have joined the world in a sigh of relief – accompanied by a warning that a turn for the worse was still possible (and perhaps a wry half-apology for all that expiring, unused vaccine). Instead, WHO officials seemed to be the only people around who didn’t realize that the pandemic really and truly hadn’t been that bad.
People who found this perplexing went looking for an explanation. The explanation many of them found – with the help of some long-time WHO critics and anti-corporate politicians – was conflict of interest. “Ah, now we get it! Now we see why WHO officials and their outside advisors changed the pandemic phase definitions before they declared the pandemic. Now we see why they refused to notice that the pandemic was turning out mild. They did it to terrify the world into buying vaccines and antivirals from Big Pharma. The proof: WHO has secretly put people with Big Pharma connections onto its advisory committees.”
(Note: Some skeptics and WHO-bashers came up with a different explanation: “This is WHO’s way of maintaining its importance and justifying member state funding of WHO programs.” That explanation hasn’t gained nearly as much traction as the conflict-of-interest one.)
The recent meltdown in WHO’s credibility has focused on conflict of interest – and even more on transparency about conflict of interest. The complaint in a nutshell: “Why does WHO lean so heavily on advice from people with pharmaceutical industry connections, and what is it trying to hide when it refuses to tell us about those connections?”
These two issues did not cause WHO’s credibility meltdown; they are results of that meltdown. As long as most people trusted WHO’s public health pronouncements, the world was content to let WHO manage its own conflict-of-interest problems under the veil of confidentiality. But a lot of people gradually changed their minds when they noticed that WHO couldn’t seem to figure out (or acknowledge) that swine flu wasn’t a bad flu pandemic after all, as flu pandemics go. WHO seemed to be reporting from an alternative universe. That’s when even mainstream observers started to think that maybe we need somebody to look over WHO’s shoulder, checking out what kinds of people it’s relying on for advice.
Neither the Council of Europe report ![]() nor the BMJ article offers any evidence that members of WHO advisory committees have in fact distorted their advice in order to benefit the pharmaceutical industry financially. Neither publication claims to have such evidence. Instead, they make four main points:
nor the BMJ article offers any evidence that members of WHO advisory committees have in fact distorted their advice in order to benefit the pharmaceutical industry financially. Neither publication claims to have such evidence. Instead, they make four main points:
- There are members of WHO advisory committees with ties to the pharmaceutical industry, who might therefore have an incentive to give advice that would benefit that industry financially.
- Some advice from WHO advisory committees has in fact benefited the pharmaceutical industry financially – for example, advice about vaccines and antiviral drugs to combat the H1N1 pandemic.
- Some of the advice that has benefited the pharmaceutical industry financially is medically debatable, particularly in hindsight; not everyone agrees that WHO’s vaccine and antiviral recommendations did in fact significantly reduce H1N1 mortality or morbidity.
- WHO has been unwilling to give the public information about the conflicts of interest of its advisory committee members – information we would need in order to make our own judgments about whether those conflicts of interest might have distorted advisory committee advice to WHO, and thus WHO’s recommendations to the world’s governments.
All four of these points are simply true, but not necessarily culpable. It is the fourth point – WHO’s lack of transparency about the conflicts of interest of its advisory committee members – that makes the other three look suspicious.
The key question is whether these four points add up to a prima facie case that WHO got and took bad pandemic advice in deference to Big Pharma. We think they add up to no such thing – but again, WHO’s lack of transparency makes it look otherwise to many people.
In other words, the problem isn’t that members of WHO advisory committees often have conflicts of interest. The problem is that WHO isn’t routinely open with the public about those conflicts of interest. That worked okay as long as the substance of WHO public health pronouncements was widely trusted. But as soon as significant numbers of people stopped trusting what WHO had to say about the H1N1 pandemic, its transparency failures with regard to conflict of interest suddenly became newsworthy.
In this section we will look first at the question of transparency about conflict of interest. That’s fundamentally a risk communication question. And it’s a thorny one. It is a lot easier to make a case that WHO should be candid about the mildness of the H1N1 pandemic and the changing definitions/descriptions of pandemic phases than it is to claim that WHO should publish the details of every advisory committee member’s consulting activities and stock market investments.
Then we will discuss the issue of conflict of interest itself, which is not primarily a risk communication issue. We will step outside our field again, as we did when we discussed the evidence that the H1N1 pandemic has been mild so far (as flu pandemics go), and present a typology of conflicts of interest.
Our purpose is to show that the most dangerous conflicts are not the sort that the Council of Europe and BMJ seem to be most worried about, and not the sort that an improved WHO transparency policy could provide much reassurance about. We agree nonetheless that WHO needs to find ways to become more transparent about conflicts of interest. We are hopeful that more responsive transparency policies will help WHO regain credibility as it advises governments about urgent public health matters. But we doubt that improved transparency will have much impact on whether WHO advisory committees actually give advice that is relatively uncorrupted by competing interests.
Transparency
![]() The conflict-of-interest issue caught our attention with regard to the H1N1 pandemic in October 2009, when Science reported on allegations in Holland that well-known Dutch influenza expert Albert Osterhaus “has been stoking pandemic fears to promote his own business interests in vaccine development.” The Science article noted that “the Dutch House of Representatives had even slated an emergency debate about the matter.”
The conflict-of-interest issue caught our attention with regard to the H1N1 pandemic in October 2009, when Science reported on allegations in Holland that well-known Dutch influenza expert Albert Osterhaus “has been stoking pandemic fears to promote his own business interests in vaccine development.” The Science article noted that “the Dutch House of Representatives had even slated an emergency debate about the matter.”
There were other, less dramatic mutterings about WHO being influenced by advisors with pharmaceutical ties, and on December 3, 2009, WHO responded. Here’s what it said about conflict of interest:
WHO is aware of some concerns, expressed in the media, that ties with the pharmaceutical industry among experts on the Organization’s advisory bodies may influence policy decisions, especially those relating to the influenza pandemic….
Potential conflicts of interest are inherent in any relationship between a normative and health development agency, like WHO, and a profit-driven industry. Similar considerations apply when experts advising the Organization have professional links with pharmaceutical companies. Numerous safeguards are in place to manage possible conflicts of interest or their perception.
