Foreword
![]() This “Foreword” is really an “Afterword.” A week or so after my October 5, 2016 presentation, my host and friend, CIDRAP Director and University of Minnesota Professor Michael Osterholm, shared some reactions with me. These are my reactions to his reactions.
This “Foreword” is really an “Afterword.” A week or so after my October 5, 2016 presentation, my host and friend, CIDRAP Director and University of Minnesota Professor Michael Osterholm, shared some reactions with me. These are my reactions to his reactions.
In part, Mike thought I threw around words like “dishonest” and even “liar” too readily. Even though I acknowledged that many public health professionals are themselves misled and innocently conveying false information; even though I acknowledged that those who know they’re conveying false information tend to see themselves as simplifying rather than misleading; even though I acknowledged that their motives are often altruistic – despite all that I came across as damning the profession with too broad a brush.
Column Table of Contents
I think Mike is right. My notes aren’t angry, but at times my actual presentation was angrier than I meant it to be. There’s a real difference in tone between telling an audience that “X and Y aren’t true, and public health professionals who know they’re not true should stop saying them” and “If you say X and Y knowing they’re not true, you’re a liar.” I veered too often from the former to the latter. And sometimes I veered further, claiming that anyone who says X and Y is a liar, neglecting to restate the point that public health professionals are often innocently repeating misinformation they have learned from their leaders.
More fundamentally, Mike felt that my indictment of public health dishonesty failed to distinguish what he called “felonies” from mere “misdemeanors.” As we talked, the typology that emerged looked something like this:
- Sometimes the dishonesty is systemic, genuinely misleading people in ways that have real impact on their health-related decisions. Mike’s example – not one of the four I focused on in my presentation – was the widespread excessive claims about flu vaccine efficacy. He also seemed to agree with me about how public health professionals responded to the various Zika funding bills.
- Sometimes the dishonesty is genuinely dishonest, but it’s an isolated exception, not part of a broader pattern. Mike agreed with me that it was dishonest of the polio eradication campaign to cover up the fact that the oral polio vaccine occasionally gives people polio, for example, but he thought in most ways the polio eradication campaign was honest. And even this isolated dishonesty wasn’t truly misleading in his judgment, since the oral polio vaccine is far safer than going unvaccinated in places where there is a current risk of polio.
- Sometimes what I see as dishonesty Mike sees as more a matter of overconfidence – failing to acknowledge uncertainty sufficiently. With regard to Ebola quarantine, for example, Mike said public health professionals had a strong case that quarantining returning volunteers was unnecessary, but he agreed that the case against quarantine was often overstated. He added that there were other aspects of Ebola communication he considered better examples of systemic dishonesty: whether U.S. hospitals could safely manage Ebola patients without special training and equipment; whether airport fever screening was a useful Ebola precaution; whether modeling could accurately predict the size of the West African epidemic; etc.
- Sometimes what I see as dishonesty Mike sees as a benign decision to leave out technical details that the public doesn’t need to know. He put in this category my objections to the way the measles-mumps-rubella (MMR) shot is typically described to patients and the public. Combining the three vaccines into one shot is sensible and harmless, Mike said; individual shots are unavailable and unneeded. There is therefore no reason why doctors should feel obliged to point out, before administering the recommended second MMR, that no vaccinee needs that second rubella dose and most don’t need the second measles dose either. He said it’s not reasonable to demand total transparency about information that doesn’t affect anybody’s health.
Implicit in my presentation is a very different typology:
- Altruistic dishonesty (like hiding the rare bad outcome of polio vaccination so parents wouldn’t unwisely refuse to let their children be vaccinated).
- Self-serving dishonesty (like delaying the second MMR for logistical reasons while telling parents that any vaccine delay endangers their child).
- Political dishonesty (like urgently demanding Zika funding as a public health necessity while failing to support a Zika funding bill that included a mostly symbolic “poison pill” denying Planned Parenthood access to the new money).
My typology focuses on motives. Mike’s focuses more on health impacts.
In terms of my hazard-versus-outrage distinction, Mike seems to be saying that it’s a felony for public health to mislead the public about the size of the hazard. But if people aren’t misled about the hazard, then even genuinely dishonest messages are mere misdemeanors. And if the hazard is uncertain, deciding to sound more confident than the science justifies may be suboptimal but it isn’t really dishonest. Finally, withholding extraneous details because they might be misleadingly alarming isn’t dishonest at all; it’s sensible.
The distinctions Mike is making are obviously important, and my presentation would have been stronger if I had discussed them. But I think Mike’s typology pays too little attention to outrage and its health implications.
Consider the MMR vaccination. Of my four examples of public health dishonesty, that’s the one Mike found least convincing.
I imagine myself in the shoes of a parent who is already skeptical about all those childhood vaccinations. The pediatrician and CDC insist, rightly (in my judgment), that the parent’s skepticism is unwarranted – that the vaccines are safe. They also insist, falsely, that it’s unconscionably dangerous for the parent to delay any vaccine in the recommended schedule because every dose in the schedule is essential to the child’s health. Then the parent goes online – not just to anti-vaccination websites but also to the granular detail published (but not publicized) by vaccination proponents. And there the parent learns that some vaccine doses are completely unnecessary, that for some vaccinations the risk of delay is minuscule, and that the officially recommended vaccination schedule includes delays of its own that are built in for purely logistical reasons.
Can you blame such a parent for concluding that the public health profession is not to be trusted? And then the dynamics of outrage come into play. Dishonesty arouses outrage, and outrage increases hazard perception. So the parent reasons from the true observation that she has been misinformed about some aspects of the MMR to the false conclusion that the MMR is dangerous.
I don’t know how many actual parents fit my paradigm. As I point out in the presentation, public health dishonesty doesn’t seem to be leading – not yet, anyway – to the credibility collapse that my theory says should result … and that in my heart of hearts I think the public health profession deserves.
And there’s the core question. Mike’s felonies are obviously felonies: misguiding people’s health decisions by feeding them misinformation. They’re hazard felonies. But what about outrage felonies? What about feeding people misinformation that doesn’t misguide their health decisions – until they learn that they have been misled, conclude that public health cannot be trusted and that what public health is recommending must be dangerous, and make horribly misguided health decisions as a result?
Mike is worried about misinformation that misleads people who believe it. I’m worried about that too. But I am just as worried about misinformation that misleads people precisely because they learn that they were wrong to believe it, and wrong to trust the public health profession that asserted it.
Neither typology, I think – and Mike agrees – captures the complexity of what I simplistically call “public health dishonesty.” Among the variables that a more thorough typology would need to consider:
- How false is the dishonesty – flat-out lies versus misleading half-truths versus incomplete/oversimplified/one-sided truths.
- How big is the dishonesty – big-picture falsehoods versus false or misleading details.
- How intentional is the dishonesty – fully conscious deception versus self-deception versus innocent ignorance.
- How pro-social are the motives for the dishonesty – self-serving motives versus ego-driven motives versus ideological/political motives versus altruistic motives.
- How emotionally loaded is the dishonesty – the extent to which the topic is high-salience and emotionally difficult for the audience.
- How systemic is the dishonesty – the extent to which public health is “speaking with one voice” and the voice is false.
- How consequential is the dishonesty – the extent to which people are basing decisions on it.
- How beneficial or harmful to public health is the dishonesty – the extent to which it has a bottom-line positive or negative effect on people’s health.
- How outrage-provoking is the dishonesty – the likelihood that people will find out; the likelihood that they will be outraged if they do.
None of this is laid out in my presentation, or in the notes that follow. I am grateful to Mike for both his good thinking and the thinking he provoked.
Introduction: Corporate Dishonesty and Disrespect Lead to Public Outrage
1. A preliminary comment: Despite Mike’s lovely introduction, he is not responsible for how I’m using my spot on this program. Some of you, I suspect, will disagree with my basic point. Many of you will disagree with some of my specific examples. In other words, as the boilerplate goes, “the opinions in this presentation are not necessarily those of our sponsor.” ’Nuff said.
2. I spent a lot of my career over the past 40+ years helping corporations prevent and manage what I termed “stakeholder outrage,” especially vis-à-vis risks and risk controversies. A basic principle of my work was that people get outraged when they know they’ve been lied to. It doesn’t have to be an outright lie; carefully cherry-picking information to give an intentional misimpression is seen by most people, lawyers excepted, as pretty much the same thing as lying. And most people don’t need proof the company intentionally misled them. It’s enough to suspect that the company did it, or even just sense that the company did it. Companies that are less than candid with their stakeholders, in short, end up with outraged stakeholders.
3. More often than not, my corporate clients’ dishonesty toward their stakeholders was accompanied by some kind of contempt, disdain, patronizing absence of respect. That, of course, exacerbated the outrage.
4. “So what?” my clients often asked. “What harm does it do us that we’re often dishonest and disrespectful?” Even back in the 1970s, when I started this work, my answer was that outraging your stakeholders means undermining your corporate reputation. It means there are more people who don’t like you, don’t trust you, don’t want to listen to you or do business with you, and therefore (among other things) don’t want your facility in their neighborhoods. As the decades passed, the magnitude of this reputational impact of stakeholder outrage grew – thanks to a wide range of factors, from the internet and social media to the socially responsible investment community to freedom-of-information laws. It became ever-truer that misleading stakeholders is bad for business.
5. One specific risk communication outcome of high outrage is high perceived hazard, irrespective of the actual hazard. That is, in any risk controversy – the emissions of an industrial facility, for example – there’s a strong causal link between how outraged people are at your organization and how dangerous they believe your organization’s activities to be.
6. So:
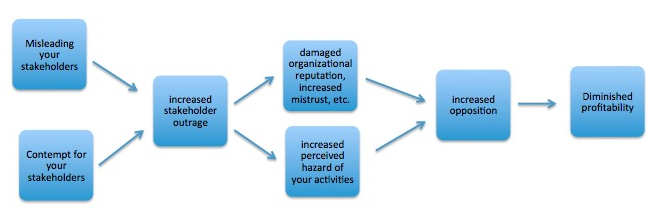
7. This set of relationships gave me a rationale that didn’t lean on ethics to urge my corporate clients to become more candid and less disdainful. It was a Sisyphean task. I had some success some of the time convincing some of my clients to reform some of their behavior. I’m pretty sure the net effect was an improvement, even if it was a smaller and more transient improvement than I liked to suppose. And it earned me a good income as a high-priced corporate consultant, telling companies to treat their stakeholders with more integrity and more respect for the sake of their own bottom lines.
Public Health May Be Different
![]() 8. Parallel to my work with corporations, I was also working with non-profits – initially with environmental activist groups and public health NGOs like the American Cancer Society; starting a little later with environmental and public health government agencies as well.
8. Parallel to my work with corporations, I was also working with non-profits – initially with environmental activist groups and public health NGOs like the American Cancer Society; starting a little later with environmental and public health government agencies as well.
9. It didn’t take me long to learn that my public-interest and government agency clients were at least as dishonest and contemptuous vis-à-vis their stakeholders as my corporate clients.
9.1 The main thrust of my presentation today will be to try to convince you that that is true, especially with regard to public health professionals and infectious diseases. I will focus mostly on dishonesty – intentionally misleading stakeholders and publics about public health – though along the way I’ll have some things to say about disrespect for the public as well.
9.2 I don’t have anything like quantitative proof – no methodologically sound tally of how often CDC, say, tells untruths to the public – compared to how often ExxonMobil or 3M commits the same sin. What I do have is a virtually endless supply of examples, from which I have selected a sample that I thought you might find both surprising and convincing. In the language of epidemiology, my evidence of public health dishonesty about infectious diseases is anecdotal only.
- The oral polio vaccine (see also this 2012 discussion)
- The measles-mumps-rubella vaccine (see also this 2011 discussion)
- Ebola quarantine (see also this 2014 discussion)
- Zika funding (see also this June 2016 discussion, especially endnote 14)
9.4 The lesson for you as consumers of public health information: Stay skeptical, even when there seems to be a consensus of the entire public health leadership. Decide for yourself what to believe. Look at the data, not just the leadership’s conclusions. Don’t give the public health Guild your proxy.
9.5 The lesson for you as providers of public health information: Decide how complicit you want to be. Will you push for candor, both in your organization and in public health itself? Or do you accept that the dishonesty and disrespect manifested by public health are sufficiently benign that you are willing to go along rather than risk being branded an iconoclast?
An example for those of you in the healthcare industry: Will you continue telling employees that you’re requiring them to get flu shots in order to protect patient health, even though you know the evidence is extremely weak (except in long-term care facilities) that healthcare worker flu vaccination benefits patients? (See “Flu Vaccination of Healthcare Workers: Two Risk Communication Issues” and “Convincing Health Care Workers to Get a Flu Shot … Without the Hype.”)
On its webpage supporting flu vaccination for health care workers, CDC cites only one reference as evidence of patient benefit, a meta-analysis that looked at eight studies. Seven of the eight were conducted in long-term care or nursing home facilities. Only one study was in an acute care hospital setting, and that study was observational. The meta-analysis authors graded the overall evidence quality of the eight studies as “moderate,” but they graded the quality of the observational studies (including the only acute care hospital study) as “low.”
10. If you want more detail or evidence/citations re any of my examples, or if you want different examples, or if you want to tell me some of your own examples, I’ll be here till your dinner. Or email me! You can also find more examples, and more detail on some of these, on my website.
11. I have routinely told my nonprofit and government public health clients exactly the same thing I was telling my corporate clients: that dishonest and disrespectful treatment of stakeholders was doing serious damage to their ability to achieve their public health missions. It took me an embarrassingly long time to begin to wonder if that was actually true, when it came to “Do Gooder” clients. I have come to doubt that it is true. For a variety of reasons, it now seems to me, the public tends not to notice these misbehaviors in public health organizations; and if it notices them it tends to forgive them. Among the factors here:
- We rightly see these organizations as altruistic; they’re trying to help us, not fleece us. That makes us both less suspicious and more forgiving.
- We depend on these organizations for help in ways that we don’t depend (or don’t realize we depend) on profit-making corporations. Especially in a crisis, we don’t want to know that the organizations we hope will protect us are not leveling with us or not treating us with respect.
- The media similarly cut slack for public health organizations in ways that they don’t for corporations. Exposing corporate misbehavior is a good way to win journalism prizes and advance in your career. Exposing public health agency misbehavior is a far less promising path to glory. There are exceptions, such as Alison Young of USA Today. But they are exceptions.
- Anti-corporate activist groups are widely considered to serve the public interest by exposing and thereby discouraging corporate misbehavior. Activist groups that oppose public health organizations (anti-vaccination groups, for example), are fewer in number and lower in stature, seen as the fringe rather than the mainstream. Anti-corporate groups’ frequent exaggerations are either taken seriously or shrugged off without undermining the rest of their message, while anti-vax groups’ exaggerations (for example) are seen as evidence that nothing those groups have to say is worth hearing.
12. In short, I can build a strong case that corporations that mislead and disrespect their stakeholders will be crucified, sooner rather than later. About the most I can say about public health agencies and organizations that mislead and disrespect their stakeholders is that I think eventually their misbehavior will catch up with them and undermine their credibility and effectiveness. I have very little evidence that this has happened so far.
Three Reasons for Public Health Dishonesty – and the Oral Polio Vaccine Example
![]() 13. One of the main reasons public health people persist in their dishonesty, I assume, is that it works. It usually isn’t caught and rarely incurs any meaningful punishment. That’s the first of three reasons why my public health clients have typically been less honest than my corporate clients. There are two other reasons worth discussing.
13. One of the main reasons public health people persist in their dishonesty, I assume, is that it works. It usually isn’t caught and rarely incurs any meaningful punishment. That’s the first of three reasons why my public health clients have typically been less honest than my corporate clients. There are two other reasons worth discussing.
14. Reason #2: My public health clients are trying to do good in the world, and sometimes they come across situations where it feels like candor could undermine their public health goal. So they mislead instead. In other words, public health dishonesty is quite often motivated by altruism. The oral polio vaccine (OPV) is a good example.
14.1 As most of you know, there are two polio vaccines; one’s a shot and the other is delivered orally. The oral vaccine is a live, weakened vaccine. It is significantly less safe than the injected (dead) vaccine, and it’s now illegal in most developed countries. But an OPV polio campaign is significantly less expensive than an IPV polio campaign. OPV has another advantage that until recently made it the vaccine of choice for developing countries: The vaccine virus sheds in the stool of vaccinated children and spreads via the stool to unvaccinated or unsuccessfully vaccinated children – without their knowledge or consent – giving them protection against polio too.
14.2 But about one vaccinee in a million gets polio from the oral vaccine itself (VAPP – vaccine-associated paralytic polio). And from time to time the virus reverts to a more virulent form, causing a polio outbreak (VDPV – vaccine-derived paralytic polio) in children who were not directly vaccinated.
14.3 Throughout the decades when OPV was the backbone of the polio eradication campaign, campaigners routinely hid the fact that the OPV can give you polio.
14.4 Starting in 2005, for example, Nigeria experienced the largest VDPV outbreak on record – hundreds of cases. It was duly reported to the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention. But health authorities tried to cover it up in Nigeria. After the cover-up was revealed in late 2007, WHO’s top polio official at the time, David Heymann, defended the cover-up, saying the outbreak was an “operational” issue, so there was no need to inform anyone outside the scientific community.
14.5 Why were the authorities reluctant to say anything? Religious leaders in parts of some Muslim countries, including Nigeria, have opposed the polio eradication program. They have claimed, among other things, that the program is a western genocidal plot. The polio risk from the oral vaccine is the germ of truth in that false belief, although of course the vaccine prevents orders of magnitude more polio than it causes.
14.6 Authorities feared that acknowledging the Nigerian VDPV outbreak would give credence to the claims of anti-vaccine imams. When I consulted on this issue, I suggested the opposite effect: that trying to suppress news of the outbreak would ultimately make the claims of the anti-vax imams more credible … especially the claim that you can’t trust what the polio eradication campaign tells you about the safety of the polio vaccine. My clients disagreed and continued their explicit policy of covering up both VAPP and VDPV.
There are 2,000 children who die each day in Indonesia and it is natural that when you are immunising, some of those children who would die normally would die.
That is literally true. It is carefully worded so as not to constitute an outright lie. But Dr. Heymann was explicitly trying to convince Indonesian parents that VAPP didn’t exist – that OPV can’t give you polio and sometimes kill you. He was telling one truth in order to steer the Indonesian public away from a different truth: When millions of children are vaccinated with OPV, a few of them are going to catch polio from the vaccine and some may die as a result.
This vaccine is safe and has no side effects.
Trainers were also taught to teach vaccinators how to answer parents’ questions about oral polio vaccine safety. A 2011 “Training Manual for National/Regional Supervisors and Monitors” (apparently developed for a national polio vaccination program in Yemen) instructs readers: “You should memorize the following Questions and Answers.” Here is #8, in its entirety. This is what trainees were to memorize to tell any parent who asked:
Question
Are there side effects from the vaccine?Answer No, there are no side effects. Experience shows that if children develop diseases or symptoms after vaccination, it is a mere coincidence. They would have developed these diseases anyway, with or without vaccination.
This manual was still online when I checked on September 24, 2016.
14.9 Polio eradication campaign officials were convinced this dishonesty was saving lives by protecting the credibility of the vaccination campaign. In the short term, they were probably right. In the long term, I believed it was costing lives by undermining the credibility of the international polio eradication campaign … and of public health itself. But I couldn’t prove it – and I’m no longer convinced it’s so. The dishonesty is documented; its impact is speculative.
14.10 This is perhaps the most defensible kind of public health dishonesty: altruistic dishonesty, sacrificing the integrity and perhaps the long-term credibility of public health in order to save lives in the short term. As we shall see, it is by no means confined to developing countries.
15. My first reason why public health professionals are often dishonest is simply because it works – they don’t usually suffer any consequences. My second reason is altruism.
Reason #3 is related to what I’m calling altruistic dishonesty, but it’s different, and I want to advance it more tentatively: Because my public health clients are genuine altruists, because they are doing good in the world, I think they feel more entitled to be dishonest … even when the particular dishonesty is more self-serving than altruistic. Even my corporate clients often feel virtuous, believing that they are doing well by doing good. But at least they are in fact doing well. By contrast, my public health clients often feel – not always, by any means, but often – like they have made a considerable personal sacrifice in terms of income, stress, working conditions, etc. in order to do good in the world. So they tend to get a little bit entitled, a little bit of a chip on their shoulder. Among other things, they’re less thoughtful in their dealings with consultants like me, and less receptive to criticism. But I think they’re also less honest and respectful in their dealings with stakeholders.
Public Health Dishonesty Is Half-Conscious
![]() 16. It is important to say that the dishonesty of public health organizations and practitioners typically is not entirely conscious. They don’t twirl their moustaches and tie maidens to railroad tracks. They don’t say to themselves: “Now we’re going to mislead the public. We know we’re doing it. We know why. We’ve decided integrity matters less than the outcome we have in mind.” I think that kind of self-aware dishonesty is comparatively rare.
16. It is important to say that the dishonesty of public health organizations and practitioners typically is not entirely conscious. They don’t twirl their moustaches and tie maidens to railroad tracks. They don’t say to themselves: “Now we’re going to mislead the public. We know we’re doing it. We know why. We’ve decided integrity matters less than the outcome we have in mind.” I think that kind of self-aware dishonesty is comparatively rare.
17. On the other hand, public health dishonesty is not entirely unconscious either. Somewhere in the middle realm between deception and self-deception is a place where we don’t feel we’re being dishonest because we’re not focusing on the truth we’re hiding. If you catechized us or cross-examined us on the facts of the situation, yes, we do know that X and Y are true, and we do know that what we said gave the impression that X and Y are false … but no, we weren’t intentionally deceiving anyone.
18. Until 2011, the CDC routinely claimed that the flu vaccine was 70–90% effective. When CIDRAP was documenting that this was a wildly optimistic claim, Mike and I had many debates about whether CDC, ACIP, and the rest of the flu vaccine leadership were misjudging the data or intentionally misrepresenting the data.
I think the truth was somewhere in the middle. When they put their minds to it, they sort-of knew that 70–90% was too high even for healthy young adults in a year with a good match … and way too high for people my age and older in a year when the match was suboptimal. But when they said 70–90%, full stop, they mostly imagined that they were simplifying the science, not misstating the science. I call this “misoversimplification.” And they almost surely thought that claiming high vaccine efficacy was a crucial path to achieving high vaccine uptake.
Almost singlehandedly, CIDRAP forced them to change their efficacy claims. Interestingly, flu vaccine uptake did not collapse as a result.
They’ve come only partway. They now typically claim 50–60% flu vaccine efficacy, still an overstatement when stated globally without the qualifier, “in healthy, young adults in a year with a good match.” (Not to mention recent research suggesting that repeated annual flu vaccinations may actually lead to diminished immunity.) And they still don’t feel dishonest when they say it, even though they know it’s an overstatement of the sort that they would never make in a professional context.
19. In 2008 I gave a day-long seminar on “Managing Vaccination Controversies … and Trying Harder Not to Provoke Them” for the CDC’s National Center for Immunization and Respiratory Diseases. I focused largely on a list of less-than-honest messages promulgated by vaccination proponents – including some in my presentation today. My main purpose was to make a case that vaccination dishonesty, which I consider well-intentioned on behalf of a cause I share, was ultimately self-defeating because it undermines the credibility of public health in general and vaccination in particular – a thesis I’m no longer certain I believe. (I wish it were true. I’m just not sure it is. Public health mostly gets away with its dishonesty, at least so far.)
20. But in order to argue that public health dishonesty is self-defeating, I first had to convince my CDC audience that it is commonplace. Hence my long list of examples. As I went on and on, it became vividly clear to me that my audience was being split into two roughly equal groups. About half were wryly nodding their heads, silently acknowledging that, “Yes, we do that.” The other half were emphatically shaking their heads, silently insisting that, “No, we certainly don’t do that!” Everyone in the room was, in my judgment, a perpetrator – willing to tell half-truths and even untruths in the interests of promoting vaccination. In the very safe environment of a CDC lecture hall, half were able to see it and acknowledge it, at least in the moment. The other half weren’t.
21. It is also important to bear in mind that I’m really talking about the dishonesty of public health leaders – people in authority and people with specialized expertise. Lower-ranking and less-specialized public health professionals – most state and local public health officials, for example, not to mention clinicians – are better seen as the victims than as the perpetrators. They follow the lead of CDC, WHO, ASTHO, various professional societies, and renowned experts. Even if they disagree, they know it would be professionally risky to voice their objections, and almost unheard of to voice them publicly. But they don’t usually feel they know enough to disagree. Even when the Guild dogma strikes them as “off” in some way, they usually figure the people in charge must know something they don’t know.
22. In the United States, public health is highly decentralized in principle. But in day-to-day practice, it’s a Guild. A very small cadre of leaders “recommend” policies and procedures that are then almost universally – and almost religiously – adhered to.
During the H1N1 pandemic of 2009–2010, for example, CDC’s public statements about what age groups were likeliest to die if they caught the disease diverged systematically and intentionally from CDC’s own published mortality data. Whenever I pointed out the discrepancy to state or local health officials, their first response was to doubt my interpretation of the data. Once I satisfied them about that, they retreated to a different position: that CDC must have a good reason for its choice of messages, even if those messages seemed to contradict the data. Only occasionally did I manage to convince anyone that more honest messaging might be preferable – and then came the clincher: “It is our policy always to adhere to CDC recommendations.”
23. But more often than not state and local health officials simply don’t know when the recommended messaging contains falsehoods. One of the most common patterns I’ve seen is this two-step dishonesty:
- The public health leadership carefully crafts public statements, policy positions, and talking points that are intentionally misleading but not actually false.
- The public health followership is duly misled. Local agencies and individual clinicians restate in a simpler, clearer way what they think the leadership was saying – and the restatement is a genuine falsehood.