External experts who advise WHO are required to provide a declaration of interests that details professional or financial interests that could compromise the impartiality of their advice. Procedures are in place for identifying, investigating and assessing potential conflicts of interest, disclosing them, and taking appropriate action such as excluding an expert from participating in a meeting….
All members of the Emergency Committee sign a confidentiality agreement, provide a declaration of interests, and agree to give their consultative time freely, without compensation. Members of the Committee are drawn from a roster of about 160 experts covering a range of public health areas. The framework for membership is set out in the International Health Regulations. Each State Party to the Regulations is entitled to nominate one member of the roster and additional experts are appointed by the Director-General. Recommendations of the Emergency Committee are immediately made public on the WHO web site together with the relevant decisions of the Director-General….
Allegations of undeclared conflicts of interest are taken very seriously by WHO, and are immediately investigated.
In other words: “We’ve got it covered.” WHO’s December 2009 position was that WHO expert advisors must declare their conflicts to WHO, which polices them effectively – so there is no need for the public to watch over the process. “Trust us. We know what we’re doing.”
The issue gained more widespread European attention a week later, when the Council of Europe started making strange accusations. Dr. Wolfgang Wodarg, former chairman of the Council’s health committee, focused initially on the charge that H1N1 was “a mild flu and a false pandemic.” The “mild flu” claim is overstated; so far H1N1 has been a mild flu pandemic as pandemics go, but “mild flu” doesn’t capture it for us. As for “false pandemic,” the claim is tendentious, but not as completely baseless or “disrespectful” as WHO officials maintain.
But Wodarg and his colleagues soon transitioned to two much nastier and far less supportable claims: that the pandemic response was engineered by pharmaceutical companies in order to sell antivirals and vaccines, and that the vaccines are dangerous. The first paragraph of the motion ![]() he and others submitted for Council of Europe deliberation puts it this way:
he and others submitted for Council of Europe deliberation puts it this way:
In order to promote their patented drugs and vaccines against flu, pharmaceutical companies have influenced scientists and official agencies, responsible for public health standards, to alarm governments worldwide. They have made them squander tight health care resources for inefficient vaccine strategies and needlessly exposed millions of healthy people to the risk of unknown side-effects of insufficiently tested vaccines.
Six months later, by the time the Council of Europe report ![]() and the BMJ article were released on June 3, 2010, WHO had come to realize that mere reassurance wasn’t going to do the job. Better transparency and accountability policies were needed.
and the BMJ article were released on June 3, 2010, WHO had come to realize that mere reassurance wasn’t going to do the job. Better transparency and accountability policies were needed.
So WHO’s June 10 response was much more responsive (not just “reassuring”) on a number of points. And in line with good risk communication principles, the response shared dilemmas about WHO’s past conflict-of-interest practices and potential changes in those practices:
Allegations that WHO declared a pandemic to boost the profits of the pharmaceutical industry arise from WHO’s use of expert advisers and the way declarations of interest from these experts are handled….
The publication of summaries of relevant interests following meetings is inconsistent and needs to be made routine. WHO further acknowledges that safeguards surrounding engagement with industry need to be tightened, and is doing so….
The emergence of the new H1N1 virus prompted the first convening of an Emergency Committee under the IHR. At that time, WHO debated whether or not to publicly disclose the names of members, and faced a dilemma. On one hand, the names of members of other advisory groups are made public after they meet; the identification of persons offering guidance adds transparency to their advice and subsequent WHO decisions. On the other hand, experiences during the SARS outbreak demonstrated the considerable economic and social disruption caused by some public health emergencies, meaning that experts could well be lobbied or pressured for commercial or political reasons, potentially compromising the objectivity of their advice.
After considering these issues, WHO decided to apply its usual practice of disclosing the names of experts after an advisory body has completed its work. The members themselves welcomed this decision as a protective measure, and not as an attempt to veil their deliberations and decisions in secrecy. However, given the duration of the pandemic, the Emergency Committee has held a number of meetings over more than a year, rather than a single meeting like most advisory groups, thus delaying even further the release of the names of its members.
WHO is now fully aware that this decision has fostered suspicion that the Committee might be providing guidance shaped by commercial interests or pressures. Names of members and a summary of relevant declarations of interest will be made public when the Committee advises that the pandemic has ended. Procedures for revealing names of members of future Emergency Committees are under review….
In 2002, WHO convened a consultation with experts to develop a document, WHO guidelines on the use of vaccines and antivirals during influenza pandemics, which was published in 2004. Some critics have alleged that certain experts who participated in the meeting and the drafting of the guidelines had ties with industry interpreted as conflicts of interest. In line with WHO policy, all experts who participated in this meeting were required to submit a declaration of interest form and all such forms were duly reviewed by WHO. However, a summary of relevant interests was not issued together with the publication. WHO regrets this oversight.
Since that time, a number of administrative and legal changes have been implemented to strengthen procedures for addressing potential conflicts of interest that might influence the advice provided to WHO. WHO is committed to tightening these procedures further and ensuring their more consistent application.
WHO is making two significant substantive concessions here: It needs to tighten its conflict-of-interest requirements, and it needs to share more conflict-of-interest information (starting with the names of advisory committee members!) with the public. The details are still scanty, but the promise to improve in both areas is clear.
Beyond these two substantive concessions, the June 10 response also makes it clear that WHO understands that it was too slow to start taking the criticism to heart: “WHO is now fully aware that [the decision to keep the Emergency Committee members’ names secret] has fostered suspicion that the Committee might be providing guidance shaped by commercial interests or pressures.” This is an important improvement, six months after the merely reassuring response on December 3, 2009.
WHO, we assume, came to these three concessions under pressure – specifically, under pressure resulting from the June 2010 Council of Europe and BMJ reports. In recent years, many scientific organizations and journals have faced similar pressure to ratchet up their own requirements governing both conflict of interest and disclosure of conflict of interest. They responded to that pressure. Now WHO faces a similar need to respond.
It’s not the first time. The last huge WHO conflict-of-interest controversy focused on the scandalous infiltration of WHO by the tobacco industry, culminating in a 2000 report (by an advisory committee) entitled “Tobacco Company Strategies to Undermine Tobacco Control Activities at the World Health Organization.” ![]() The committee concluded:
The committee concluded:
In one of their most significant strategies for influencing WHO’s tobacco control activities, tobacco companies developed and maintained relationships with current or former WHO staff, consultants and advisors. In some cases, tobacco companies hired or offered future employment to former WHO or UN officials in order to indirectly gain valuable contacts within these organizations that might assist in its goal of influencing WHO activities. Of greatest concern, tobacco companies have, in some cases, had their own consultants in positions at WHO, paying them to serve the goals of tobacco companies while working for WHO. Some of these cases raise serious questions about whether the integrity of WHO decision making has been compromised. All of them illustrate the need for rules requiring that current and prospective WHO employees, including consultants, advisors, and members of expert committees, disclose any ties to the tobacco industry.
It’s ironic that WHO got into big-time trouble for letting itself be infiltrated by tobacco interests. WHO hates the tobacco industry. Its opposition to Big Tobacco is entirely different from its suspicion of Big Pharma. The latter is grounded largely in WHO’s anti-corporate values; WHO has nothing against Big Pharma’s product line, medicines. But tobacco itself is the target of a determined WHO eradication campaign.
Today, WHO all-but-forbids its consultants and advisors to have any current or recent ties to the tobacco industry. But for other conflicts of interest, it settles for requiring its consultants and advisors to disclose such ties – to WHO itself, not to the public.
WHO’s organizational values with regard to conflict of interest are deducible from its policies and actions. Tobacco aside, those policies and actions suggest six implicit propositions:
- Most experts have multiple masters. Conflicts are real and commonplace.
- It’s essential for experts to reveal their conflicts in confidential forms that WHO then assesses.
- Once the conflicts are revealed, it’s not difficult to balance them to make sure a single perspective does not dominate an advisory committee discussion.
- Besides balancing, the other main protection against conflicts is awareness; everyone considers everyone else’s advice in the context of that person’s conflicts.
- This is more a question of appearances than actual biases, because most experts are honorable and objective.
- Revealing detailed conflict-of-interest information to the public would unnecessarily invade the privacy of WHO consultants and advisors.
Take a minute to look at a typical WHO “Declaration of Interests” ![]() form – this one for experts being considered for a meeting to help draft a WHO guidance document on mutagenicity testing for chemical risk assessment. There are doubtless more onerous forms in existence (we don’t even want to imagine the forms prospective U.S. Supreme Court Justices have to fill out), but this one isn’t sketchy.
form – this one for experts being considered for a meeting to help draft a WHO guidance document on mutagenicity testing for chemical risk assessment. There are doubtless more onerous forms in existence (we don’t even want to imagine the forms prospective U.S. Supreme Court Justices have to fill out), but this one isn’t sketchy.
Every prospective WHO consultant, advisory committee member, and short-term professional employee fills out a form more or less like this one.
Much of the required information is information the person filling out the form may have made prior commitments not to divulge. In particular, some organizations require their consultants and contractors to sign confidentiality agreements promising not to reveal their connection with that organization. We have worked with organizations that made this stipulation – including the World Health Organization itself. Here’s a clause from a WHO consulting contract ![]() we have signed:
we have signed:
The Consultant shall not advertise, or seek promotion of, the fact that he/she is a consultant to the World Health Organization. Also, the Consultant shall in no other manner whatsoever use the name, emblem, or official seal of the World Health Organization in connection with his/her business or otherwise.
Those last two words, “or otherwise,” nail it. A former WHO consultant who felt obliged to reveal his or her prior WHO work on a WHO “Declaration of Interests” form would face an impossible double-bind.
The confidentiality-versus-disclosure dilemma is made all the more acute by this WHO contract provision:
CONSENT TO DISCLOSURE. The Secretariat will assume that you consent to the disclosure of any relevant conflicts to other meeting participants and in the resulting report or work product, unless you check “no” in the space provided here. If you check “no”, the Secretariat will not disclose the information without your prior approval, although this may result in your not being able to participate in the meeting or conference.
For reasons that are pretty obvious by now, WHO virtually never publishes the detailed conflict-of-interest information it collects from consultants and advisors – even though it tries to reserve the right to do so. It uses the “Declaration of Interests” forms to decide whether a prospective advisory committee member might have a disqualifying conflict, and to make sure the conflicts of those who make the cut are taken into account and are reasonably balanced, not all in the same direction.
Committee members are typically sent capsule biographies of all members; similar biographies often appear in published committee work products. Such a biography would probably include the information that X used to be vice-president of the ABC Biopharma Company, but probably not the information that Y has sometimes consulted for ABC, got a research grant from them once, and owns some ABC stock – although WHO would have all that information. Other committee members might or might not be aware of Y’s ABC ties. Some of those ties might come up in committee discussions if they weren’t confidential and Y thought they were relevant. Otherwise most committee members probably wouldn’t know much unless they did a little Googling on their own … and wouldn’t know everything (the stock ownership of the committee member’s spouse or children, for example) even then. The rest of us could resort to Google too, of course, if we knew the committee members’ names.
As far as we can tell, on the infrequent occasions when WHO does publicly report committee members’ conflicts of interest, it normally does so not in an overall summary but by listing specific conflicts of specific individuals that it judges important to acknowledge. See for example the notes at the bottoms of this list of members of an ad hoc working group and this list ![]() of WHO’s Strategic Advisory Group of Experts (SAGE) on immunization. Both lists were published in 2009.
of WHO’s Strategic Advisory Group of Experts (SAGE) on immunization. Both lists were published in 2009.
The information in these notes is far scantier than the information in the Declarations of Interests submitted to WHO. But it’s a lot more than nothing. It’s the most salient conflicts of interest of those committee members judged to have some pretty salient conflicts of interest.
Apparently, publication of certain committees’ members’ conflicts wasn’t yet WHO policy in 2002, when WHO convened an expert consultation to develop guidelines on the use of vaccines and antivirals during influenza pandemics; nor was it policy in 2004, when the guidelines were published. So no conflicts of interest were ever publicly reported for that committee – a key point in the BMJ critique.
On June 8, after that critique was published, WHO spokesman Gregory Hartl candidly called the absence of published conflict-of-interest data in 2004 an “oversight.” We don’t think he meant that somebody forgot to append the data to the published list of committee members. He meant that including information on advisory committee conflicts of interest wasn’t the policy back then, but it should have been. As Medscape Medical News reported: “‘It was an oversight,” said Hartl. ‘If we were using today’s practices, we would have published the summary for the relevant interests. The way we handle [declarations of interests] is a work in progress.’”