24. I have seen this pattern dozens of times (and no doubt missed it hundreds of times) – on issues from the efficacy of the flu vaccine to the foolishness of Ebola quarantine. I need to stress again that the flu vaccine is surely better than no vaccine, and quarantining returning Ebola volunteers was probably an unnecessary precaution. The dishonesty of public health is usually – though not always – exercised on behalf of positions that are fundamentally sound, on behalf of desired outcomes that are fundamentally the right outcomes. They are usually shortcuts – bad means to good ends.
Dishonesty, Disrespect, and the MMR Vaccine
![]() 25. I said a few minutes ago that altruistic dishonesty like the OPV example isn’t confined to the developing world. A good U.S. example is the widespread claim that measles is roaring back and that parents who don’t vaccinate their children with the measles-mumps-rubella combination shot, the MMR, are seriously endangering their children’s health and the health of neighbors. Here are some undeniable truths about MMR vaccination:
25. I said a few minutes ago that altruistic dishonesty like the OPV example isn’t confined to the developing world. A good U.S. example is the widespread claim that measles is roaring back and that parents who don’t vaccinate their children with the measles-mumps-rubella combination shot, the MMR, are seriously endangering their children’s health and the health of neighbors. Here are some undeniable truths about MMR vaccination:
25.1 Herd immunity against childhood infectious diseases prevents huge amounts of mortality and morbidity. The measles, mumps, and rubella vaccines are marvels of public health. If sizable numbers of U.S. parents stopped vaccinating their children, these diseases might very well come roaring back.
25.2 In the U.S., the number of parents who don’t vaccinate their children falls pretty far short of the number that would yield this disastrous outcome. Measles is not roaring back. A chart of annual measles cases in the U.S. since 2010 show no upward trendline. Some physicians and public health professionals fear that measles could come roaring back at some point in the future if more parents stopped vaccinating their children – and they are right. Some imagine that this has happened already – and they are wrong. Others publicly claim it has happened already, knowing it hasn’t, in order to help prevent it from happening. That third group is doing what I have called altruistic dishonesty – misleading the public in a good cause.
25.3 Let me rub it in. Imagine you’re a pediatrician in a typical U.S. community (not one of the pockets where large numbers of people are unvaccinated and herd immunity is genuinely inadequate – including the Somali community here in Minneapolis). The parents of a patient wish to skip their child’s MMR. (Leave aside legal requirements for the sake of this hypothetical.) The probability that vaccinating the child will lead to a serious adverse response, something like anaphylaxis, is of course tiny. The probability that not vaccinating the child will lead to a case of measles with serious long-term morbidity is also tiny. I don’t know which risk is bigger, but surely we can agree that both are negligible, both on the order of one-in-a-million or less.
25.4 In other words, parents who don’t vaccinate their children are free-riders. They are not doing their share to sustain herd immunity. But at least so far, herd immunity in most neighborhoods is being satisfactorily sustained without them. In the absence of a current outbreak, if you tell your patient’s parents that they are seriously endangering their child or a neighbor child by skipping or postponing the MMR, you are either misinformed or dishonest.
25.5 You’re doing it in a good cause. It is altruistic dishonesty. In fact, a physician friend told me she would consider it malpractice for a doctor to inform a patient that the current risk of not getting the MMR is about the same as the current risk of getting the MMR. She didn’t dispute that that was true. But she considered it a truth that doctors could not ethically tell patients.
25.6 In terms of current risk, not possible future trends, both the risk of getting the MMR and the risk of not getting the MMR are orders of magnitude lower than many risks children are exposed to every day – the risk of owning a backyard swimming pool, say, or even the risk of going unvaccinated against the flu (which kills orders of magnitude more Americans every year than measles).
25.7 You can make a good case for requiring everyone to get the MMR, precisely because it’s a “prisoner’s dilemma” situation: It is fairly sensible for the individual child not to get the MMR as long as most other nearby children do get the shot, but everyone is better off if everyone is required to get it than if lots of children fail to get it. So requiring the MMR makes sense. But telling a parent that not vaccinating his or her child is taking an unconscionable risk is simply false.
26. Most parents accept this dishonest claim without question when they hear it from their pediatrician. (The pediatrician may well accept it without question too.) But I think a lot of parents, especially those who were nervous about vaccination in the first place, sense the dishonesty. They might or might not be responsive to an honest plea for altruism, to do their share to keep herd immunity working. But their response to a dishonest appeal to the health of their child isn’t just greater skepticism about the MMR. We all have an algorithm that says don’t trust liars. So the mistrust is generalized to vaccination more broadly, and to public health itself.
27. I hasten to add, yet again, that I have no evidence to demonstrate my claim that even when it’s motivated by altruism, public health dishonesty leads to mistrust. In fact, as I pointed out earlier, I have begun to suspect that it isn’t true, at least not in the short term. But it should be true. And I continue to worry that eventually the bill for public health dishonesty, even altruistic dishonesty, will come due.
28. As long as I am talking about the MMR, let me mention some aspects of MMR dishonesty that are not altruistic:
28.1 According to the ACIP, just about nobody needs the second rubella vaccine dose. Here’s an excerpt from the ACIP’s 2013 “Summary Recommendations”: ![]()
For prevention of rubella, 1 dose of MMR vaccine is recommended for persons aged ≥12 months.
We give a second rubella dose to millions of children every year only because that unnecessary vaccine dose comes as part of a package deal with the measles and mumps vaccine. The combo shot is efficient for pediatricians, with regard to room in their refrigerators and speed in moving on to the next patient. It saves the child some pain to give several doses in one shot. It keeps parents, especially vaccine-hesitant parents, from realizing how many separate vaccine doses their children are actually receiving. And it encourages parents to accept all three vaccines instead of making three independent decisions.
28.2 The vast majority of patients don’t need the second measles dose either. CDC says one MMR is about 93% effective at preventing measles if a vaccinee is exposed to the virus; the second MMR increases efficacy to 97%. It’s not a booster; it’s just a second shot, literally, in case the first one didn’t work. So if the three vaccines in the MMR were packaged separately, vaccine-hesitant parents could request measles titers (antibody tests to see if their kid needs a second dose) – and most of the time they could skip the second measles shot too.
28.3 There is no evidence that an unnecessary rubella and measles vaccine dose does significant harm. So regardless of its motives, the ACIP’s decision to recommend phasing out the individual vaccines in favor of the combo shot didn’t do significant harm either. Even if individual shots were still available in the U.S., which they are not, I would still see nothing wrong with recommending the combo shot to the vast majority of parents, who are content to go with their doctor’s recommendation. If offered the choice, the vast majority of parents would be unlikely to opt for a measles titer test followed by one or two additional shots rather than a second MMR.
28.4 But what about the minority of parents who are worried about what they consider an excessive vaccine load on their children? They might very well prefer to make the effort to avoid unnecessary vaccine doses. The public health profession has chosen a path that denies them that option. And it has chosen not to tell them that their only remaining option entails at least one and usually two unnecessary vaccine doses. It is hard not to see these decisions as disrespectful of the concerns of vaccine-hesitant parents.
28.5 Of course most pediatricians don’t know why the individual measles, mumps, and rubella vaccines were phased out. They don’t know that none of their patients needs the second rubella dose and very few need the second measles dose. They are simply going with the leadership’s recommendation. So when they tell parents that all three doses in the second MMR are needed, they are mistaken, not lying.
Here is a CDC statement on that subject:
Getting every recommended dose of each vaccine provides children with the best protection possible.
28.7 The MMR is not unique. As the recommended number of pertussis doses increases, vaccine recipients also get extra or premature doses of diphtheria and tetanus vaccine, since those vaccines are combined the same way the MMR is combined. I am not saying this is dangerous. I am saying it conflicts with the Guild’s assertion that all vaccine doses are necessary as scheduled.
Here is an excerpt from the American Academy of Pediatrics webpage entitled “The Childhood Immunization Schedule: Why Is It Like That?” ![]()
Q2: How are the timing and spacing of the shots determined?
A: Each vaccine dose is scheduled using 2 factors. First, it is scheduled for the age when the body’s immune system will work the best. Second, it is balanced with the need to provide protection to infants and children at the earliest possible age.
If you can give the second dose of MMR as early as 28 days after the first dose, why do we routinely wait until kindergarten entry to give the second dose?
The second dose of MMR may be given as early as 4 weeks after the first dose, and be counted as a valid dose if both doses were given after the first birthday. The second dose is not a booster, but rather it is intended to produce immunity in the small number of people who fail to respond to the first dose. The risk of measles is higher in school-age children than those of preschool age, so it is important to receive the second dose by school entry. It is also convenient to give the second dose at this age, since the child will have an immunization visit for other school entry vaccines.
This example is about disrespect as well as dishonesty. We ridicule parental anxiety as a reason for delaying a vaccination; we comfortably delay vaccinations for our own reasons of convenience; we hide the delays we have built into the recommended schedule and insist that all delays are unconscionably hazardous.
28.10 I don’t see the ACIP’s delay of the second MMR shot as a significant risk. I am confident that if public health professionals really believed that measles was roaring back, as they often claim to believe, they would surely harvest this low-hanging fruit (the small percentage of kids for whom the first MMR dose didn’t produce measles immunity) and instantly recommend that all kids get their second MMR shot a month after their first – not three to five years later.
28.11 When parents want to space out vaccinations, we tell them their reasons are specious and any delay is dangerous. When public health decides to space out vaccinations, we judge that the delay isn’t dangerous after all – in fact, we don’t consider it a delay at all, because it complies with our schedule. And we keep our reasons to ourselves.
29. I said I would focus today more on the dishonesty side of my outrage model than the disrespect side. But the treatment of parents who want to space out their children’s vaccinations illustrates both.
30. Again, I want to stress that I have no objections to the MMR, nor to the CDC’s recommended vaccine schedule. My objection is to how we treat parents who do have objections – especially how often we respond to their objections by telling them things that simply aren’t true.
31. Part of public health’s (and medicine’s) dishonest and disrespectful mistreatment of vaccine-hesitant parents is grounded in injured pride. Let me talk some more about the MMR in this context as well.
31.1 As most of you know, Andrew Wakefield published a study some years ago suggesting that the MMR vaccine might increase the incidence of autism. Wakefield’s study has been withdrawn; it was grotesquely mistaken and dishonest.
31.2 But here’s the question I want to raise: Is it fortunate or unfortunate – good or bad for public health – that Wakefield was wrong? If Wakefield had been right that combining the measles, mumps and rubella vaccines somehow accounted for a lot of autism, we would have separated the three vaccines again (as Wakefield recommended) and autism rates would have plummeted. As it is we continue to bundle them together, even though many parents still worry that the MMR might cause autism. And the solution to the scourge of autism is as distant as ever.
31.3 So why do public health people so often sound triumphant rather than disappointed when they explain that the MMR doesn’t contribute to autism … even when they’re saying it to the parents of an autistic child who are desperate for an explanation, a cause for their child’s condition?
31.4 Usually when a promising hypothesis turns out to be unfounded, that’s a disappointment. But the rejection of this promising hypothesis, which would have offered an easy way to reduce the incidence of autism, is to most public health professionals a huge victory. I get it that the triumph of truth over error – or over fraud – is always a victory. But isn’t it, at least, a sad victory? Wouldn’t patients be better off if Wakefield had been right?
31.5 I make this point often in presentations to public health audiences, and they almost never resonate to it. I think that’s revealing, and I think it’s discouraging. On some deep emotional level, it seems like a lot of public health professionals are more deeply committed to being vindicated, to being right, than they are to their patients’ welfare.
31.6 Of course that wouldn’t keep them admitting an uncomfortable but important truth. I realize that if Wakefield had turned out right, the public health profession would have seen it, acknowledged it, and abandoned the MMR combo shot. Still, it’s amazingly difficult for the public health profession to talk about the vaccination-autism connection with compassion for those who are clinging to that hypothesis.
31.7 And when vaccine skeptics accept that the MMR doesn’t contribute to autism (and that thimerosal preservative doesn’t either) and worry instead that too many vaccines concentrated into too little time might be the culprit, why do so many public health professionals roll their eyes in frustration that the critics keep changing the terms of the debate … as if it were somehow illegitimate to abandon a discredited hypothesis in favor of one about which much less is known?
31.8 Not to mention that we typically go too far when we claim that it is totally certain that there is absolutely never a vaccination-autism connection – ignoring Hannah Poling and other rare cases where something on the autism spectrum was plausibly if not definitively connected to a child’s vaccinations (in Hannah Poling’s case, possibly because of her underlying mitochondrial disorder).
32. Let me try to capture my point about pride this way. Some years ago, I posed the following question to a group of public health professionals: “Suppose there were data that showed indisputably that more kids would end up getting vaccinated if you conceded that on rare occasions vaccination might lead to something like autism, and apologized for having implied otherwise, than if you kept denying that there could ever be a connection. Would you then make the concession and the apology?” There was silence. Then various people in the group advanced the argument that the so-called exceptions (Hannah Poling and others) are at most anomalies or unexplained sequelae of vaccination where the legal process gave the patient the benefit of the doubt, even if it was quite a small doubt. “Okay,” I said, “but we’re postulating that you can get more kids vaccinated just by granting that the exceptions might be valid, not that they necessarily are but just that they might be, not always or often or even occasionally but rarely. Would you make that concession for the sake of improving vaccination uptake?” I couldn’t get the group to agree to swallow its pride in order to vaccinate more children. A very doctrinaire position on a possible though rare downside of vaccination was a higher priority than vaccination itself.