So there has been progress in recent years. WHO didn’t used to publish conflict-of-interest information about advisory committee members. Today, WHO publishes some information about some conflicts of some members of some committees.
As WHO’s June 10 response to the European Council and BMJ critiques strongly suggests, there is more progress to come. In response to its rapid and disheartening loss of credibility over the so-called “fake pandemic,” WHO is beginning to take steps to develop more transparent accountability mechanisms regarding its advisory committee members and their conflicts of interest. Risk communication experts have long counseled that it is wise to maximize transparency and accountability when trust is high, as bulwarks against subsequent loss of trust. But better late – when trust is low and needs to be restored – than never.
One big issue still in contention: For some committees, WHO’s current stance is not to reveal any conflict-of-interest information until the committee’s work is done. This is the case for the immensely impactful WHO Emergency Committee, which advises on how to assess and respond to the H1N1 pandemic. The Emergency Committee’s work won’t be done until the pandemic is over.
The main problem with the Emergency Committee members’ Declarations of Interests isn’t that WHO doesn’t know about the members’ conflicts, potential conflicts, and appearances of conflicts. WHO does mostly know. The problem is that WHO, as usual, chose not to make this information public. The public has had to trust WHO’s judgment that the committee members’ conflicts were unlikely to corrupt the advice they provided about pandemic preparedness and pandemic management. Once WHO’s trustworthiness and judgment began to be called into question, that simply wasn’t good enough anymore.
And in the case of the Emergency Committee members, the public can’t even Google their names and do its own conflict-of-interest research – because WHO has chosen not to release the names. For committees that are expected to meet only once or twice, sometimes the names aren’t released until the committee’s work product is released. For committees (like the Emergency Committee) that are longer-lived than that, providing ongoing advice rather than producing a single written report, the names are sometimes (but not invariably) released before the work is done. The names of members of WHO’s important Strategic Advisory Group of Experts on Immunization (the so-called SAGE Committee) are readily available.
But not the Emergency Committee. “Our decision not to make these names public,” Director-General Chan said on June 8, “was motivated by a desire to protect the experts from commercial or other influences.”
That’s more than a little mind-boggling. In order to protect the committee members from new conflicts of interest, WHO won’t say who they are so people can begin figuring out what their current conflicts of interest are (if they have any).
The world’s top influenza and public health experts don’t need that kind of protection. They live in a sea of other people’s opinions about how the pandemic should be managed – the opinions of other experts; the opinions of Big Pharma and other corporate interests; and the opinions of their governments and other governments (not just ministries of health, either; ministries of tourism, agriculture, foreign affairs, and trade have also had plenty to say about pandemic response).
Would the members of the Emergency Committee have to endure some additional lobbying if their names were known? Probably. Might they be influenced by that lobbying? Certainly – just as they might have been influenced all along by what they heard from everyone around them (including the media coverage). WHO is in the untenable position of asserting that Emergency Committee members can be trusted to render good advice despite their existing (not-to-be-revealed) conflicts of interest, but must remain anonymous in order to avoid new conflicts of interest that might corrupt their advice.
Rather than being protected through anonymity, the committee members need only to be required to declare any efforts to influence them, just as they are required to declare other past or current conflicts of interest, potential conflicts of interest, or situations that may appear to be conflicts of interest.
It’s obvious to us that WHO should name the Emergency Committee members – unless WHO has promised them it won’t, and the members choose to hold WHO to that promise, which is hard to imagine.
Less obvious is the extent to which WHO should reveal the contents of the committee members’ “Declaration of Interests” forms. A short list of the most salient conflicts, like the SAGE Committee list ![]() , would certainly be a step in the right direction, though in the current mood of mistrust we doubt it’s detailed enough to meet the need.
, would certainly be a step in the right direction, though in the current mood of mistrust we doubt it’s detailed enough to meet the need.
We can’t predict how WHO will ultimately change its policies regarding transparency about advisory committee members’ conflicts of interest (and their names). It’s a genuine dilemma. Releasing all the details in the Declarations of Interest would be a substantial invasion of privacy, and a substantial incentive to stay off WHO advisory committees. Releasing only broad summaries (“seven committee members reported industry-funded research grants in the past five years”) probably wouldn’t significantly reduce the hostility of critics and the skepticism of the public – nor would releasing selected details on just some of the committee members. We hope WHO can find an acceptable midway point.
But we also hope WHO will begin to realize that conflict of interest (and transparency about conflict of interest) is not the fundamental issue. The fundamental issue is that the World Health Organization has depleted its reserves of trust and credibility. It is significantly less trusted by governments, journalists, and the public today than it was at the start of the swine flu pandemic. Painful as that must be, WHO needs to acknowledge this truth … and adjust to it.
In the past year, WHO has become much better known – and much less trusted. It squandered trust by:
- Warning the world about H1N1 in ways that put insufficient emphasis on uncertainty – that sounded to many like predictions of disaster;
- Paying insufficient attention to the ways in which H1N1 turned out mild and even anticlimactic – persisting in an alarmist tone not just when it appropriately warned that events could still take a turn for the worse but even when it described what had happened so far;
- Never conceding that some of the precautions taken in anticipation of a serious pandemic might in hindsight have been excessive, even though they were appropriate given what was known at the time;
- Deciding in early June 2010 not to declare the H1N1 pandemic to be post-peak but rather insisting that we were still in Phase 6, even though the data considered at the June 1 Emergency Committee meeting sounds like it matches WHO’s definition of the post-peak phase;
- De-emphasizing severity in its revised definitions/descriptions of the pandemic phases and in its descriptions of influenza pandemics, implementing the revisions just as H1N1 was beginning to spread, and then falsely denying that severity had ever been a factor that “may be considered” in the run-up to declaring a pandemic; and
- Never properly explaining this change once questions arose – and repeatedly making misleading statements about the change when denying accusations of having changed the “definition of a pandemic.”
WHO’s June 10, 2010 response to its critics – the response that made major acknowledgments and concessions on conflict of interest and transparency – gave no quarter whatever on these more fundamental issues.
We do not believe that WHO’s mishandling of pandemic communication had anything to do with conflicts of interest among the members of its Emergency Committee. But WHO did mishandle pandemic communication – and that is what led to demands for transparency about the committee members’ conflicts of interest. Improving WHO transparency policies regarding conflict of interest is an appropriate response to the critics’ skepticism and suspicion. Being more transparent and apologetic about the ways WHO has mishandled pandemic communication will help even more on the road to restoring WHO’s trust – and its trustworthiness.
Conflict of Interest
![]() The literal definition of conflict of interest makes it clear that we all have such conflicts. The first sentence of the Wikipedia “conflict of interest” entry is instructive: “A conflict of interest (COI) occurs when an individual or organization is involved in multiple interests, one of which could possibly corrupt the motivation for an act in the other.” The italicization of “possibly” is in the original. Conflicts of interest don’t have to undermine performance; they merely must have the potential to do so.
The literal definition of conflict of interest makes it clear that we all have such conflicts. The first sentence of the Wikipedia “conflict of interest” entry is instructive: “A conflict of interest (COI) occurs when an individual or organization is involved in multiple interests, one of which could possibly corrupt the motivation for an act in the other.” The italicization of “possibly” is in the original. Conflicts of interest don’t have to undermine performance; they merely must have the potential to do so.
Suppose for example that you come to realize that what’s best for your employer isn’t actually what’s best for your career … or, perhaps, for your marriage. On the job you’re expected to make decisions in your employer’s interest. If your motivation to do so is diminished (“corrupted”) by your awareness of your other interests, you have a conflict of interest. Even if you end up doing what’s best for your employer, you still had a conflict of interest, though you resolved it satisfactorily. If you end up actually compromising your work performance, then you have resolved your conflict unsatisfactorily – especially if you neglect to tell your employer: “I did it that way because it’s best for my career/marriage. It’s not really what’s best for the company.”
You probably have similar conflicts of interest at home, where you are (arguably) expected to do what’s best for your family, but are sometimes motivated to compromise that goal in order to achieve other goals – career advancement, employer satisfaction, hedonic pleasure, world peace, whatever.
The point is: Conflicts of interest are everywhere. We all have them, all the time.
But the kind of conflict of interest we usually focus on – and the kind the Wikipedia article focuses on too – is organizational, economic, and secret. You’re supposed to act in the interest of one organization but you act instead in the interest of another; you do so for current or future financial gain; and nobody knows you’re getting paid off.
So what sorts of conflicts of interest – narrowly or broadly defined – might come up in the World Health Organization’s management of the swine flu pandemic?
We can think of four. The first two are what people usually mean when they charge someone else with a conflict of interest, or when they deny such a charge that has been made against themselves. The last two are the ones that happen most often, are least likely to become the focus of attention, and have the most impact.

Does WHO sell out to Big Pharma?
WHO’s core responsibility is to provide public health information and advice to the world’s governments and the world’s people. If its information and advice are potentially corrupted by unacknowledged financial considerations, that’s certainly a conflict of interest.
Does that happen? Of course it does, sometimes – as is the case in virtually any organization. But very, very rarely are the financial considerations of the World Health Organization focused on the pharmaceutical industry.
WHO gets most of its money and most of its personnel not from Big Pharma but from national governments, and to a much lesser extent from NGOs. Does WHO sometimes compromise what it says about a public health issue in order not to give offense to an important government like the U.S. or China? Sure. We could give dozens of examples from the public record, and any WHO official could give hundreds.
Some examples are tiny: A minor WHO program with which we were peripherally involved was canceled by a senior WHO official when a program participant irritated a senior official of an important country. Others are not so tiny: WHO periodically withholds news of local infectious disease outbreaks because the government where the outbreak is occurring is not yet willing to go public.
The very decision to declare H1N1 a pandemic was delayed by WHO for many weeks, largely in deference to several governments that wanted more time to develop their plans and forewarn their people. One of the big ironies of the “fake pandemic” issue is the charge that WHO declared the pandemic precipitously or unnecessarily in deference to Big Pharma, when in fact WHO dallied in deference to member states.
This delay didn’t matter much technically, because the recommended actions specified in the newly published pandemic phase definitions were the same for Phase 5 (declared on April 29, 2009) as for Phase 6 (declared on June 11, 2009). It’s hard to find examples of governments or businesses that took precautions after June 11 they were unwilling to take earlier because WHO hadn’t officially declared a full-fledged pandemic yet. Nonetheless, the delay served the interest of certain member states, not the immediate interest of international public health.
Note that “serving the interest of certain member states” does often serve the longer-term interest of international public health as well. When the stakes are not too high, as in this instance (because the recommended actions for Phases 5 and 6 were the same), WHO sometimes defers to member states so the member states will continue to support WHO and give it access, so WHO can continue to do its public health job.
We’re not talking about secret deposits in the Swiss bank accounts of WHO officials. Nonetheless, these are real conflicts of interest. One WHO public health interest (announcing early
 ) is influenced (“corrupted”) by a completely different WHO public health interest (maintaining good relations with particular member states).
) is influenced (“corrupted”) by a completely different WHO public health interest (maintaining good relations with particular member states).WHO has much less incentive to make such compromises in deference to Big Pharma. And it has much less natural inclination to do so. Everyone who knows WHO knows that, like most U.N. agencies, it tends to be left-leaning and anti-corporate (by American standards, anyway). WHO officials visibly grit their teeth when they have to ask Big Pharma for favors.
Once again, secret cash payoffs aren’t the issue. Few of WHO’s critics have insinuated anything nefarious about how WHO officials might have personally benefited from their alleged deference to Big Pharma. There have been some passing references to former WHO officials who moved on to pharmaceutical industry jobs. But that’s about it. Nobody is alleging kickbacks. This is not the U.N. oil-for-food scandal, in which some U.N. officials personally accepted bribes.
If WHO is selling out to Big Pharma, it must be doing it for the same reasons it “sells out” to member states: for the sake of some future public health goal.
That’s not an absurd possibility. WHO does sometimes ask Big Pharma for favors. It asks for price reductions on life-saving medicines, for example, and it asks for relaxed licensing restrictions so those medicines can be manufactured and sold more cheaply in developing countries. Is it conceivable that WHO might quietly make a (teeth-gritted) decision that helps a pharmaceutical company financially in one venue, in hopes of increasing that company’s willingness to make concessions valuable to public health in some other venue? Yes, it’s conceivable – though we know of no examples. We are confident it isn’t commonplace.