33. I have an ample store of additional examples of public health dishonesty about infectious diseases (not to mention other public health issues like e-cigs).
34. But in my remaining time, I want to focus on two recent emerging infectious diseases, Ebola and Zika. I will confine myself – with some difficulty – to one example for each. Both examples are a little complicated to explain:
- The debate in the U.S. over whether returning Ebola volunteers should be quarantined – and in particular the cases of Craig Spencer, Pauline Cafferkey, and Kaci Hickox.
- The failure of the U.S. Congress to pass a Zika funding bill from President Obama’s February request until a Zika provision was finally signed into law at the very end of September.
Ebola Quarantine
![]() 35. The basic thrust of nearly all public health communications regarding U.S. Ebola quarantine can be summarized thusly: “The science proves that there is no need to quarantine returning Ebola volunteers because asymptomatic persons cannot transmit Ebola. Politicians who have instituted Ebola quarantine policies are ignoring Sound Science, probably in order to reassure an unduly frightened public and gain a political advantage by doing so.” I have collected a wealth of statements from public health sources to this effect. I will share a few of them a little later if time permits.
35. The basic thrust of nearly all public health communications regarding U.S. Ebola quarantine can be summarized thusly: “The science proves that there is no need to quarantine returning Ebola volunteers because asymptomatic persons cannot transmit Ebola. Politicians who have instituted Ebola quarantine policies are ignoring Sound Science, probably in order to reassure an unduly frightened public and gain a political advantage by doing so.” I have collected a wealth of statements from public health sources to this effect. I will share a few of them a little later if time permits.
36. I agree with the public health mainstream that U.S. Ebola quarantine policies were probably unnecessary. They certainly turned out unnecessary. The only cases of Ebola transmission in the U.S. were from a hospitalized Dallas patient to two nurses. Those two nurses, their patient (who entered the country from West Africa on his own), and one returning Ebola volunteer are the only four U.S. Ebola cases – not counting an additional handful of patients airlifted to the U.S. for treatment, already in isolation. None of the four gave any member of the U.S. public Ebola before being hospitalized for treatment.
The “n” is very small, obviously. The argument against quarantine doesn’t hinge on the fact that nobody gave anybody else Ebola in the U.S. except inside a hospital. It hinges on the contention that nobody could possibly have done so as long as symptomatic people were isolated.
37. The strongest argument against quarantine is the evidence that Ebola transmission is rare and perhaps impossible until the sufferer is symptomatic, and quite possibly until the sufferer is emitting infectious bodily fluids.
37.1 This evidence is scanty rather than plentiful, grounded in small-scale studies in Africa. So the statement that “asymptomatic people cannot transmit Ebola,” while probably true, is more absolutist than I think the science can support.
37.2 The CDC Ebola protocol most recently in effect recommends either quarantine or direct active monitoring with extreme movement restrictions for asymptomatic people with the highest probability of having been infected: people known to have had close contact with the bodily fluids of Ebola patients (via a needlestick, for example).
Obviously if it were truly impossible for asymptomatic people to transmit Ebola, there would be no reason for CDC to hedge its bets by restricting the movements of any asymptomatic people, no matter how high the likelihood that they were incubating Ebola.
37.3 Still, even if asymptomatic transmission might not be quite as impossible as the public health claims kept reiterating, it is clearly extremely uncommon.
37.4 But to elide from “asymptomatic people rarely if ever transmit Ebola” to “it is contrary to science to quarantine asymptomatic people,” you have to ignore two other possibilities: that people might become symptomatic suddenly; and that early symptoms might be missed, ignored, denied, or misinterpreted.
38. With regard to sudden onset, it worth noting that “sudden onset” or “abrupt onset” of symptoms is part of the CDC and WHO case descriptions for Ebola. That is, CDC and WHO both say that it would be commonplace – more the rule than the exception – for someone who is incubating Ebola to suddenly become symptomatic.
38.1 If the suddenly appearing symptom is fatigue or fever, the newly symptomatic person may pose relatively little risk to others. But if the suddenly appearing symptom is vomiting or diarrhea, the risk would be greater. I know of no data suggesting how often that happens – how likely a person incubating Ebola is to be asymptomatic at 8 a.m. and vomiting on the subway or having diarrhea in the bowling alley at 2 p.m.
Vis-à-vis sudden onset, nothing but quarantine will do. Even direct active monitoring – having a third party actually see the person and check for symptoms twice a day – won’t do the job if bodily fluids are likely to be ejected between one visit and the next.
38.2 I mention vomiting on the subway and having diarrhea in the bowling alley in honor of Craig Spencer, an Ebola volunteer who was incubating Ebola when he returned to his home in New York City from his work in West Africa for Médecins Sans Frontières. A couple of days before his symptom onset, Spencer felt sluggish – but he didn’t consider that a symptom. The day before his symptom onset he had a busy day, including a three-mile run followed by time on the New York subways and in a New York bowling alley.
38.3 The following morning – October 23, 2014 – Spencer had a low fever of 100.3°F, just below the CDC screening cutoff, 100.4°F. CDC’s “Algorithm for Evaluation of the Returned Traveler” ![]() then in effect called for immediate isolation and evaluation if a returned traveler had a temperature of ≥100.4°F, “or compatible Ebola symptoms,” defined as “headache, weakness, muscle pain, vomiting, diarrhea, abdominal pain, or hemorrhage.”
then in effect called for immediate isolation and evaluation if a returned traveler had a temperature of ≥100.4°F, “or compatible Ebola symptoms,” defined as “headache, weakness, muscle pain, vomiting, diarrhea, abdominal pain, or hemorrhage.”
Only a week earlier, the CDC returned traveler temperature cutoff had been much higher: ≥101.5°F. It was lowered to ≥100.4°F after two Dallas nurses who had cared for Ebola patient Eric Duncan were diagnosed with Ebola within a day of presenting with temperatures of 100.6°F and 100.5°F, plus symptoms (a rash and a sore throat) that weren’t on the Ebola symptom list.
38.4 So with his temperature below the cutoff, Spencer had no obligation to call it in. And when he did, officials at Médecins Sans Frontières and the New York City Health Department had no apparent basis for deciding that he should be isolated as a possible Ebola case. You could argue in hindsight that Spencer’s sluggishness was equivalent to “weakness,” which is on the CDC symptom list. But he’d had that “symptom” for days and didn’t consider it a symptom.
38.5 For whatever reason, Spencer did call in his symptom(s), and officials did decide to take seriously his possible Ebola infection. He was transported by specially equipped ambulance to New York City’s Bellevue Hospital, where he was isolated. He tested positive for Ebola the same day. The positive blood test was less then 24 hours after he was socializing in a bowling alley and riding the subway; it was less than 12 hours after his first symptom … if you decide to count his below-the-cutoff fever as a symptom (and decide not to count his prior sluggishness, especially given his three-mile run).
38.6 This sequence of events raises the question: Did Spencer have other “compatible Ebola symptoms” that would have justified his immediate isolation and testing? In particular, might he have had diarrhea?
Well, the patient – today – developed a fever and had some gastrointestinal symptoms as well. So these are the symptoms that let us know that this patient had a clinical picture that was really fully consistent with Ebola.
Gastrointestinal symptoms that are “really fully consistent with Ebola” sound like diarrhea. But Dr. Bassett didn’t use the word.
New York State Health Commissioner Howard Zucker was even vaguer about what Spencer’s additional symptoms, if any, might have been:
His symptoms began – he had a fever – that symptom began this morning, and some of the other symptoms as well this morning.
Early the next morning, Associated Press reporters Mike Stobbe and Marilynn Marchione did use the word “diarrhea”:
Spencer, a 33-year-old emergency room doctor, returned from Guinea on Oct. 17 and sought treatment Thursday [Oct 23] after suffering diarrhea and a 100.3-degree fever.
Later that second day, city and state health officials held a second news conference about the Spencer case. Commissioner Bassett made two comments of possible relevance:
We want to … find every person with whom he may have been in contact and we want to account for all of his time, from the time he developed symptoms until he was safely placed in isolation, and in care, at Bellevue Hospital. …
He reported no watery diarrhea, no vomiting, no loss of control of body fluids. We don't see any possibility that he contaminated his apartment.
Did Dr. Bassett’s reference to the plural “symptoms” refer to any symptoms beyond Spencer’s sluggishness and low-grade fever – symptoms that might have explained her previous day’s characterization that they were “fully consistent with Ebola”? And when Dr. Bassett said that Spencer “reported no watery diarrhea,” was that just her way of saying that his bowel movements were normal? Or was she carefully avoiding committing herself on whether he had non-watery diarrhea that he managed to deposit in the toilet?
Spencer’s diarrhea, if he had diarrhea, disappeared from the official narrative of his illness onset that was published six months later. So did any reference to the gastrointestinal symptoms that had been mentioned at the Day One news conference.
In the article on the Spencer case in the April 3, 2015 Morbidity and Mortality Weekly Report (MMWR), the only early symptoms mentioned are his fever (a fever below the CDC criterion in effect at the time) and “fatigue” (what Spencer had called “sluggishness,” also not on the CDC list of symptoms, though “weakness” is listed). Here is the relevant passage:
On October 23, 2014, NYC DOHMH was notified by Médecins Sans Frontières (MSF) that one of its physicians who had returned to NYC nine days earlier from treating Ebola patients in Guinea had an oral temperature of 100.3°F (37.9° C). The physician reported fatigue for 2 days without other symptoms (e.g., vomiting, diarrhea, cough, muscle aches, or abnormal bleeding)…. Because of his travel and work history and symptoms consistent with Ebola, DOHMH arranged for immediate transfer [to Bellevue].
38.7 Together with my wife and colleague Jody Lanard, I emailed the MMWR authors (many of whom were New York City health department people) and the city and state health department heads about the discrepancy. We got no response. More recently I had a chance to raise the question in person with Dr. Bassett, the New York City health department head – a client now on Zika and some other issues. She said she didn’t remember any discrepancy.
But the discrepancy is real. Spencer’s low-grade fever did not reach the level specified in the CDC case definition for Ebola. Unless he also had gastrointestinal symptoms such as diarrhea or vomiting, it is hard to see why he would have been isolated to rule out Ebola. “Gastrointestinal symptoms” were mentioned at the news conference when he was first hospitalized. They were explicitly denied in the MMWR case report. Perhaps Spencer’s only symptoms were his 100.3°F fever and his sluggishness/fatigue, and Drs. Bassett and Zucker were mistaken at the news conference. Or perhaps there were reasons not to acknowledge sudden onset of GI symptoms such as diarrhea or vomiting that might have endangered other New Yorkers if they had occurred in public rather than at home.
38.8 Spencer was home when his low-grade fever and his diarrhea – if he had diarrhea – began. Nobody had contact with his bodily fluids at least in part because he was home, near his own bathroom. If the diarrhea had come on equally suddenly the previous day, he would not have found a toilet on the subway; in the bowling alley, it would surely have been a toilet many others would use after him.
- If we count sluggishness as an Ebola symptom, then Spencer (or Médecins Sans Frontières, which was his self-monitoring contact) ignored his first symptom for a couple of days. Fortunately, he had slow onset of his later symptoms.
- If we don’t count sluggishness as an Ebola symptom but we count a fever below the CDC cutoff, and if we ignore the early references to gastrointestinal symptoms and diarrhea, then Spencer had sudden onset of a symptom (his fever) that he duly reported, and he was safely isolated before other, more transmissible symptoms could materialize.
- If we take the early references to gastrointestinal symptoms and diarrhea seriously, then Spencer had sudden onset of symptoms that could have posed a risk to others, and it was lucky he happened to be home and near a private bathroom.
38.10 It is worth noting in this context that Spencer’s fiancée and two close friends were quarantined for some days (but not 21 days, as initially planned), first at Bellevue Hospital and later at home. I am not aware of any objections voiced by public health professionals to these quarantines, even though the three quarantined individuals were asymptomatic and their only exposure was to Spencer, who we are now told (according to the MMWR article) had no symptoms except sluggishness and a low-grade fever.
In fact, in the second news conference the day after Spencer’s Ebola diagnosis, New York City Health Commissioner Bassett discussed the three quarantine orders with clear approval – after first voicing her approval of the earlier quarantine of the Dallas family Eric Duncan had been visiting before his Ebola was diagnosed:
I think it’s instructive for all of us to recall the experience with the household of Mr. Thomas Eric Duncan, the gentleman who is the only person to succumb to Ebola in the United States. His entire household was quarantined. As we’ve been discussing, he was quite sick while he was still at home…. He had diarrhea. He had fever but no one in his household became infected with the Ebola virus…. So, I think that the household was appropriately quarantined but I think it’s instructive always to remember that this is not a virus that is easily transmitted….
There are three individuals who have been served with quarantine orders. These are all individuals who had extensive contact with the patient. The fiancée lives with the patient and there were two friends who spent quite a bit of time with the patient and they have been served with quarantine orders. What that means, is that they are required to be isolated under a commissioner’s order for a period of 21 days from their last contact with the patient. Our staff will visit the quarantined individuals daily and take their temperatures.