And it isn’t even conceivable with regard to the big pandemic decisions, like the decision in 2004 to urge countries to stockpile antiviral drugs, or the decision in 2009 to focus intensive effort on trying to produce and distribute large amounts of swine flu vaccine as quickly as possible. Those big decisions clearly benefited the companies that manufacture antivirals and vaccines. So, yes, WHO did have multiple interests: an interest in preparing the world to cope with future pandemics (2004 antiviral stockpiling guidelines) or emerging pandemics (2009 Emergency Committee recommendations) of unknown severity, and an interest in building and maintaining good relations with Big Pharma. But there was no conflict of interest. Both interests pointed in the same direction. And the former was obviously a lot more compelling than the latter.
To imagine WHO selling out to antiviral and vaccine manufacturers by supporting antiviral stockpiling and expanded vaccine production, you have to imagine that most experts not connected with the relevant companies thought the decisions were wrong, and that WHO consciously chose to ignore their advice in order to make money for the manufacturers of antivirals and vaccines. There is no publicly available evidence – none – that this was the case.
But part of the current problem is that there is also no publicly available evidence – yet – that this was not the case. Transcripts or detailed minutes of the relevant advisory committee meetings would go a long way toward settling the question.
There are certainly experts who now believe, in hindsight, that the antiviral stockpiles and the big vaccine ramp-up didn’t turn out all that useful. There may even be a few experts who believe in hindsight that this conclusion should have been deducible early on. But as far as we can tell, the vast majority of experts with or without Big Pharma connections agreed with the two decisions when they were made, and the vast majority continue to think they were the right decisions, given the uncertain pandemic future at the time when the decisions had to be made.
To believe that WHO sold out to Big Pharma, then, you must believe in a Big Conspiracy. You must believe that virtually all mainstream flu experts have ties to Big Pharma sufficient to corrupt their judgment and their behavior, even if their primary employers are government health agencies or universities or NGOs. You must believe that experts whose Big Pharma ties aren’t to the manufacturers of antivirals and flu vaccines would nonetheless join in the conspiracy, presumably in return for some future benefit for the companies with which they are connected. And you must believe that all of these experts, and WHO itself, doubted the public health wisdom of producing more antivirals and new flu vaccines, but consciously advocated the opposite view in order to enrich the manufacturers.
That’s more than we can believe.
But it is certainly understandable that the secrecy surrounding the identities and industry connections of WHO’s expert advisors – a non-issue in the public’s mind at the start of the pandemic – became a red flag as the pandemic progressed and WHO didn’t stand down from its initial characterization of its severity.

Are industry-connected advisors secretly paid as lobbyists and spies?
This too would be a clear-cut conflict of interest: WHO advisors getting money from industry that WHO knows nothing about, a secret payoff for handling the WHO meeting the way industry wants it handled.
It is certainly true that pharmaceutical industry employers encourage their people to agree to serve on WHO committees. And undoubtedly one reason they do so is because it adds value for the employer. Committee members can point things out that their employer wants to see pointed out – information about the uses and side-effects of various drugs, information about how long those drugs take (and how much they cost) to produce, etc. And committee members can learn things that their employer finds useful to know – information about the direction of WHO officials’ thinking, who’s on which side for what reasons, etc.
All of this is true not just of experts employed full-time in the pharmaceutical industry but also of experts whose ties to the industry are part-time. An industry consultant who sits on a couple of WHO committees is a more valuable consultant than one who doesn’t.
This doesn’t quite add up to “secretly paid.” Everyone who sits on a WHO committee, including WHO officials themselves, knows who the industry-connected committee members are, and can “consider the source” when assessing their contributions. Everyone knows industry-connected experts earn some money from industry, and those whose principal affiliation is industrial earn most of their money from industry. (Except for expenses, outside experts get no money at all from WHO for serving on its committees.) And everyone knows committee members are information conduits in both directions – carrying non-confidential information from company to committee to WHO and back again. So it’s not secret. And there’s unlikely to be extra industrial pay earmarked for this task – no bonus, not even time off, just another headachey job to squeeze into the schedule. Still, industry-connected advisors do sometimes function as lobbyists (telling WHO what the company wants them to say) and spies (telling the company what they learned from WHO).
So do university-connected advisors, but less so. And so do government-connected advisors – in spades. One of us (Jody) served on a WHO team that helped a developing country cope with the health aspects of an oil spill. Several of the other team members were seconded from the public health agency of a developed country with lots of oil spill experience. At the end of the mission, those members’ last visit was to their own country’s embassy, to brief embassy officials on the status of the spill and the spill response. Nobody thought that was nefarious. Everyone knows that government officials working with international agencies are going to keep their own governments informed.
And everyone knows that government representatives on international advisory committees are going to echo their governments’ policy preferences. Rarely does anyone say, “My government’s official policy is X, but personally I think Y.” They are, after all, their governments’ “representatives” on the committee. (But experts do sometimes find ways to signal their disagreement with their government’s policy, or they may casually say something to that effect during a coffee break.)
The fact that WHO advisory committee members carry information back and forth is a large part of their value – not just to their employers, but also to WHO. WHO needs to know what the pharmaceutical industry is thinking, and it needs the pharmaceutical industry to know what WHO is thinking. What committee members bring to the table is partly their wisdom as individuals and partly their capacity as conduits.
The conflict of interest arises, if it arises, when committee members represent as their individual opinions a viewpoint that is actually not what they think, but rather the preference of their industry (or government) associates. Or when they carry back to their industry (or government) associates information that has been identified as confidential and not to be shared. We assume these things do happen from time to time – especially with government-connected WHO advisors but sometimes, also, with industry-connected advisors.
Was lobbying/spying on behalf of Big Pharma a big problem with regard to WHO pandemic decision-making? Were there people on WHO’s Emergency Committee (or any other WHO committee) saying things they didn’t believe because that’s what their pharmaceutical industry contacts wanted them to say? Were there people reporting back to Big Pharma things that WHO didn’t want them to report? We can’t prove there weren’t … but it seems pretty unlikely.
Remember back when the pandemic was young, and the world’s governments were appropriately worried that it might be or become severe? Developed countries were desperate to order more antivirals and vaccine. Developing countries were even more desperate; they had no money to order antivirals and vaccine, but they wanted some anyway. Manufacturers were having no trouble selling as much as they could produce. They were triaging customers, trying to cope with the outrage of governments that thought their orders weren’t getting the priority they deserved.
Under those conditions, does anyone really think the pressure on WHO came mainly from companies keen to increase their sales, not from governments keen to increase their access?

-
Do industry-connected advisors unconsciously reflect industry perspectives?
Critics of WHO pandemic decision-making seldom actually claim in so many words that industry-connected WHO advisors are secretly paid as lobbyists and spies.
What they claim is simply that the advisors have industry connections. This, they rightly point out, is a structural conflict of interest. The advisors are trying to serve two masters (or more than two): the companies from which they derive income and the international agency to which they are giving advice. The critics can’t prove that the advisors’ conflict of interest actually affected the advice they gave, nor do they feel any obligation to prove that, although they like to insinuate it. They make two assertions, both of them true:
- Specific members of WHO advisory committees have ties to Big Pharma, ties that WHO does not routinely acknowledge publicly.
- Specific committee recommendations accepted by WHO end up benefiting Big Pharma.
The link between the two assertions is left for the public to fill in. And what the public presumably imagines is advisory committee members who intentionally give WHO bad advice in order to enrich the pharmaceutical industry – and WHO officials who either are duped into accepting the bad advice because they don’t know any better or intentionally accept the bad advice for the same reason it was given in the first place: to enrich the pharmaceutical industry.
But a huge body of theory and research tells us that intentional bias is the tip of the conflict-of-interest iceberg. The big problem with serving two masters – with structural conflict of interest – isn’t that people consciously betray one master for the sake of the other. It is that people unconsciously confuse, merge, or compromise the interests of both.
Like everyone else’s opinions, the opinions of experts are significantly influenced, unconsciously, by the opinions of those on whom the experts are economically dependent.
A 2009 book on Conflict of Interest in Medical Research, Education, and Practice devotes an appendix to an essay by Jason Dana on “How Psychological Research Can Inform Policies for Dealing with Conflicts of Interest in Medicine.” Dana writes:
This research shows that when individuals stand to gain by reaching a particular conclusion, they tend to unconsciously and unintentionally weigh evidence in a biased fashion that favors that conclusion. Furthermore, the process of weighing evidence can happen beneath the individual’s level of awareness, such that a biased individual will sincerely claim objectivity. Application of this research to medical conflicts of interest suggests that physicians who strive to maintain objectivity and policy makers who seek to limit the negative effects of physician-industry interaction face a number of challenges. This research explains how even well-intentioned individuals can succumb to conflicts of interest and why the effects of conflicts of interest are so insidious and difficult to combat.
One of the best-established findings in the social science of science is the very strong correlation between the preferences of a study’s funder and the findings of the study. (See for example this slideshow
 by Sheldon Krimsky, one of the leading researchers on scientific conflict of interest in the biomedical field.) The vast majority of studies, especially on controversial topics, reach conclusions their funders find acceptable. This is not chiefly because the researchers are consciously dishonest. Rather, it is because of the subjectivity of all research – what we sometimes call “the Ouija board heuristic.” Researchers, like most people, unconsciously absorb and try to satisfy the expectations of the people they work for. Those expectations influence how research problems are framed, how methodological options are resolved, how uncertain results are interpreted, and how decisions to publish or not publish are made. (Of course funders also tend to choose researchers who share their predilections in the first place.)
by Sheldon Krimsky, one of the leading researchers on scientific conflict of interest in the biomedical field.) The vast majority of studies, especially on controversial topics, reach conclusions their funders find acceptable. This is not chiefly because the researchers are consciously dishonest. Rather, it is because of the subjectivity of all research – what we sometimes call “the Ouija board heuristic.” Researchers, like most people, unconsciously absorb and try to satisfy the expectations of the people they work for. Those expectations influence how research problems are framed, how methodological options are resolved, how uncertain results are interpreted, and how decisions to publish or not publish are made. (Of course funders also tend to choose researchers who share their predilections in the first place.) This unconscious influence is all the more powerful precisely because it is unconscious. Research consistently finds that most experts are supremely confident that their expert opinions are their own, influenced only by the evidence and not by contagion – not by other experts’ opinions and certainly not by the opinions of their funding sources.
Experts have learned over the years that conflict of interest is a serious issue. They know they’re supposed to acknowledge conflicts (especially financial conflicts) when they report research results … and when they sit on advisory committees. They know they can get into trouble if a conflict emerges later that they neglected to mention. So they usually take the reporting burden seriously.
But they don’t take the issue seriously. They know their conflicts of interest are only “potential conflicts,” not actual conflicts. They know their expert opinions haven’t been corrupted. Other experts, perhaps, may be unduly influenced. But no one they work with. And certainly not themselves.
Their self-confidence exacerbates the corruption. You can’t really be on guard against a conflict of interest if you are certain it poses no danger.
This is analogous to the conviction of physicians that they are not influenced by gifts from drug salespeople. A 2003 review of this phenomenon
 by scholars at the University of Pennsylvania concluded:
by scholars at the University of Pennsylvania concluded:In fact, researchers have found that the more gifts a physician receives, the more likely he or she is to believe that they do not influence behavior (Hodges 1995). While medical professionals might believe themselves to be “more rational and critical” than the average person (Shaughnessy, Slawson, and Bennet 1994; Babcock and Loewenstein 1997), the success of pharmaceutical marketing illustrates that physicians are as susceptible to target marketing as others (Coste 1999). Those who do not acknowledge the power of small gifts are the ones most likely to be influenced, because their defenses are down.
When ordinary citizens hear about charges of conflict of interest, they usually imagine intentional wrongdoing – our first two categories. But conflict-of-interest experts worry far more about unintentional wrongdoing: the universal human tendency to adopt opinions congenial to those on whom you are economically dependent … without realizing that you are doing so.
Of course this unconscious tendency is far broader than that. The opinions of some WHO advisory committee members are undoubtedly influenced, unconsciously, by the opinions of the pharmaceutical company officials for whom they have done work. Their opinions are undoubtedly influenced also by the opinions of their non-industrial friends and colleagues: other experts they spend time with on the job and at professional conferences, other members of the WHO advisory committee on which they serve, etc.
Unconscious conflict of interest is arguably most pernicious when it involves money rather than, say, friendship. But wherever the influence comes from – and it comes from everywhere – the key point is this: People’s stated opinions are more affected by unconscious bias than by conscious misrepresentation.