39. With regard to symptoms being missed, ignored, denied, or misinterpreted, there are many relevant points. I don’t want to get even more granular here, so let me summarize some of the main ones:
39.1 There are two well-known examples of Ebola-infected prominent doctors in West Africa who continued to go to work, socialize intimately, and have family parties after becoming symptomatic – and transmitted Ebola to others in the process. No one knows whether they misinterpreted their symptoms or intentionally ignored them, because they both died.
39.2 As I have mentioned, Spencer felt “sluggish” for a couple of days before he went out on the town. It’s not clear if he decided his sluggishness wasn’t a symptom or if he reported it to someone at Médecins Sans Frontières who decided it wasn’t a symptom. An awful lot of people feel sluggish after a grueling overseas assignment and a long trip home.
39.3 On October 24, 2014, the day after Spencer was diagnosed, returning volunteer Kaci Hickox had several elevated temperature readings when she was screened at Newark Airport and after being moved to a hospital setting. Other temperature measurements were within normal range. Hickox immediately claimed that the elevated readings were false positives, and that she was just flushed and upset about being detained. (We will turn shortly to the Hickox story in greater detail.) Since Hickox dismissed her airport and hospital fever readings as false positives, I have to assume that she would have had the same dismissive reaction if she had been self-monitoring at home.
39.4 There is ample theoretical and empirical work to support the existence of fear-driven psychological denial as a reason why people with diseases and especially dreaded, deadly diseases often deny that they have symptoms, or deny that their symptoms mean what they mean. Every clinician has treated many patients who misreported or misinterpreted their symptoms because of denial.
39.5 Doctors and other medical personnel are famously more, not less, vulnerable to this sort of denial (and such related psychological defenses as rationalization and minimization). Doctors take notoriously poor care of their own health. Healthcare workers at all levels often go to work sick.
39.6 A second potential motive for ignoring or misinterpreting symptoms is reluctance to make a fuss, to inconvenience everyone, and to embarrass oneself. No returning volunteer wanted to be the false positive who panicked at nothing and forced an expensive and frightening public health response because she was jetlagged and had a headache.
39.7 People who have made uncommon sacrifices for the common good often feel entitled. Heroes and saints sometimes act like jerks. There are well documented (and appalling) instances of returning Ebola volunteers acting like jerks at airport screening stations, as I will describe in a minute.
39.8 Some of the symptoms on the CDC list of Ebola symptoms are very common – and would be even more common among people just back from an exhausting month or more in Africa. If these symptoms were being taken literally, there should have been a lot of false positives – returning volunteers who reported a fever or diarrhea or whatever and according to the recommended CDC protocol had to be isolated for a few days until active Ebola disease could be ruled out. The fact that so few returning volunteers were isolated and tested suggests either that they were not reporting symptoms they considered routine or that the health officers to whom they were reporting these symptoms were deciding that no further workup was needed.
39.9 Three of the four Ebola cases diagnosed on U.S. soil – Eric Duncan, Amber Vinson, and Craig Spencer – had their early symptoms missed (if we count Spencer’s “sluggishness” as a symptom). All four (the fourth is Nina Pham) tested positive within a day of becoming suspect Ebola cases.
40. Finally, consider the case of Pauline Cafferkey, a Scots nurse who was recently cleared of professional misconduct.
40.1 Returning from Ebola work in West Africa, Cafferkey and a group of fellow medical volunteers were screened at Heathrow. After making a big fuss about delays in the screening, several of the group got permission to take each other’s temperatures. Cafferkey’s reading was well above the criterion for immediate isolation to rule out Ebola. So some members of the group, including at least one doctor, decided to write a lower, below-the-criterion number on her screening form and she proceeded to baggage claim. There she took a fever-reducing paracetamol, waited, and then returned to the screening area after a colleague urged her to do so. She was re-screened by an official this time, and her temperature, post-paracetamol, was low enough to be allowed to fly on to Glasgow. By very early the next morning she was much sicker, was diagnosed with Ebola, and had to be flown back to London on a military med-evac plane for treatment.
40.2 As far as I can tell, Cafferkey never lied, and she wasn’t the one to write down the false temperature reading. She periodically told some staff in the re-screening area that she had had a fever and had taken paracetamol (though she did not tell them that a dishonest temperature reading had been entered onto her original screening form by a colleague). Other times she failed to mention these facts to the re-screeners who permitted her to fly on to Glasgow.
40.3 Last month the U.K.’s nursing professional body cleared Cafferkey on charges of professional misconduct. It was clear from the panel report that Cafferkey’s behavior would normally have been grounds for disciplinary action. But not in her case. She was exhausted by jetlag and in the early stages of Ebola, the panel judged, so she had to be forgiven for showing such horrible professional judgment – abusing the screening process, misleading the screening authorities, and endangering quite a large number of people. After listening to testimony it considered to be expert, the panel judged that people in the early stages of Ebola shouldn’t be expected to behave rationally and responsibly vis-à-vis their own symptoms.
Here are two excerpts from the panel’s conclusions:
13. Evidence before the Case Examiners regarding the potential effect of the Ebola virus on Ms Cafferkey’s state of mind was from Dr 6, PHE investigator. The Case Examiners commented that he states, “when someone is at the early stages of the infection, and just has a raised temperature, this may have a clinical effect on their thought processes. They may not be as rational as they would be when well. This could also be a psychological effect. Ebola is a very unpleasant illness, and I would not be surprised that someone in Ms Cafferkey’s situation might not think straight. There are good clinical and psychological reasons why that person might not make competent decisions”.
15. Dr 7 says, “I have no doubt that a combination of early Ebola Virus infection and fatigue resulting from a busy night shift followed by a lengthy journey by bus across Sierra Leone then by plane to the UK via Morocco would have impaired Pauline’s judgement at the time of entering the screening process at Heathrow airport.”
40.4 At least one newspaper article says that disciplinary action is planned for the other members of her group, who were not incubating Ebola but nonetheless collaborated in the fraud. I don’t know if it’s true.
40.5 A few days after being cleared, Cafferkey called for a probe of Public Health England and its Ebola screening operation, saying that they endangered her and others by missing her Ebola symptoms at the airport. I assume she meant that they let the volunteers take and record each other’s temperatures. This argument conflicts with the more common mantra of those arguing against quarantine of asymptomatic, or allegedly asymptomatic, volunteers: “Who would know better than a returning health care worker that it is important to report early symptoms?”
40.6 The Cafferkey case has three bottom lines relevant to the Ebola quarantine debate:
- Both Cafferkey and her accusers agreed from the outset that a returning Ebola volunteer with an intermittent fever reading shouldn’t be allowed to mingle with the general public – that Cafferkey shouldn’t have been allowed to fly on from London to Glasgow.
- Both Cafferkey and her accusers ended up agreeing that a returning Ebola volunteer in the early stages of Ebola virus disease can’t be expected to react responsibly to his or her early symptoms – that Cafferkey did act irresponsibly but that was because of her exhaustion and her illness, not her character.
- At least sometimes returning Ebola volunteers who were not infected decided to flout the screening rules and hide symptoms, in this case a colleague’s fever, presumably because they mistakenly assumed the symptom was something other than Ebola.
40.7 At the time of the Craig Spencer and Kaci Hickox cases (October 23 and 24, 2014), the CDC standard for Ebola monitoring was self-monitoring, not active or direct active monitoring. The three conclusions I have drawn from the Pauline Cafferkey case support at least direct active monitoring – more than the CDC protocol in effect until well after New Jersey, New York, Connecticut, and other states implemented quarantine or close-to-quarantine policies. To get from direct active monitoring to quarantine, you would have to be worried about sudden onset of symptoms, or worried that even third parties might misread symptoms – not just worried about a returning volunteer’s misrepresentation or misinterpretation or denial of his or her own symptoms.
41. Keep the Cafferkey case in mind as I review the facts of a case likely to be more familiar to you, that of Kaci Hickox. On October 24, 2014, the day after Spencer’s sudden onset (if that’s how we choose to interpret it), Ebola nurse Kaci Hickox arrived at Newark Airport from West Africa.
41.1 The conventional wisdom, reiterated endlessly by public health sources among others, is that New Jersey Governor Chris Christie – a pugnacious and politically ambitious Republican – ordered Hickox quarantined even though she was asymptomatic, under a brand new New Jersey quarantine policy that was contrary to CDC recommendations and contrary to Sound Science – and that he did so not to protect public health but to gain political advantage by catering to a panicky public.
41.2 Now here’s what actually happened.
In the hours after her plane landed, Hickox had multiple temperature readings with both a forehead screening thermometer and an oral thermometer. At the CDC quarantine station at Newark Airport, where returning volunteers were screened, her first temperature reading was normal, and under the CDC protocol in effect at the time she would have been released into voluntary self-monitoring. New Jersey, however, had just instituted a mandatory home quarantine policy in the wake of Spencer, under which she would have been sent home and required to stay home with active monitoring by a health officer. But Hickox was not a New Jersey resident. So she was held at the airport for several hours, presumably while New Jersey officials tried to figure out what to do with her.
While she was still at the airport quarantine station, Hickox’s temperature was taken again. She later told the media that her second reading with a forehead thermometer was 101°F, well above the CDC threshold (then) of 100.4°F as a symptom that CDC stipulated should lead to immediate isolation for a possible rule-out-Ebola workup (not necessarily to a 21-day quarantine). Hickox’s temperature according to that second test was higher than the fever Spencer had had the day before when he was rushed to the hospital, isolated, and diagnosed with Ebola. It was higher than the fever the two Dallas nurses had had at the time they were put into isolation and then found to have Ebola.
Later, at the hospital where Hickox was isolated, readings from a forehead thermometer continued to be elevated, but readings using an oral thermometer were below the threshold.
41.3 Hickox said and still says that the forehead thermometer readings were false positives, because she was “flushed” rather than feverish. Nonetheless, the CDC protocol called for anyone with a fever reading higher than 100.4°F to be isolated until active Ebola disease could be ruled out; it didn’t say low readings should cancel out higher ones. So in accordance with the CDC protocol, Hickox was isolated until active Ebola disease could be ruled out.
Although virtually all the media coverage and public health commentary got it wrong, Hickox was not an asymptomatic traveler quarantined at a Newark hospital under the New Jersey protocol. She was symptomatic under the CDC protocol. She had sudden onset of a fever above 100.4°F. She was therefore isolated until active Ebola disease could be ruled out.
It is probably true that New Jersey would have quarantined Hickox if she had had no symptoms; it’s also arguable that keeping her in the airport for some period (up to several hours) before her elevated temperature reading was itself a brief quarantine, or at least a detention. But it is hard to argue that her fever reading should have been ignored because it was intermittent, or because it depended on what device was used to measure it, or because she claimed she was just flushed and upset. Certainly nothing in the CDC recommended protocol would have permitted that.
41.4 The airport quarantine station through which Hickox was processed is permanently staffed by CDC. Although CDC has never said whether or not it participated in and agreed with the decision to isolate Hickox, it almost certainly did – but when the controversy arose it decided (or perhaps was instructed by the White House) to let Governor Christie take the rap. I have to say this is one of the examples of public health dishonesty that most angers me. I suppose it’s conceivable that CDC wasn’t consulted in this decision, but the odds are overwhelming that it was. I devoutly hope that fact finally emerges from Hickox’s lawsuit against New Jersey and Governor Christie.
41.5 New Jersey (with or without CDC participation) did exactly what the CDC recommendations said it should do. It found a temperature reading of over 100.4°F, so it isolated Hickox for a few days in order to monitor her for fever and other symptoms and test her blood for Ebola. Three days later New Jersey health officials decided she didn’t have Ebola, though she might still be incubating it. If she were a New Jersey resident, home quarantine would probably have been the next phase. Since she wasn’t, she was driven by state police to her home state, Maine.
- Her elevated screening temperature is largely ignored, as if her claim at the time that her reading was in error should have been dispositive and she should be considered to have been asymptomatic. This is a nice example of outcome-driven reasoning. She turned out not to have Ebola after all, so public health professionals now assert that she had no symptoms.
- Also ignored is the fact that her treatment was pretty much by the CDC book except for the first few hours at the airport (not to mention the high likelihood that CDC participated in the airport decision to isolate her because of her temperature until they could rule out Ebola).
- And public health experts who must know better continue to assert that Hickox was quarantined under New Jersey’s quarantine provision, rather than isolated under the CDC protocol. (I should add that there were times during the evolution of the CDC returning traveler algorithm and the CDC movement and monitoring guidelines when the two sets of specifications conflicted with each other in some ways. So it would be fairer to say that Hickox was treated in a way that fit within the range of CDC protocols in effect the day she arrived at Newark Airport.)
- Much is also made of the “unheated tent” in which she was isolated, the absence of a flush toilet, and other features characteristic of a temporary isolation unit – which was located inside a hospital building, not in an outdoor hospital parking lot. Hickox of all people would know that a symptomatic person, isolated for rule-out-Ebola, should not be using a flush toilet, since the flushing action might spread Ebola to other parts of the room.
42. In the early days of domestic Ebola – starting with the Duncan case in Dallas – CDC’s criteria for deciding how to treat various categories of possible Ebola risk were insufficiently cautious. CDC has acknowledged that – most publicly with regard to the two Dallas nurses who were infected and the fact that one of the nurses was permitted (correctly under the protocol then in effect) to fly to Ohio and back while she was incubating Ebola. CDC changed its criteria several times both before and after the Hickox case, nearly always in the direction of greater conservativeness.
So when the governors of New Jersey and New York instituted their quarantine policies, CDC’s protocol was – it now concedes – insufficiently conservative. The final CDC protocol was still less conservative than the New Jersey and New York quarantine protocols, but only by a little. Importantly, the final CDC protocol was closer to the New Jersey and New York protocols than it was to the CDC protocol in effect when the two state governors announced their protocols. In other words, the governors filled a gap that needed to be filled, trying to figure out how to tighten up screening, with no help from CDC at the time. CDC caught up later.
43. It is still arguable that the New Jersey and New York protocols were more conservative than necessary. How conservative to be – how safe is safe enough – is of course a trans-scientific question, not a scientific one. In this case the available science provides little guidance. I haven’t tried to build a case that quarantine was the right policy for returning Ebola volunteers – only that it wasn’t a foolish or scientifically unjustified policy, given the twin risks of sudden symptom onset and misrepresented or misinterpreted symptoms.
- The Craig Spencer case can be seen in either of two lights: as a near miss that shows we were taking insufficient precautions or as “no-harm no-foul” evidence that the precautions turned out sufficient in the end.
- The Pauline Cafferkey case is clear evidence that returning volunteers should not be trusted to monitor their own symptoms.
- The U.S. military quarantined returning servicemen for 21 days.
- Some volunteer organizations imposed their own 21-day quarantines or work furloughs on returning Ebola volunteers.
- As I will discuss in a few minutes, many top U.S. hospitals and medical schools allowed students and staff to volunteer only on condition that they stay away for 21 days after returning. These policies were in effect long before Spencer and Hickox, and long before public health decided en masse that it was unconscionable of state governors to promulgate similar Ebola quarantine policies of their own.
- Finally, as I mentioned earlier, the CDC protocol for the highest-risk asymptomatic people – those reporting an Ebola needlestick accident, for example – extends to (or nearly to) quarantine. I have asked CDC people why they are okay with quarantining asymptomatic needlestick victims or imposing severe movement restrictions on them, since CDC maintains that asymptomatic people cannot transmit Ebola. They respond that needlestick victims are far likelier to be incubating Ebola than the average returning volunteer, and thus likelier to eventually develop symptoms. That’s true, of course. But it would be totally irrelevant if CDC were as confident as it claims that asymptomatic people cannot transmit Ebola.
44. Legal authorities are clear that reassuring the general public is an unacceptable rationale for imposing a mandatory quarantine on anyone. You can’t restrict somebody’s freedom because somebody else is afraid. A serious weak point in the New Jersey quarantine policy would be evidence that public reassurance was its chief purpose. That was also the principal reason why a Maine judge ruled against Maine’s restrictions on Hickox after she was transported there from New Jersey; the judge said Maine’s government hadn’t presented any evidence that Hickox might endanger people, as opposed to merely frightening them. Insofar as New Jersey’s, New York’s, Connecticut’s, and other states’ governors were being more conservative, more risk-averse, than CDC’s protocol called for, I believe their quarantines could stand legal scrutiny. But insofar as they were placating a frightened public or playing for political points, their quarantines were illegal.
None of that, of course, is relevant to Hickox in New Jersey. She wasn’t quarantined – except perhaps for a couple of hours before being isolated, and conceivably another couple of hours after her “rule out Ebola” period ended and she was released into quarantine from isolation, and then transported to Maine.
45. How much of all this did the average public health professional know before opining publicly that Ebola quarantine is unscientific and that any state official who favored a quarantine policy was flouting “The Science” for the sake of politics? Not much. How much of it did the public health leadership know? A lot, I think. Enough to qualify their anti-quarantine public statements as dishonest.
46. The vituperation with which the anti-quarantine position has been articulated is quite extraordinary. At best, science tells us how safe or dangerous a situation is likely to be. The claim that science tells us how safe is safe enough is arrogant and entirely unscientific. “How safe is safe enough” is a values question, not a science question. It is a question that’s debatable based as much on values as on science – the sort of question we expect political leaders, not technical experts, to answer (after listening to what the technical experts have to say, of course).
But public health professionals have gone way beyond arrogance. Terms like “irrational,” “idiotic,” “panic” (of course), and even “insane” have been thrown around as descriptors of Ebola quarantine as if they, too, were scientific judgments. It would be far more appropriate (and far more civil) for public health to frame this as a dilemma with reason and sense on both sides: the possible additional protection quarantine might afford the community versus the infringement on volunteers’ liberty and the possible damage to future volunteer recruiting.
46.1 Ashish Jha, director of the Harvard Global Health Institute and a named professor in the Harvard School of Public Health, crystallized the ridicule response on Oct 24, when he told Sarah Kliff of Vox:
I’m a believer in an abundance of caution but I’m not a believer of an abundance of idiocy.
Kliff’s article, focused largely on the case that Ebola quarantines are foolish, was entitled “The New York Ebola patient is a hero. Stop criticizing his bowling trip.” (As if he couldn’t possibly be a hero whose bowling trip merited criticism.) The “abundance of idiocy” quote was widely requoted and retweeted.
In a November 2014 interview in Harvard Public Health, Dr. Jha reiterated his disdain for quarantine, though less colorfully. I should add that Dr. Jha said some very wise things in that interview about other aspects of Ebola risk communication, including the need for public health to acknowledge mistakes and tell the truth even when you worry that the truth might undermine trust. But here’s what he said about Ebola quarantine:
The Centers for Disease Control and Prevention stayed faithful to the science. Despite the political pressure, they didn’t give in to the ill-conceived notion of the 21-day quarantines for everybody. Despite the politics, President Obama didn’t buckle. So while some politicians in New York and New Jersey clearly focused more on the politics than the science, the policy apparatus fundamentally got it right.
I don’t know whether Dr. Jha didn’t know, or didn’t choose to say, that at the time when states (not just New York and New Jersey) started promulgating Ebola quarantine policies, the CDC recommendation for returning volunteers in the high-risk category was self-monitoring and no long-distance travel … and that the CDC recommendation later ratcheted up to extreme movement restrictions for the highest-risk people, still asymptomatic: Stay at least three feet from everybody else for 21 days. That’s basically home quarantine plus maybe a carefully isolated walk in the park.
I also don’t know whether the ratcheting up of the CDC recommendations was motivated by politics or by science (especially what it learned from the Duncan, Pham, Vinson, and Spencer cases). Surely the CDC’s final recommendations were much closer to the New Jersey etc. policies than to the original CDC recommendations when the governors decided that the CDC recommendations were too lax and they had better craft their own policies.
46.2 This is from an October 27 NBC News article entitled “To Quarantine or Not to Quarantine: Doctors Weigh In on ‘Sledgehammer’ Tactic”:
Doctors lined up Monday to slam the controversial new quarantine measures announced by governors of states including New York and New Jersey as well as the U.S. military, saying they’re not only unjustified but could in the end endanger Americans.
“The governors’ action is like driving a carpet tack with a sledgehammer: it gets the job done but overall is more destructive than beneficial,” the editors of the influential New England Journal of Medicine wrote in a commentary.
“This approach, however, is not scientifically based, is unfair and unwise, and will impede essential efforts to stop these awful outbreaks of Ebola diseases at their source, which is the only satisfactory goal,” they wrote….
From the Infectious Diseases Society of America to the director of the National Institutes of Allergy and Infectious Diseases, there was an unusual degree of solidarity against the idea of keeping people at home for three weeks if they aren’t sick….
“We now know that fever precedes the contagious stage,” Dr. Jeffrey Drazen and fellow editors of the New England Journal of Medicine wrote in their editorial. The fever gives a traveler a chance to seek isolation and help, they argued….
“When there are no symptoms, there is no risk,” said Dr. Daniel Diekema, an infectious disease specialist at the University of Iowa and president of the Society for Healthcare Epidemiology of America, a medical association for experts in infection control and prevention….
“The reasons to do it have largely been political and to control the fear and perception of risk,” Diekema said.
It is hard to see how Dr. Drezen and the other authors of that New England Journal editorial could “know” that “fever precedes the contagious stage,” since the Journal itself had recently published a study reporting that nearly 13% of West African Ebola victims had no fever.
Also worth noting: Before the Hickox case, Dr. Diekema of SHEA was in the media matter-of-factly explaining that the asymptomatic family members of Eric Duncan were of course quarantined. Nobody, not Dr. Diekema and not even they, thought that was a foolish precaution … though like the quarantined Western volunteers, they never developed Ebola.
And in an Associated Press article the day after Craig Spencer was diagnosed – just before the Kaci Hickox furor converted the entire public health establishment into stalwart opponents of Ebola quarantine – a former SHEA president and IDSA councillor (and former president of the International Society for Infectious Diseases) validated the view that Ebola quarantines are sensible:
A three-week quarantine makes sense for anyone “with a clear exposure” to Ebola, said Dr. Richard Wenzel, a Virginia Commonwealth University scientist who formerly led the International Society for Infectious Diseases.
Some health workers could “have a kind of denial there are any exposures,” and an automatic quarantine would address that, Wenzel said.
Our [government] leaders were enabled by a fear-mongering mass media that also ignored established medical science, further stoking panic and compounding an already immense public disservice.
46.4 Some of the accusations leveled by public health professionals against Ebola quarantine were far more irrational than the quarantine policy itself. One of my favorites was the oft-stated claim that Ebola quarantine policies were “fear-mongering.” Or as Dr. Marchbein put it, “stoking panic.” If “fear-mongering” means anything, it means trying to frighten people unduly.
There’s a good argument that Dr. Peter Hotez in Houston has been fear-mongering about Zika, along with others who have argued publicly that Zika is far more widespread in the continental U.S. than CDC suspects, and that we’re going to see a rash of unexpected microcephalic babies in the months to come.
But to the extent that it wasn’t intended to protect public health, Ebola quarantine was clearly intended to calm public fears, not to exacerbate them. Accusing the governors who promulgated Ebola quarantines of a probably illegal policy of public reassurance at the expense of other people’s freedom is a coherent argument. Accusing them of fear-mongering is not.
46.5 The nearly unanimous conviction on the part of the public health establishment that Ebola quarantine was horribly wrong seems to have crystallized with the Kaci Hickox case. Before Hickox became a cause célèbre, I can find public health leaders on both sides of Ebola quarantine. Post-Hickox, they’re virtually all on the same side. Almost nobody in public health seemed to notice (or care) that Hickox was isolated for a fever, not quarantined while asymptomatic; that her isolation was compatible with the CDC protocol in effect at the time; and that the decision was made in a Newark Airport quarantine facility run by CDC itself.
I’m not sure how importantly the impending election figured in this crystallization. Would it have happened if New Jersey Governor Chris Christie hadn’t been a high-visibility, famously pugnacious Republican in an election year? If the Hickox case had happened in a blue state? If CDC had said, “Come on, she had a fever, of course New Jersey isolated her”? Maybe it would. Maybe all it took was Hickox’s highly publicized anger. Or maybe at least some of the dishonesty of public health professionals vis-à-vis the Hickox case was politically motivated. I’m not sure.
Another interesting counterfactual: What if Spencer had turned out not to have Ebola after all, and Hickox had turned out to have the disease? The case for isolating Spencer (assuming he didn’t have diarrhea) was weaker than the case for isolating Hickox. Would the public health establishment have ganged up on New York City and New York State Democratic officials for overreacting to Spencer’s mild fever the way it ganged up on New Jersey’s Republican Governor Christie? Again, I’m not sure.
46.6 What is absolutely sure is that many renowned medical schools and schools of public health imposed quarantine-like policies of their own vis-à-vis Ebola volunteers among their staff – and continued to do so, quietly, even as they joined in the demonization of Christie for “quarantining” Hickox.
46.7 Consider for example Massachusetts General Hospital (MGH), operated by Harvard Medical School. Its policy statement on Ebola volunteers, “Guidelines Regarding Possible Ebola Deployment by MGH Staff/Volunteers,” ![]() was dated September 16, 2014, just over a month before Hickox arrived at Newark Airport. The “Exposure and post-deployment repatriation” section reads in part:
was dated September 16, 2014, just over a month before Hickox arrived at Newark Airport. The “Exposure and post-deployment repatriation” section reads in part:
Potential volunteers should understand that a 21-day home “quarantine” and active fever watch period will be necessary before clinicians who have cared for Ebola patients will be allowed to return to clinical duties at Mass General Hospital.
This was at a time when the CDC protocol called only for self-monitoring and no long-distance travel, even for people in the highest-risk categories. So MGH was much, much more cautious than the CDC recommended. A month before Governor Christie announced New Jersey’s quarantine, MGH had its own quarantine-like policy. Needless to say, MGH did not come to Christie’s defense. Nor did it change its policy.
But I haven’t found any evidence that MGH as an institution ever attacked Ebola quarantine – though I have quoted already from Ashish Jha of Harvard’s School of Public Health.