-
Do advisors who covet industry connections tend to say things industry will like hearing?
Imagine a WHO advisory committee member with no conflicts of interest – no financial or non-financial relationships capable of influencing (“corrupting”) his or her advice. Imagine that in spite of this stunning absence of connectedness, the advisory committee member is a genuine expert; he or she has somehow managed to acquire relevant knowledge without forging any links.
The ideal committee member, right? Well, not unless he or she is happy to remain unconnected.
Sometimes (we don’t know how often) people express opinions that are neither their own opinions nor the opinions of their peers and funders. Sometimes they are the opinions they think will please the people they would like to be their peers and funders in the future. Sucking up plays a role in at least some advisory committee meetings.
Sucking up takes three main forms:
- Saying things you think the people you want to impress will find impressive and useful.
- Saying things you think the people you want to impress will find flattering and gratifying (this can include pretending to agree with them).
- Not saying things you think the people you want to impress might find offensive.
All three of these behaviors are likely to conflict with your agreement to give the committee your best advice. (Number one might be okay, if the people you want to impress are the same people who gave the committee its mandate.)
This kind of conflict of interest is least often mentioned. And we have the least to say about it. But we do want to say two things.
First, sucking up is impervious to conflict-of-interest paperwork. No matter how thoroughly committee members are required to confess their structural ties to industry, nothing on the forms asks them to confess their desire to build such ties in years to come. We suppose it would be possible to add an item to that effect. “True or False: I hate those bastards and wouldn’t work for them if they asked.”
Second, sucking up applies to all prospective ties – to industry, to government, to activist groups, to academia, even to WHO itself. “If I do a good job on this committee, maybe WHO will put me on a more prestigious committee next time.” But it might have comparatively less influence on prospective industry ties. As a financial matter, industry tends to be more willing than government or activist groups to work with people with opposing views. (Some see this as openness; some see it as cooptation.) And as a psychological matter, industry tends to be less thin-skinned than government or activist groups, less likely to be turned off by people who fail some ideological litmus test. A canny would-be industry consultant demonstrates how potentially valuable his or her opinions are, not how faithful they are to the Big Pharma party line.
Insofar as a WHO advisory committee member is sucking up to Big Pharma, he is likely to feel fairly free to speak his mind – which will serve WHO’s interests just fine. If she’s sucking up to government or other interest groups, she is likely to mind her tongue – which will serve WHO’s interests less well.
The main point to remember about sucking up is that it isn’t revealed or monitored by even the most transparent conflict-of-interest policy.
So here is WHO’s conflict-of-interest situation in a nutshell:
- WHO now needs to be more transparent about the conflicts of interest of its advisory committee members … and about their names. When mistrust is high, the demand for transparency is justifiably greater than when mistrust is low. (You should aim for transparency even when mistrust is low, but you will have to become more transparent still when mistrust is high.) Thanks to its mishandling of the “mildness” and “definition of a pandemic” controversies, mistrust of WHO is now high.
- It will be hard to be transparent about all the granular detail contained in WHO Declarations of Interest without seriously reducing many experts’ willingness to help. But a vague summary or a few selected examples won’t begin to rescue WHO’s credibility. Finding a compromise will be a challenge. But WHO isn’t the first, and it can learn from how other organizations have faced similar transparency challenges.
- Transparency aside, WHO also needs to develop more stringent conflict-of-interest requirements. Here again it will be following in the footsteps of other organizations – medical journals and government advisory committees, for example – that have ratcheted up their standards in response to pressure motivated by increased mistrust.
- None of these improvements will have much impact on the kinds of conflict of interest most likely to distort advice WHO actually gets from its advisory committees: first and foremost, the mostly unconscious tendency to absorb the views of others – whether funders or peers – as one’s own; and secondarily, the mostly conscious tendency to say things that will appeal to those whose good opinion one values.
- WHO should try to remember that the recent controversy over conflict of interest, and transparency about conflict of interest, is just a symptom. This controversy is a reflection of WHO’s credibility problem, not its source. The source of the credibility problem is twofold:
- WHO’s recalcitrance about acknowledging that the H1N1 pandemic has been mild so far (and is nearly gone for the moment); and
- WHO’s disingenuousness about having “changed the definition of a pandemic” and its claim that severity was “never” part of the definition/description of a [flu] pandemic.
- Nothing WHO says or does about conflict of interest will help it regain ground as much as conceding that it was wrong to keep calling the swine flu pandemic “moderate” while the world experienced it as mild (especially since WHO has called the first waves of three other flu pandemics “mild”), and wrong to keep pretending that severity was “never” part of the WHO definition/description of a [flu] pandemic.
Consider the credibility problems of another organization, one in considerably worse shape than the World Health Organization: BP. Because trust in BP is now so low, the company desperately needs to be able to prove what it says. For example, it needs third-party advisors with anti-corporate credentials who will eventually be able to tell the world (if and when it becomes true) that less oil than previously is gushing from the ocean floor. Such claims directly from BP spokespeople would lack credibility precisely because those spokespeople have an obvious conflict of interest, and have low-balled the amount of leaking oil from the start. BP would be wise to rely more on outside expert advisors.
And it should expect to have to answer tough questions about those advisors’ conflicts of interest. It certainly won’t be able to reassure the public that it has checked out their conflicts of interest and found them to be satisfactory, as WHO tried to do on December 3, 2009.
But relying on credible outside advisors isn’t BP’s main risk communication job. What it needs most is to begin the process of rebuilding its own credibility. It needs to demonstrate, credibly, its compassion for those it has hurt; its contrition (indeed, its shame) for what it did and what it failed to do; and its determination to make things right.
WHO has not perpetrated an environmental catastrophe. To the contrary, its main offense is failing to stand down its warnings when a possible public health catastrophe began to look far from catastrophic. Resuscitating BP’s credibility may not be feasible, and may not even be desirable. Resuscitating WHO’s credibility is both feasible and desirable. That task will, however, require WHO to back off two entrenched positions: that the swine flu pandemic isn’t mild so far (by historical standards), and that WHO didn’t do anything funny with its flu pandemic definitions. Along the way, it will help some if WHO also makes improvements in how it handles conflict-of-interest concerns about its advisory committees.
Copyright © 2010 by Peter M. Sandman and Jody Lanard