46.8 Some other medical schools, hospitals, and schools of public health have the distinction of having simultaneously imposed a quarantine-like policy on their employees and students while voicing fervent disdain for the quarantine policies of New Jersey and other states. Johns Hopkins is a good example.
First, the JHU policy ![]() : For medical school students, faculty, and staff, the policy reads that they should be
: For medical school students, faculty, and staff, the policy reads that they should be
…considered as having “high risk exposures” by Occupational Health / Student Health, and according to CDC guidelines, will not be allowed to engage in patient care for 21 days.
(I can’t find any CDC guidelines that would have justified treating all returning volunteers as having high-risk exposures.)
For non-med-school faculty and staff – including those in the School of Public Health – the recommendation was almost the same. The policy says that they:
…should not participate in direct clinical care for 21 days following their return.
Note the rationale for the policy, which explicitly refers to:
…the potential to unwittingly acquire Ebola and place others in the Johns Hopkins community, including patients, at risk on return.
Clearly, JHU decided that asymptomatic returning Ebola volunteers represented a health risk. That did not keep the Dean of the Johns Hopkins School of Public Health from sending an anti-quarantine letter to Governor Christie on October 27, 2014, which claimed that quarantine:
…increases paranoia without materially protecting health.
That’s a disingenuous claim; to the extent that people were frightened or even paranoid about Ebola, a quarantine policy would surely constitute reassurance. It would diminish, not exacerbate, the paranoia.
The letter also included this falsehood:
I ask that you follow the current CDC guidelines, as we do for our faculty, staff or students who are returning from working in West Africa.
47. Some Ebola quarantine bottom lines:
47.1 Ebola quarantine is genuinely debatable. The fact that asymptomatic people rarely if ever transmit Ebola is the best argument against quarantine. The significant risk of sudden symptom onset and the likelihood that symptoms may be missed, ignored, denied, or misinterpreted are the best arguments for quarantine.
47.2 Public health professionals and their organizations claimed, en masse, that Ebola quarantine was not debatable, that Sound Science proved indisputably that quarantine proponents were ignorant or worse.
47.3 They did so in ways that were often dishonest and almost always disrespectful – and despite widespread quarantine-like policies within public health itself. Coincidentally or not, their advocacy served the cause of Democratic politics.
Zika Funding
![]() 48. I shouldn’t need to say this, but I suspect I do. As you listen to my final example, I want you to bear in mind that I am neither a Republican nor an abortion rights opponent. My daughter is a Planned Parenthood attorney, and I believe fervently in her work. I nonetheless intend to offer an extended critique of how I think public health has dishonestly and dishonorably sacrificed Zika funding advocacy to Democratic Party advocacy and Planned Parenthood advocacy.
48. I shouldn’t need to say this, but I suspect I do. As you listen to my final example, I want you to bear in mind that I am neither a Republican nor an abortion rights opponent. My daughter is a Planned Parenthood attorney, and I believe fervently in her work. I nonetheless intend to offer an extended critique of how I think public health has dishonestly and dishonorably sacrificed Zika funding advocacy to Democratic Party advocacy and Planned Parenthood advocacy.
Let me summarize where I’m going with a cartoon, one of many that blamed Republicans for the failure of Congress to fund Zika until late September. This one is from a U.S. News article with the incredibly alarmist title “The Plight of Generation Zika.” The message is clear, and explicitly political: Blame Zika on two villains, mosquitoes and Republicans.
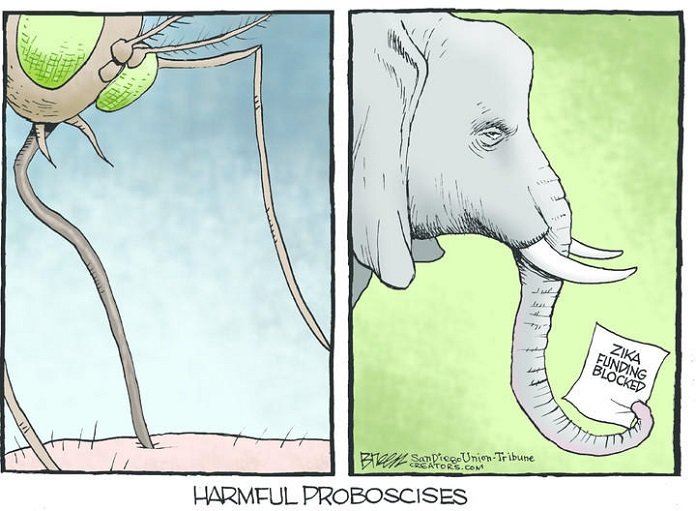
49. In the early months, from January till the end of March 2016, public health – especially CDC – was the main player in domestic news about Zika. CDC’s message was exactly right, based on what was known at the time:
- That pregnant travelers faced a serious risk if they traveled to Zika-affected places;
- That Puerto Rico was already a Zika-affected place where the risk to fetuses was substantial; and
- That everybody else – everybody in the continental U.S., whether pregnant or not – faced a very low risk because Zika transmission in the continental U.S. was expected to consist of small local outbreaks, following the pattern of dengue.
In CDC communication jargon, that was CDC’s “SOCO” – its “Single Overriding Communication Objective.” Among its overarching goals was to warn the American public (outside Puerto Rico) that there would probably be some microcephalic babies resulting from local Zika transmission, but not many, and to prepare the American public to take limited local Zika transmission and its inevitable victims in stride, without overreacting. Jody and I wrote a column praising CDC for excellent Zika risk communication so far.
50. Starting in early April, the CDC’s “Single Overriding Communication Objective” was itself overridden, by the White House, which articulated a new SOCO: that the continental U.S. faced a public health crisis because Zika transmission was expected to be widespread. I won’t take the time to share with you the long litany of quotes from the White House and Congressional Democrats about the widespread Zika disaster the continental United States was facing in the months ahead.
51. There is no question that Zika is frequently catastrophic to fetuses. The question was whether the number of fetuses threatened with this catastrophe constituted a major public health crisis. The answer for Brazil and many other countries was definitely yes. The answer for Puerto Rico was also definitely yes. So was the answer for pregnant U.S. travelers to Zika-affected places. The answer for everybody else in the continental U.S. was less clear.
Public health had had one answer. Its most likely scenario in January, February, and March was “limited local transmission.” Starting in early April, the White House voiced a very different answer. Its most likely scenario: a widespread outbreak and a catastrophic domestic public health crisis.
52. What has since transpired in south Florida looks closer to the CDC’s original SOCO than to the White House’s later SOCO, even though the number of local cases in south Florida is already higher than the Key West dengue outbreaks of 2009 and 2010, with no end in sight. It remains possible but unlikely that a widespread disaster in the continental U.S. awaits us in the months to come, that there will indeed be something like a “Generation Zika” throughout the country – as Peter Hotez has explicitly predicted and many others in government and public health have endlessly implied.
53. Starting in April, CDC (and Tony Fauci at NIH) continued to voice the “limited local transmission” SOCO, but less frequently and less loudly, most often deferring instead to the White House messaging. CDC even advanced the White House messaging in a variety of ways – most notably by replacing its preexisting map of places where the Zika-competent Aedes aegypti mosquito is prevalent in summer with new maps showing the estimated “potential range” (essentially where the insects could theoretically survive) of both Aedes aegypti and Aedes albopictus – a swath of parts of 30 states. (Imagine replacing a map of places that often have tornadoes with a map of places where a tornado is possible – and then basing your tornado preparedness, prevention, and response planning on the new map.)
Endless state and local health departments have cited the new CDC maps as part of their rationale for urging their citizens to take steps to “stop Zika” – steps like wearing insect repellant – even in places with no actual history of Aedes aegypti, let alone evidence of local transmission.
54. I don’t blame CDC and NIH much for toeing the White House line; that’s part of their job description. In fact, Dr. Fauci in particular drew on some of his extremely high credibility by continuing to go on Sunday interview shows to preach the old gospel of limited local transmission. I do, however, blame non-federal public health professionals – especially powerful ones – for going along with the new White House SOCO.
54.1 I assume some public health professionals didn’t notice the change.
54.2 Some public health professionals undoubtedly believed the change was a response to real changes in the situation. There were some real changes for the worse, most notably the discovery that sexual transmission wasn’t all that rare, and the growing body of evidence that microcephaly was the tip of the iceberg of Zika birth defects. Speaking at the White House, presumably under some pressure not to contradict the new White House SOCO, CDC’s Anne Schuchat conceded on April 11 that “Everything we look at with this virus seems to be a bit scarier than we initially thought.” But there’s a yawning chasm between “a bit scarier” and a national public health crisis.
54.3 And some public health professionals, I think, realized that the most likely scenario was being hyped and decided not to say so – maybe because they coveted Zika funding; maybe because they didn’t want to risk damage to their professional reputations by dissenting (despite Fauci calmly reiterating the old SOCO); maybe because they saw political value for the Democratic Party in the White House messaging.
55. Opinions may differ on why White House spokespeople promulgated a “crisis” vision of Zika’s most likely prevalence and impact in the continental U.S.
- Maybe they thought the experts were wrong and Zika was going to be much worse in the continental U.S. than the experts were claiming.
- Maybe they thought it was good risk communication to be extra-cautious, perhaps in order to arouse an apathetic public to a state of greater concern.
- But I believe the White House’s repeated use of words like “crisis,” “disaster,” and “widespread” with regard to Zika in the continental U.S. was aimed at the funding controversy already brewing in Congress by early April.
56. That controversy focused on whether the President’s request for $1.9 billion in emergency Zika funding should be passed. Republicans’ main objection was that the President and the Democrats didn’t want any offsets. They wanted $1.9 billion in “new money” – that is, money added to the deficit and the national debt rather than money reallocated from some other priority. As you know, the administration did eventually reallocate money, in several tranches from several pots, most notably from a budget appropriated during the Ebola epidemic and originally set aside for long-term public health infrastructure-building in West Africa. But at the time the administration was resisting any offsets, and the hyping of domestic Zika risk occurred in that context.
57. Two hypotheses are relevant here:
- That the White House was trying to motivate or pressure Republicans to pass Zika funding by emphasizing how bad Zika was likely to be in the continental U.S.
- That the White House was trying to set up Republicans to take the blame – that is, that in a crucial election season the White House wanted a Zika battle far more than it wanted a Zika budget.
58. I think there is a lot of evidence supporting the second hypothesis, but that’s not my argument here. All I want to note at this point is the consistency and zealousness with which public health organizations of all sorts endorsed the twofold White House position:
- That a federal Zika appropriation was desperately needed to address a domestic Zika public health crisis, not just in Puerto Rico but throughout the country.
- That it would be unconscionable to prioritize Zika over any other budget item, especially any other public health budget item; that the desperate need for Zika money must be met without reprioritizing – without (as virtually every op-ed and news release put it) “robbing Peter to pay Paul.” (Of course the “Peter” being robbed by “new money” is our grandchildren.)
In other contexts – antimicrobial resistance, for example – public health is highly critical of people’s tendency to optimize for current benefit and discount the needs of future generations. (This is a lesson environmentalists have tried to teach us vis-à-vis climate change and other long-term threats.) But when it came to Zika funding, public health was on the opposite side: Spend more now, and let our grandchildren pay later.
We have the opportunities to slow the spread of Zika into the United States over the next few months. If we’re successful, we could save dozens or even hundreds of infants from being born with devastating birth defects. We must act now…. But [public health agencies] should not have to fight Zika by raiding funds from other important agencies – shifting money from crisis to crisis will have us chasing our tail instead of organizing a holistic comprehensive response to these public health challenge. We don’t have the time that it took to learn about West Nile Virus. We have a short time in next few months to stop the Zika Virus from gaining a foothold….
McCabe also said:
We have a few short months to stop Zika from gaining a foothold in the U.S. If we don’t the consequences will be dire.
Also:
I understand the polarization of politics in this country; I don’t understand why children are being made the center of it. … We know what needs to be done, and it’s not stealing from Ebola to fix this disorder. Congress needs to do the right thing.
And talking to a Los Angeles Times reporter in late May:
This is very, very, very serious. We wouldn’t want L.A. to turn out to be ground zero for endemic Zika in the U.S.
58.2 March of Dimes was by no means alone. Here is the first paragraph of an American Public Health Association (APHA) April 5 letter ![]() to Congress:
to Congress:
The undersigned organizations committed to the health and wellbeing of our nation’s families and communities urge you in the strongest terms to immediately provide emergency supplemental funding to prepare for and respond to the Zika virus here in the United States. We also urge that Congress provide new funding rather than repurpose money from other high priority programs at the Centers for Disease Control and Prevention (CDC) and other federal agencies that ensure our health security and public health preparedness.
In other words, Zika is an emergency but not so much of an emergency that we should take money from any other public health activity, the way the Republicans want to do. Take it from our grandchildren, the way the Democrats want to do.
A June 28 APHA press release quoted Georges Benjamin, APHA President, as follows:
We’ve seen this coming from a mile away. There are nearly 1,000 cases in the U.S. already and it could get much more severe if we don’t get serious about slowing the outbreak immediately. We’re hopeful that Congress will put measures in place to stop the spread of Zika without compromising other public health safeguards.
In this short press release, APHA argues for funding Zika without offsets (at least without public health offsets) three different times.
I think it’s an absolute outrage that President Obama was forced to move Ebola money to the Zika response. … There will be another congressional hearing, and you’ll have poor mothers with their microcephalic babies testifying before Congress, and the public will ask, “How did you let this happen?”
The Zika virus has the potential to rapidly become a public-health emergency that poses a grave risk to patients….
It is imperative that the House and Senate reach an agreement without further delay; every day that goes by without an agreement is a day where more patients will be at risk of being exposed to the virus….
While developing a Zika response is critical, … Congress should exercise caution so that funding for other essential health initiatives is not placed at risk in order to fund the response.
59. Perhaps the most stunning example of this stance – that Zika funding is urgent but only the “right” sort of Zika funding is acceptable – is public health’s response to the Planned Parenthood rider.
59.1 I don’t want to get into the weeds of Congressional procedure here, but you need to know this much. First the Senate passed a $1.1 billion Zika bill that was all new money. Then the House passed a bill about half that size that was entirely offset. So a joint conference committee needed to come up with a compromise bill to be submitted for an up-or-down no-amendments vote in both Houses.
59.2 The conference committee bill was $1.1 billion (like the Senate bill), but it was about two-thirds offset and one-third new money. Republicans also inserted several riders into the conference committee bill. I want to focus on one of the riders, the one that got by far the most attention:
- It appropriated $95 million for social service block grants for Zika-related family planning – presumably mostly to help women not get pregnant in places where Zika is circulating.
- It specified that the $95 million could be spent only in places with “active or local transmission” – no state where only travelers were infected was eligible.
- Of the $95 million, it specified that at least $80 million must go to territories where transmission was worst – essentially, to Puerto Rico.
- Finally, it specified that all the money must go to hospitals, public health departments, Medicaid providers, and similar public organizations
59.3 The final provision was written in a way that probably would have excluded Planned Parenthood clinics. Given the other provisions, the impact would have been almost entirely on Profamilias, the Planned Parenthood affiliate in Puerto Rico, the territory for which most of the $95 million was earmarked – and especially on the two Profamilias clinics in San Juan, as opposed to its island-wide education facilities. (The education facilities do distribute condoms – but everyone agrees that avoiding Zika pregnancies in Puerto Rico pretty much requires prescribing the pill or the IUD, not just handing out condoms.)
59.4 Once Florida started documenting local transmission in the Miami area, the provision might have had a small effect on Planned Parenthood clinics in that state – and perhaps on Planned Parenthood clinics in other states that document local transmission in the future. But it’s basically about Puerto Rico.
60. Those are the facts: A bill that provided $1.1 billion for Zika had a provision that earmarked a $95 million family planning slice of that $1.1 billion for public agencies, creating a new Zika family planning pot mostly for Puerto Rico that probably would have excluded the Planned Parenthood affiliate in Puerto Rico.
61. That bill passed the House. It would have passed the Senate, except that Democrats filibustered it three times to keep it from coming up for a vote. They thus protected the President from having to choose between vetoing it (as he had threatened to do) and signing it.
62. Opinions differ on whether the Planned Parenthood rider was added to win much-needed right-wing Republican votes in the House or to deter Democratic votes in the Senate. Both hypotheses make sense.
62.1 Republicans on the conference committee saw a real need to offer their right wing a sop or two, given the size of the bill and the fact that it wasn’t completely offset.
62.2 But they might also have seen the value of fighting back in the blame game the Democrats had been playing for months. In the fight over whether Zika funding should be offset or added to the national debt, Democrats had successfully accused Republicans of putting a budgetary principle ahead of a public health emergency – as if that weren’t also symmetrically true in reverse for the Democrats. Now Republicans saw a chance to pass a Zika bill in the House that Democrats might be seduced into opposing in the Senate.
63. The White House, Congressional Democrats, and a shockingly large number of public health professionals had explicitly blamed the failure to pass Zika funding on Republican opposition to the $1.1 billion Zika bill the Senate had passed. They had said the House bill was too small and its offsets were unacceptable. Now the Republicans had their own $1.1 billion Zika bill – with a “poison pill” rider that most Democrats were unwilling to accept.
64. It would be going too far to claim that major public health organizations explicitly opposed the conference committee’s Zika bill because it included the Planned Parenthood rider, and explicitly sided with Democrats’ decision to filibuster the bill.
- Lots of Democratic politicians said the rider was unconscionable, that it “forced” Democrats to vote against the bill – thus continuing to blame Republicans for preventing the passage of federal Zika funding.
- Lots of newspaper editorials said the same thing.
- Lots of individual clinicians and public health professionals said the same thing.
- Lots of women’s health advocates and bloggers said the same thing, in much more hot-tempered language.
- Planned Parenthood itself went furthest of all. In late June, Planned Parenthood wrote to all Senate offices opposing the bill, warning Republicans and assuring Democrats that:
Try telling that to all the poor exposed women in Puerto Rico in the summer of 2016.…a vote against this bill will be seen as a vote for women’s health care.
But the sin of the major public health organizations vis-à-vis this Zika bill wasn’t active opposition. It was silence. Silence or intentional vagueness.
To the best of my knowledge, not one public health organization or leader publicly advocated passage of the bill. Not one. Remember, this was a conference committee bill, meant to reconcile differences in separate bills previously passed by the House and Senate. Under Congressional rules, it couldn’t be amended, and no alternative bill could be introduced. (They eventually got around that with a Zika provision in the continuing resolution that kept the government going, not a free-standing Zika bill.) For the immediate future, the only option was an up-or-down vote on the bill in the form it had emerged from the conference committee … Planned Parenthood rider and all.
I can’t find a major national public health organization or even an individual public health professional of any renown who said: “Vote it up, for God’s sake!”
Public health organizations and leadership individuals had advocated strongly for the Senate bill. They had advocated strongly against the House bill, because it was smaller and had Ebola offsets (and Obamacare offsets). When it came to the conference committee bill with the Planned Parenthood rider, they either went silent or retreated into vague wishfulness, urging Congress to end its quarreling and its paralysis, and pass some Zika bill. But they never, ever urged passage of the Zika bill with the Planned Parenthood poison pill, the one that was pending before the Senate after having handily passed the House.
65. You know the end of the story. The Democrats won the blame game. The Republican effort to shift the blame failed, and several surveys showed that most of the American public still blamed Republicans for the absence of federal Zika funding. The issue had become a potent weapon for Democrats in several important races, especially Marco Rubio’s Senate race in Florida. And so the Republicans caved, and in the final days of September they gave the Democrats what they wanted: a $1.1 billion Zika provision in the continuing resolution that has minimal offsets and no Planned Parenthood poison pill.
66. Was all this political spy-versus-spy game-playing on the part of both Democrats and Republicans disreputable?
66.1 For sure, it was disreputable if you believe what both political parties claimed to believe – and what public health professionals mostly claimed to believe as well – that Zika was a national public health emergency (not just in Puerto Rico) and that Zika funding was therefore an urgent, even desperate need. (The renowned D.A. Henderson dissented; shortly before his death, he said he thought Zika was being overhyped, especially as regards the continental U.S.)
66.2 On the other hand, if you believe Zika is somewhere down in the middle of a reasonable list of public health threats in the continental U.S., and if you believe the 2016 election is one of the most important elections in recent decades, then you could make a case that politicians in both parties were just doing their jobs when they used Zika as a pawn in an overwhelmingly more important chess game.
67. I am more bothered when I see public health professionals using Zika as a pawn in that chess game, and always on the same side. Here’s what’s amazing to me. I know of no public health organization or even renowned individual professional that dissented publicly from Democratic Party orthodoxy on the Planned Parenthood rider, urging Senate Democrats to swallow the damn poison pill (largely symbolic, affecting mostly two Planned Parenthood full-service medical clinics in San Juan, Puerto Rico) for the sake of that desperately needed $1.1 billion in Zika funding.
68. Many of the statements coming out of politicians, bloggers, and editorialists were explicitly dishonest or ignorant.
68.1 Many talked about the “defunding” of Planned Parenthood – as if not giving new money to Planned Parenthood, which already receives about $500 million a year in federal funds, constituted “defunding.”
68.2 Others went further and falsely claimed that Congressional Republicans were balking at appropriating any money for Zika family planning – when the reality was that Democrats were balking at $95 million in new Zika family planning money because probably none of it would flow to Profamilias, the Planned Parenthood Puerto Rico affiliate.
69. But what I find most astounding and disquieting isn’t just the dishonesty of so much messaging against the Planned Parenthood poison pill. It’s the goal on behalf of which that dishonesty was deployed – to prevent passage of the only Zika funding bill on the table, a bill that had passed the House and would definitely have passed the Senate if not for three Democratic filibusters. The goal was to stop the only Zika funding bill that was “good to go” – all the while urgently demanding a Zika funding bill – and thus to perpetuate the narrative that it was Republicans preventing the passage of a Zika bill, first by rejecting the “good” $1.1 billion Zika bill that came out of the Senate and then by promulgating an “unworthy,” poison-pill-laden $1.1 billion Zika bill that came out of the conference committee.
70. Commentator after commentator articulated the truth that taking a mostly symbolic stand against Planned Parenthood, as Republicans wanted to do, is not an acceptable reason to deprive the country of urgently and desperately needed federal Zika funding. To the best of my knowledge, nobody in the mainstream media and nobody in public health articulated the equally obvious truth that taking a mostly symbolic stand on behalf of Planned Parenthood, as Democrats wanted to do, is also not an acceptable reason to deprive the country of urgently and desperately needed federal Zika funding.
71. Alternatively, we could speculate that public health might have been thinking long-term – that perhaps the public health leadership foresaw that the Democrats would win the blame game and eventually get their $1.1 billion without any poison pills. But under that scenario we also have to conclude that public health thought waiting a few more months for Zika money was not too high a price to pay for ridding the Zika bill of that Planned Parenthood rider. It is hard to reconcile acceptance of the delay with public health’s endlessly reiterated claim that the need for federal Zika money was urgent, even desperate.
72. I see no way a public health profession genuinely desperate for Zika funding could prefer no funding at all (at least for several months) to the bill that Senate Democrats filibustered. I am forced to the conclusion that the public health profession made an en masse choice to prioritize Democratic Party allegiance and Planned Parenthood allegiance over Zika funding urgency, all the while claiming that Congress’s Zika funding failure was a public health and moral travesty – and not quite claiming but clearly implying that that travesty was perpetrated by Republicans.
Let me repeat: I am forced to the conclusion that the public health profession made an en masse choice to prioritize Democratic Party allegiance and Planned Parenthood allegiance over Zika funding urgency, all the while claiming that Congress’s Zika funding failure was a public health and moral travesty – and not quite claiming but clearly implying that that travesty was perpetrated by Republicans.
73. My wife and colleague Jody Lanard calls this whole Zika funding story “King Solomon Weeps.” Both the Democrats and the Republicans wanted to cut the baby in half rather than compromise to get a Zika bill passed quickly. And virtually the entirety of the public health profession, if it took a stand on Zika funding at all, implicitly but clearly held Republicans but not Democrats responsible for that failure to compromise.
The position of the public health mainstream was that Zika funding is essential. And that funding is urgent; position statement after position statement warned that “the window is closing.” But according to the public health mainstream, Zika funding was not so essential that any other public health budget category should suffer. Moreover, it was not so essential, or so urgent, that Congress should pay the price of a largely symbolic insult to the Planned Parenthood Puerto Rico affiliate, Profamilias. Better no Zika bill than that Zika bill!
74. If you believe that Zika is a domestic public health crisis – or even if you believe that Zika is important enough that federal funding some months ago would have done real good, that funding last spring or summer could have made a difference compared to funding this fall – then I think you must also believe that public health had both an opportunity and an obligation to advocate for passage of the Zika bill that came out of the conference committee, notwithstanding the Planned Parenthood rider.
Instead, the public health mainstream allied with the Democratic Party’s highly successful blame game. It was complicit in the fiction that Republicans were unilaterally responsible for the failure of Congress to fund the U.S. Zika response. Or to put the matter differently, it was complicit in the decision to prioritize politics over public health.
Conclusion
75.1 Public health is a Guild. The leadership is often dishonest – often for altruistic reasons, sometimes for self-serving or political reasons. The followers are often deceived, as is the public.
75.2 I am no longer confident that the dishonesty of public health is undermining its credibility. I worry that it may, sooner or later. I believe it should.
- OPV – dishonesty motivated mostly by altruism.
- MMR – dishonesty motivated largely by logistical convenience and pridefulness.
- Ebola quarantine and Zika funding – dishonesty motivated largely by political allegiances.
75.4 In all four of these cases, disrespect for the public or segments of the public has accompanied the dishonesty.
75.5 As consumers of public health information, I urge you to listen skeptically. And as providers of public health information, I urge you to consider carefully to what extent you are comfortable being part of the conspiracy and to what extent you are willing to be branded an iconoclast instead.
My wife and colleague Jody Lanard contributed much of the documentation for this presentation.
Copyright © 2016 by Peter M. Sandman
